Parkinson’s disease psychosis (PDP) is a common neuropsychiatric condition that manifests in patients following a primary diagnosis of Parkinson’s disease (PD). Over half of patients diagnosed with PD experience PDP during the course of their disease.1,2
Diagnostic criteria for PDP have been developed by the US-based National Institute of Neurological Disorders and Stroke (NINDS)/National Institute of Mental Health (NIMH).3 These criteria identify PDP cases as patients who have a prior diagnosis of PD who experience at least one of the four characteristic neuropsychiatric symptoms (i.e., illusions, false sense of presence, hallucinations and/or delusions) that persist for at least one month and cannot be attributed to other causes or diagnoses, such as substance use, schizophrenia, or bipolar disorder.
The strategy for managing symptoms of psychosis in patients with PD typically include general measures (e.g., re-establishing circadian rhythms and normal-level sensory inputs), treatment of specific triggers (e.g., infections, dehydration, chemical imbalances), adjustment of PD medications, use of cholinesterase inhibitors for those with cognitive impairment, and treatment with antipsychotics when symptoms are no longer manageable with the other approaches.4 Guidelines from European healthcare authorities that cover the management of PD include recommendations for managing the symptoms of PDP. These guidelines generally recommend withdrawal of add-on medications suspected to have triggered the symptoms of psychosis (e.g., anticholinergics, selegiline, amantadine) as the initial intervention. If symptoms of psychosis persist, the next step is to adjust the dosage of dopaminergic PD medications in a standardised manner.5–7 If adjustment of dopaminergic medications does not yield satisfactory results, guidelines recommend the use of atypical antipsychotic agents, usually clozapine and quetiapine, as a subsequent step.5–10
In clinical practice, clozapine and quetiapine are generally withheld until there is significant quality-of-life (QoL) decline.11 Although clozapine is considered more effective than quetiapine for managing symptoms of PDP and is licensed for the treatment of PDP in the EU, use of the drug requires intensive patient monitoring due to the risk of serious side effects including agranulocytosis and myocarditis.12,13 Quetiapine is not licensed for the treatment of PDP despite being listed as a therapeutic option in guidelines.5–8,14 However, data from double-blind, randomized controlled trials evaluating quetiapine in patients with PDP have been mixed,13 with four studies reporting no significant improvement in symptoms of psychosis over placebo,15–18 and one study reporting a significant decrease in hallucinations.19 A new atypical antipsychotic, pimavanserin, received regulatory approval in the US in April 2016 for the treatment of hallucinations and delusions associated with PDP.20 However, pimavanserin is not yet available in the EU.
A survey and patient chart review were conducted with neurologists in France, Germany, Italy, Spain and the UK (collectively the EU-5) to understand the epidemiology and patterns of care and treatment for PDP in Europe. The current report describes trends in the setting of care and referral patterns for PDP from the perspective of neurologists, as well as diagnosis and treatment patterns among patients whose symptoms of psychosis require management.
Methods
Survey design
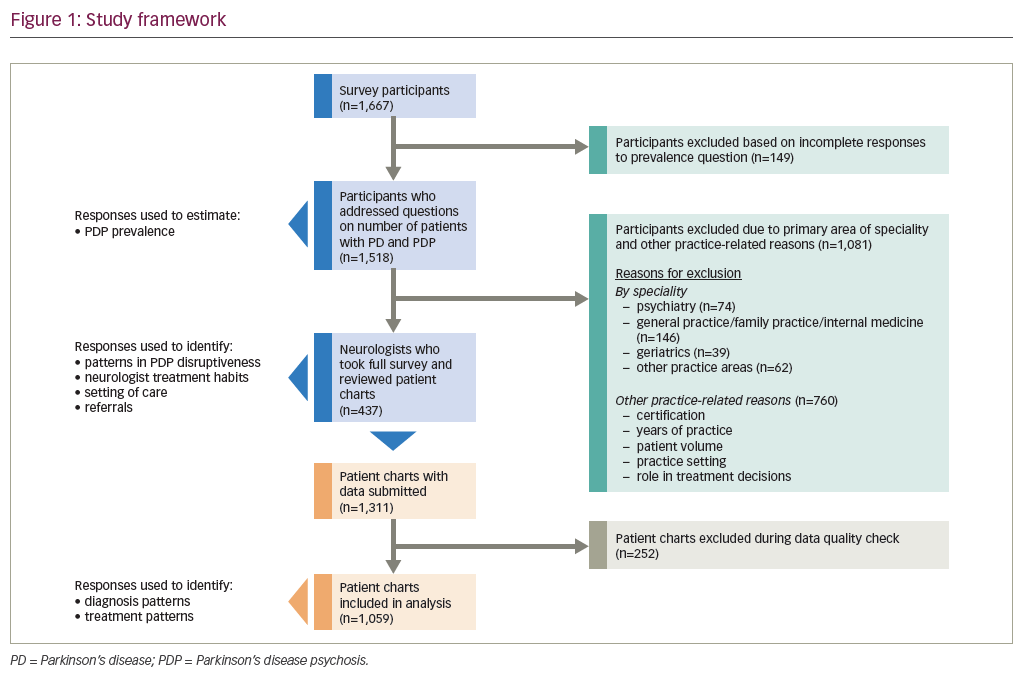
An online survey that included patient chart reviews was developed and targeted to medical practitioner specialists in the EU-5 nations between 21 May 2015 and 24 June 2015 as part of a broader study to address evidence gaps related to PDP epidemiology and treatment patterns. The survey was targeted to medical practitioners in the neurologist specialty based on preliminary qualitative research identifying the group as the key providers of care to patients with PD (unpublished findings). The study framework is presented in Figure 1. Details on overall survey design and epidemiological findings are described in a companion report.21
The patient chart review component of the survey requested anonymised data from three patients diagnosed with PDP who the surveyed neurologist had seen during the past 12 months, specifically for PD-associated motor and/or neuropsychiatric symptoms. Neurologists were provided with the criteria for patient chart selection as well as instructions on randomizing the selection process.
Surveyed neurologists were instructed to select three patient records that included the entire treatment history from the time the patient presented with symptoms of PDP. Records were required to have the chronological ordering of treatments received by the patient to manage symptoms of PDP. However, specific dates associated with the initial diagnosis of PD, the onset of PDP symptoms and the initiation of treatment for PDP-associated symptoms were not required for a valid patient record. For the three records, neurologists were instructed to select one record from a patient currently being treated with an antipsychotic, one record from a patient currently being treated with either an antipsychotic or an anti-dementia agent, and one record from a patient currently being managed with modification of PD medications alone. Surveyed neurologists who managed patients with PDP in multiple settings of care were also instructed to check that the three selected records encompassed at least one patient from each setting. These selection criteria were designed to focus the chart review on records from patients who are being actively managed for symptoms of PDP and to control for potential differences in treatment habits by setting of care. For the selection of records, surveyed neurologists were also instructed to exclude records from patients who have also been diagnosed with schizophrenia, schizo-affective disorder or bipolar disorder.
BluePrint Research Group, an independent market research firm commissioned by ACADIA Pharmaceuticals Inc., conducted the survey in compliance with data protection legislation and privacy laws, and the codes of conduct of the Market Research Society (MRS) and British Healthcare Business Intelligence Association (BHBIA).
Data analysis
Survey results were provided to investigators at Analysis Group in an anonymised aggregated dataset, and analysed using Microsoft Excel 2016 and SAS 9.4.
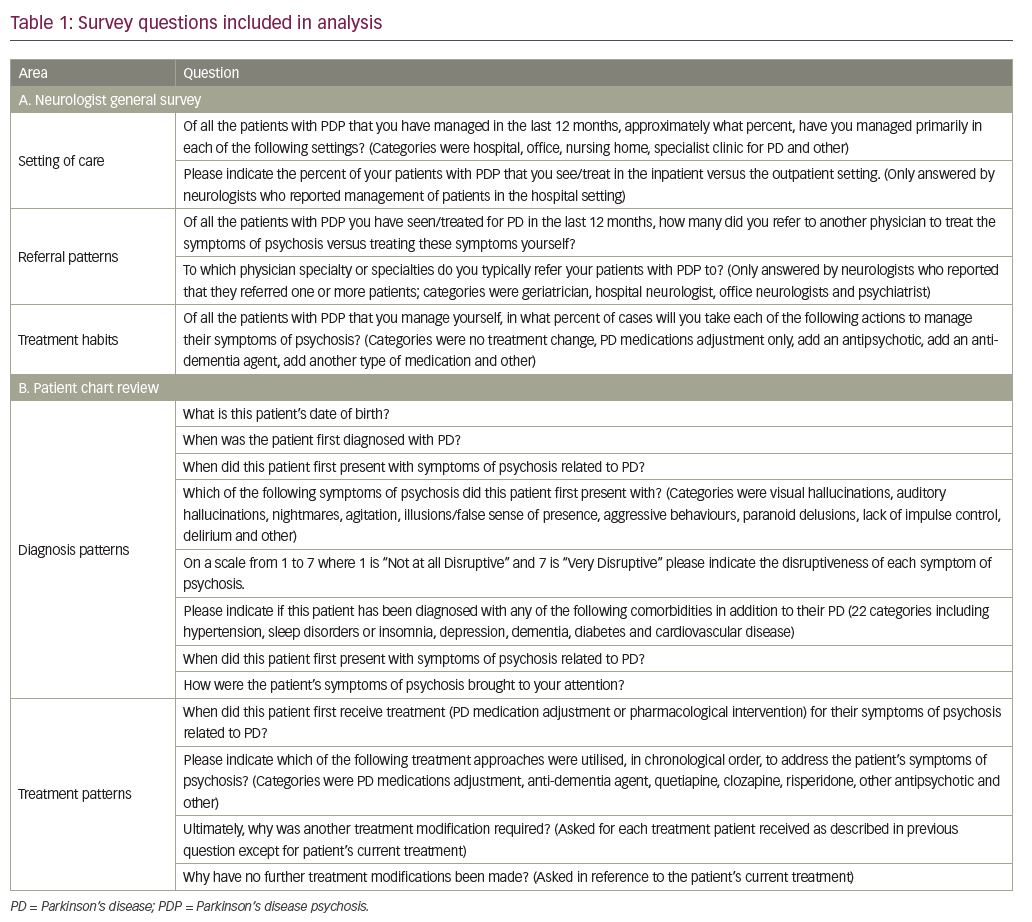
Survey questions included in the current analysis are presented in Table 1.
Individual responses to questions used to describe country-specific trends were weighted based on self-reported numbers of patients who had their PDP symptoms directly managed by the surveyed neurologists. Due to the selection criteria for patient charts, responses in the patient chart review segment on treatment patterns were weighted based on the self-reported patient numbers and estimated usage frequencies for various interventions across all patients with PDP managed by the surveyed neurologists. Each weighted response in the treatment patterns section was also adjusted based on the number of patient records from a surveyed neurologist that were applicable to a particular question. Weighting was applied prior to frequency calculations.
Reported frequencies were calculated by dividing the total number of specific responses to a particular survey question by the total number of responses received for that question. Reported frequencies were also expressed as percentages. Information on the patient’s date of birth and the dates associated with initial PD diagnosis, PDP symptom onset and initiation of treatment for PDP-associated symptoms were used to calculate the patient’s age at the time of PDP presentation, the length of time between PD diagnosis and onset of PDP symptoms, and the length of time between PDP presentation and treatment of symptoms.
Results
Survey metrics
Responses from a subset of 437 neurologists, along with chart reviews covering 1,311 patients were collected. Only 1,059 patient charts were included in the chart review analysis as information from 252 submitted records failed a subsequent quality check for inclusion. The majority of the excluded records (n=246) failed the quality check due to indicators that suggest the instructions for patient records selection were not followed (e.g., the most recent treatment on record was not PD medications adjustment, an anti-dementia agent or an antipsychotic, or there was a mismatch between the type of record submitted as indicated by the survey participant and the latest treatment for the patient listed in the record). A small number of records (n=6) were removed due to suspected fabrication of responses (e.g., patient treatment history included every selectable option). Full survey metrics are described in the companion report.21
A. Neurologist general survey estimates
Setting of Care
Country-specific breakdowns of the setting of care and referral patterns are presented in Figure 2.
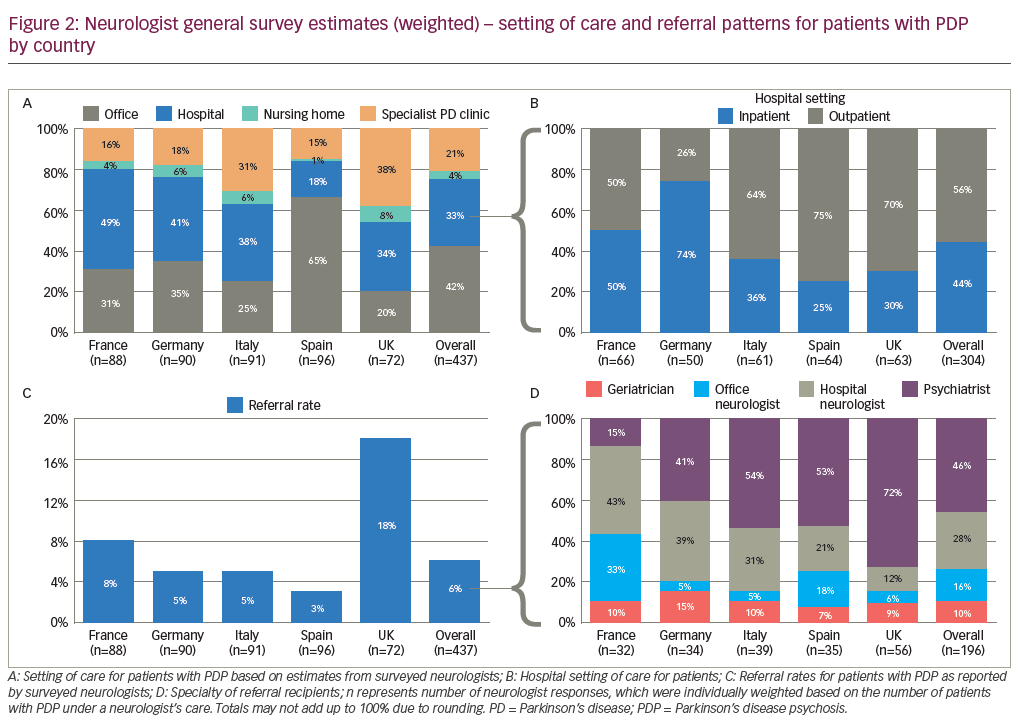
Weighted analyses of responses from the 437 surveyed neurologists in the EU-5 suggest that the majority manage their patients with PDP in the office (42%) and hospital (33%) settings. In addition, neurologists across the EU-5 reported managing approximately one-quarter of their patients with PDP in specialist PD clinic (21%) or nursing home (4%) settings. Neurologists in the UK reported the specialist PD clinic as the most common setting of care (38%) while neurologists in Spain reported managing the majority of their patients with PDP in the office setting (65%).
The hospital was the most frequently reported setting of care for patients with PDP among neurologists in France (49%), Germany (41%) and Italy (38%). Neurologists in Germany reported managing the majority of hospital patients with PDP in the inpatient setting (74%). Conversely, neurologists in Spain, Italy and the UK reported managing the majority of their hospital patients with PDP in the outpatient setting (75%, 70%, and 64%, respectively). In France, neurologists reported an even split in the management of patients with PDP in the inpatient and outpatient settings. Overall, surveyed neurologists across the EU-5 reported approximately 56% of their patients with PDP managed in the hospital setting receive care in the outpatient setting.
Neurologist referral patterns
The surveyed neurologists reported referring approximately 6% of their patients to another medical practitioner for management of PDP symptoms, and the rate ranged from 3% for neurologists in Spain to 18% for those in the UK. The most common recipients of these referrals across the five countries were psychiatrists (46%) followed by hospital neurologists (28%). Notable country-specific trends were observed in the UK, where an estimated 72% of referrals were to psychiatrists, and in France, where referrals to other neurologists who practised in the hospital (43%) and office (33%) settings appeared most common.
Neurologist treatment habits
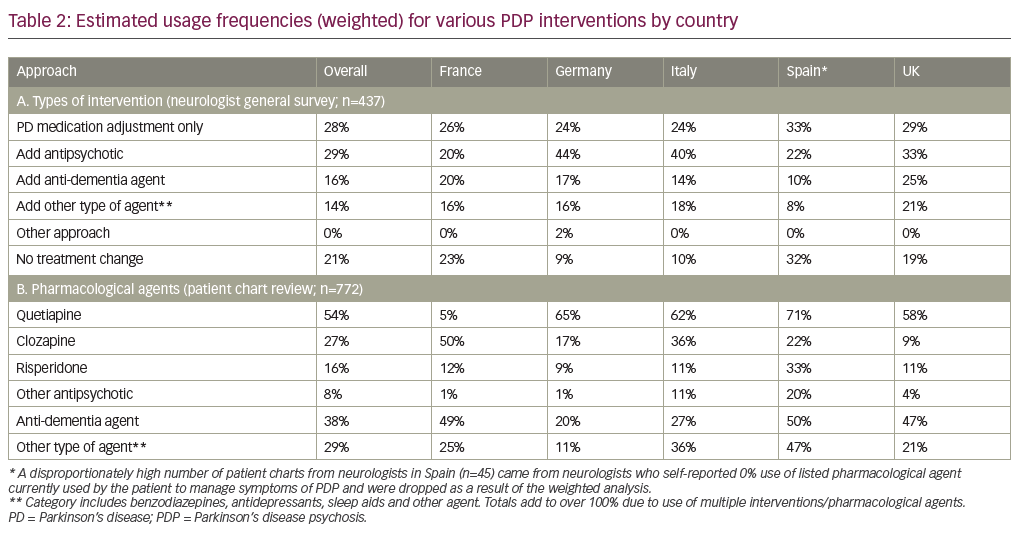
Neurologist self-reported estimated usage frequencies of various interventions for symptoms of PDP are presented in Table 2A.
Across the five countries, the most frequently (≥25%) reported interventions used to manage symptoms of PDP were antipsychotics (29%) and PD medications adjustment (28%). The self-reported frequency of use of antipsychotics for management of PDP symptoms ranged from 20% among neurologists in France to 44% among those based in Germany. These self-reported estimated usage frequencies of the various interventions were used to weight data on treatment patterns obtained from the patient chart review.
B. Neurologist diagnosis and treatment patterns from patient chart review
Diagnosis patterns
Unless otherwise noted, results from the chart review are based on neurologist-provided responses to questions about information contained in 1,059 patient charts. Unweighted analysis of results from the patient chart review suggested the majority of patients (70%) with PDP presented with symptoms four or more years after the initial diagnosis of PD. Among the 506 patient charts for which relevant chronological data were available, 38% of cases presented with symptoms ≥4 and <8 years after initial PD diagnosis, and another 33% presented with symptoms ≥8 years after diagnosis. The average age of PDP presentation was 71 years based on the 784 patient charts where such data were available. The most common (≥25%) symptoms of psychosis at initial presentation of PDP were visual hallucinations (50%), agitation (39%) and illusions/false sense of presence (28%). Neurologists rated these three symptoms as moderately disruptive in 68–77% of cases and very disruptive in 13–29% of cases. The most common (≥25%) comorbidities reported from the patient chart review were hypertension (41%), sleep disorders or insomnia (30%), depression (27%) and dementia (26%). Notably, cardiovascular disease was reported in 14% of cases. Totals added up to over 100% as surveyed neurologists were able to report multiple symptoms and comorbidities in patients.
Detailed data on symptoms and comorbidities are presented in Supplementary Figures S1–S3.
Caregivers were the most common party to bring a patient’s symptoms of PDP to the attention of the surveyed neurologist. Weighted country-specific rates were 84% in Italy, 72% in Spain, 71% in France, 63% in the UK, 56% in Germany and 70% overall. Overall, patients themselves were the next most common party to bring symptoms of PDP to the neurologist’s attention (30%), with weighted country-specific rates of 38% for the UK, 35% for France, 29% for Spain, 27% for Italy and 24% for Germany. Notably, 27% of the patients in France also had their symptoms of PDP initially reported to the neurologist by a referring medical practitioner and 30% of the patients in Germany had their symptoms uncovered directly by the surveyed neurologist. Totals added up to over 100% as surveyed neurologists cited multiple sources from which a patient’s symptoms of PDP were brought to his or her attention.
Treatment patterns
Weighted analysis of the 772 patient charts, for which relevant chronological data were available, estimated that 68% of patients across the EU-5 began treatment for PDP less than a month after initial presentation of symptoms with another 20% starting treatment within 1–4 months. Country-specific rates for starting treatment within less than 1 month or within 1–4 months were 80% and 10% in Spain, 73% and 15% in Germany, 63% and 28% in France, 62% and 28% in Italy, and 53% and 25% in the UK, respectively. Detailed country-specific breakdowns on the frequencies of use for pharmacological agents are presented in Table 2B.
Overall, the weighted analysis showed that the most frequently prescribed pharmacological agent for managing symptoms of PDP regardless of line of therapy was quetiapine (54%), followed by anti-dementia agents (38%), other non-antipsychotic/non-anti-dementia agents (29%) and clozapine (27%). Importantly, despite evidence and guideline recommendations against the use of risperidone to manage PDP,6,22 an estimated 16% of patients had been prescribed the atypical antipsychotic at some point during the course of care. The most frequently prescribed anti-dementia agents across the EU-5 were rivastigmine (62%), memantine (16%) and donepezil (15%) based on a weighted analysis of 331 patient charts. Of these 331 charts, 171 (52%) were from patients with comorbid dementia. The most frequently prescribed non-antipsychotic/non-anti-dementia agents across the EU-5 were benzodiazepines (51%), antidepressants (39%) and sleep aids (19%) based on a weighted analysis of 198 patient charts. Detailed country-specific breakdowns on the frequencies of use for typical interventions by line of intervention are presented in Table 3.
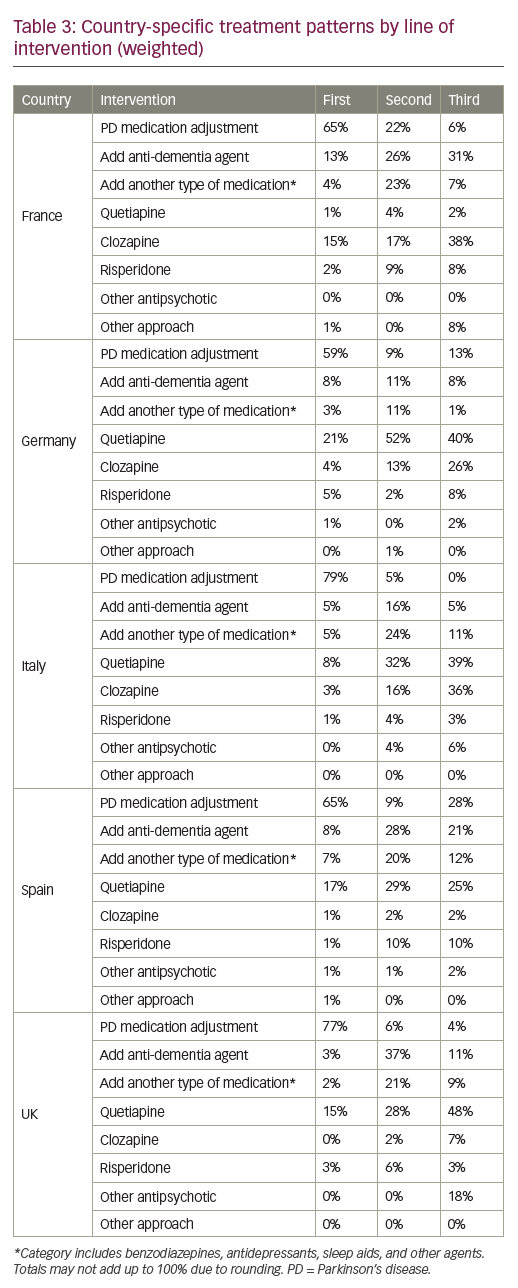
Weighted analysis of treatment history data from the 1,059 patient charts showed that PD medications adjustment was the most common initial intervention for managing PDP (68%), followed by the use of an atypical antipsychotic (19%), typically quetiapine. The estimated frequency at which PD medication adjustment was used as a first-line intervention ranged from 59% in Germany to 79% in Italy. Frequently reported approaches to PD medication adjustment were dose modification of carbidopa and/or levodopa (61%, n=645) or dose modification (46%) or discontinuation (33%) of dopamine agonists (n=426). In the select cases where a patient’s treatment regimen included anticholinergic agents (n=41) medication adjustment generally involved discontinuation of the agent (77%). Overall, the next most common initial intervention for managing PDP was quetiapine (13%), with estimated frequencies of use at 21% in Germany, 17% in Spain, 15% in the UK, 8% in Italy and 1% in France. In France, the estimated frequency of use for clozapine as the initial intervention for managing PDP was 15%. First-line usage frequencies for clozapine in the remaining countries were estimated at 4% in Germany, 3% in Italy and 1% in Spain. No clozapine usage was reported in the first-line setting among patients managed by neurologists in the UK. As a class, anti-dementia agents were the third most common intervention used in the first-line setting to manage PDP, with frequencies of use ranging from 3% in the UK to 13% in France.
Overall, the most common second-line intervention for management of PDP was quetiapine (30%), with frequencies of use estimated at 52% in Germany, 32% in Italy, 29% in Spain, 28% in the UK and 4% in France. The next most common second-line interventions for PDP were anti-dementia agents.
In the third-line setting, quetiapine remains the most frequently used option overall (31%), with frequencies of use estimated at 48% in the UK, 40% in Germany, 39% in Italy, 25% in Spain and 2% in France. The next most common third-line interventions for managing PDP were clozapine followed by anti-dementia agents.
Notably, the management of patients with PDP in France appears to be an outlier when compared to that of other EU-5 nations. The most common second-line intervention for patients in France was an anti-dementia agent (26%) and the most common third-line intervention was clozapine (38%).
Across the five countries, the most commonly (≥25%) cited reasons for the patient requiring a subsequent treatment modification after adjustment of PD medications were lack of control of psychosis (73%) or negative impact on motor function (26%) based on an analysis of 449 patient charts. Similar trends were reported from patients requiring treatment modification after receiving quetiapine or anti-dementia agents. Adequate control of symptoms of psychosis (59–77%) and waiting for a treatment response (21–40%) were the two most commonly cited reasons for patients not having their current treatment regimen modified. Detailed data on reasons for modification to, or maintenance of, treatment regimens are presented in Supplementary Tables S1–S2.
Discussion
The current report describes trends related to the care and treatment of PDP in major EU nations based on responses from 437 surveyed neurologists and information they provided from 1,059 patient charts. Our analysis focused on identifying trends in the setting of care and patient referrals as well as in the diagnosis and treatment of PDP. Prevalence patterns for PDP in the EU-5 based on an analysis of the same dataset are described in a companion report.21
Symptoms of PDP manifest in the majority of patients with PD during the course of disease1,2 and can magnify the burden of disease on both the patient and their respective caregivers.23–26 Treatment guidelines published by European healthcare authorities generally recommend adjustment of PD medications as an initial intervention step to manage PDP symptoms and mention quetiapine and clozapine as potential options for subsequent lines of intervention.5,7–10
In the EU nations covered in our survey, we observed that symptoms of PDP typically manifest in patients over the age of 70 year and that patients generally have their symptoms managed in office or hospital settings. Neurologists in Germany reported the highest rate of inpatient care for patients with PDP managed in the hospital setting, while those in Spain reported the lowest rate. Elucidating the underlying drivers behind these country-specific differences in setting of care is a potential area for future research.
The most commonly reported PDP-associated symptoms at presentation were visual hallucinations, agitation and illusions/false sense of presence. Caregivers were often the ones to bring a patient’s PDP symptoms to the neurologist’s attention. Notably, neurologists described initial symptoms of PDP as moderately disruptive or very disruptive in over 85% of cases included in the patient chart review. In contrast, the companion report on PDP prevalence patterns noted that these same neurologists estimate 53% of their patients with PDP have disruptive symptoms. The figure in the companion report is based on neurologist estimates of current PDP cases with disruptive symptoms across their respective patient pools, rather than symptoms at presentation.21 It also included patients managed with currently available treatments for PDP as well as patients not currently on treatment for symptoms of PDP. The rate reported in the companion report also suggests a need for more effective interventions for PDP given that surveyed neurologists estimate approximately half of the patients with PDP under their care have disruptive symptoms.
The results from our study suggest clinical management of PDP in the EU-5 nations is mostly aligned with published guidelines in the first-line setting, but suggests there is considerable country-to-country variability in the treatments patients receive in subsequent lines of intervention. Our analysis of treatment history data showed that adjustment of PD medications was applied to the majority of patients in the first-line setting, although quetiapine was also frequently used in the first-line setting among patients managed in Germany. Despite not being licensed in the indication, our analysis of patient treatment histories suggests quetiapine is the most frequently used antipsychotic for managing PDP in four of the EU-5 nations, with France being the exception. This observation is not unexpected as the most recent guideline update from the UK’s National Institute for Health and Care Excellence published in July 2017, notes that although clozapine has superior efficacy to quetiapine, the former is not practical for routine first-line use due to the need for frequent patient monitoring for adverse events.5 In France, clozapine appears to be largely preferred over quetiapine as the antipsychotic of choice for managing PDP. The observation is in alignment with guidelines published in June 2014 by France’s national health authority, which mentions clozapine, but not quetiapine, as a treatment option for symptoms of psychosis.9 However, it is also important to note that the survey was conducted in mid-2015 and treatment patterns in the country may have since evolved. Generic formulations of quetiapine and parallel importations of the drug have been authorized in France since the survey was conducted, although reimbursement remains restricted to licensed indications. Furthermore, the French Transparency Commission has also recently recommended the removal of anti-dementia agents from the list of reimbursed drugs for the management of dementia in patients with PD or Alzheimer’s disease, although the country’s healthcare authority did not implement the recommendation.27
In addition to atypical antipsychotics, we also observed frequent use of anti-dementia agents, as well as other non-antipsychotic/non-anti-dementia agents in the second- and third-line settings. The observed frequencies of the use of these various interventions in the second and third line, suggests that best standard of care for PDP, following PD medication adjustment, may not be well defined or that there is a lack of options with favourable risk–benefit profiles. The frequent use of anti-dementia agents may have been driven, in part, by comorbid dementia, as approximately half of the charts from patients with PDP who received anti-dementia agents during their course of care also reported the comorbidity. However, data from clinical trials of anti-dementia agents in the PD setting have been mixed, with some studies reporting a decrease in hallucinations,28,29 and others reporting no improvement in neuropsychiatric symptoms.30–32 We also observed, from our weighted analysis, that an estimated 16% of patients receiving treatment for PDP have been prescribed risperidone at some point during their course of care. The observation is a potential point of concern in the clinical management of PDP because risperidone is known to exacerbate PD motor symptoms, increase mortality risk in elderly patients with dementia (a common comorbidity among patients with PD), has known interactions with other atypical antipsychotics and is generally not recommended for use in patients with PD.6,22 These observations together suggest there is a need for new therapies with improved therapeutic and safety profiles to manage the symptoms of PDP.
It is important to note that the reported frequencies in the current study are based on data entered by neurologists as part of an online survey and patient chart review, and are retrospective by nature. Referral patterns and treatment habits are self-reported estimates based on the memory of the surveyed neurologist and are subject to bias. Treatment patterns for PDP was an area of focus for the current study and instructions provided for selecting patient charts included criteria to enrich for patients who were currently receiving treatment to manage symptoms of PDP. The approach may have captured a subset of PDP cases that are more severe or advanced, and may not be a representative subset of the patients currently managed by surveyed neurologists. Data weighting was applied to address this limitation in study design. The analysis of treatment history data from patient charts provided by neurologists in Spain may be most heavily affected as a disproportionately high number of neurologists in the country who may have reported low or no use of antipsychotics to treat symptoms of PDP but still included charts from patients currently being treated with such agents. This latter observation may be driven by a special prescription fulfilment process in Spain, whereby prescriptions for certain drugs, including atypical antipsychotics prescribed to elderly patients, must be validated by a medical inspector prior to fulfilment. In addition, the chart review did not include patients with PDP who are not on treatment for symptoms of psychosis. Thus, the extent to which the reported trends in the diagnosis of PDP apply to such patients is unclear. Moreover, a question from the patient chart review requested an assessment of symptom severity, which includes a degree of subjectivity. Furthermore, the majority of patient charts included in our current analysis lacked the chronological data needed to calculate the patient’s age at the time of PDP presentation, the length of time between PD diagnosis and onset of PDP symptoms, and the length of time between PDP presentation and treatment of symptoms. Prior literature on the average age and time to onset of PDP are limited. In the longitudinal study in Norwegian patients, the average age of the study cohort at onset of PD was approximately 65 years, and PDP developed an average of 13 years after onset of PD motor symptoms (range: 2.2–25.1 years) in the subset of patients who entered the study prior to PDP onset (n=67).2 Reasonable efforts were made during the survey design, targeting and analysis steps to preserve the integrity of the collected data, with a data curation step that included removal of patient charts where the most recent treatment for PDP was not adjustment of PD medication, an antipsychotic or an anti-dementia agent.
Conclusion
The current report provides a resource for understanding the clinical management of PDP across the EU-5 nations and for comparing differences in clinical practice among countries from the neurologist’s perspective. The observed patterns of care show there is significant variability in the choice for subsequent lines of intervention used to manage PDP following PD medication adjustment, suggesting the standard of care for subsequent lines of intervention may not be well defined. Future research directions could include assessing patterns of care stratified by PDP case severity and select comorbidities, and assessing the burden of PDP on European healthcare systems.







