Maja Relja
University Hospital Center Zagreb, Croatia
Since its introduction in the 1980s, botulinum toxin type A (BoNT-A) has become the first-choice treatment for most types of focal dystonia, including cervical dystonia (CD) and blepharospasm. It is also widely used in the treatment of spasticity arising from stroke, spinal cord injury, multiple sclerosis and traumatic brain injury, as well as in the treatment of pain e.g. chronic migraine. However, the current guidelines for the clinical use of BoNT-A are based on historical data, some of which was published more than 20 years ago,1 and recent data suggest that patient satisfaction with current therapeutic regimes is low. A satellite symposium, co-chaired by Dr Maja Relja and Dr Jorge Jacinto, was held at Toxins 2015, Lisbon, Portugal, January 2015 organised by the Centro de Medicina de Reabilitação de Alcoitão, Portugal. Dr Relja presented the aims of the symposium: to review existing data on a patient-centric approach in spasticity and CD using BoNT-A; to provide information about recent clinical data; to consider how an individualised approach can be incorporated into clinical practice; and to provide practical expert guidance on evolving treatment strategies.
Jorge Jacinto
Centro de Medicina de Reabilitação de Alcoitão, Alcabideche, Portugal
Dr Jacinto began with the Institute of Medicine definition of patientcentric care that is respectful of and responsive to individual patient preferences, requirements and values, ensuring that patient values guide all clinical decisions.2 He proceeded to discuss the evaluation of patient-centric care in spasticity and dystonia. There is a need to establish what patients want and need, in addition to what healthcare professionals consider therapeutic goals and to provide a tool for to evaluate treatment.3,4 Many people consider that there is a discrepancy between patients’ and doctors’ evaluations.
A recent online survey (n = 969) conducted in the US and EU showed that there is a need for an improvement in CD management in terms of patient satisfaction.5 A patient-centric approach may necessitate a re-evaluation of how ambitious we should be for each treatment cycle in terms of number of muscles, doses and adjunctive treatments. Individual perception is very important in assessing treatment effect; the response to BoNT-A is multidimensional, and may be measured in terms of magnitude, duration, waning of effect, tolerability and safety. It is therefore difficult for the patients to accurately interpret treatment response. Furthermore, the response is not immediate, leading to memory bias. Therefore, it is important to evaluate treatment in an individualised manner and to manage patient’s expectations.6 In a 2005 study of 78 patients (mean age 54 years, 65 % female) with CD, patients’ satisfaction with long-term BoNT-A treatment (median 5.5 years, range 1.5–10) was evaluated on a seven-point scale ranging from excellent to worsening. The independent evaluations of the treating neurologists broadly correlated with the patient’s scores but differed in the excellent category (9 % of patients versus 17 % neurologists).7
Recommendations in national guidelines generally evaluate the effectiveness of BoNT-A treatment for spasticity in terms of improvement of the modified Ashworth scale.8–10 Treatment effect is usually measured around the time of maximum effect (between 4 and 6 weeks after injection) and after 12 weeks (termination of the study or re-injection). There is no measurement of treatment effect in the time between the peak effect and the usual time point of re-injection. In addition, functional improvement is usually not adequately measured in most studies, partly due to the lack of sensitive assessment scales that relate to real-life tasks. Duration is typically not reported, since a routine injection interval is used (and/or single injection). Doses and injection patterns are predefined in most study protocols; studies are generally constrained in this aspect by the need to serve regulatory purposes. Patient-reported outcomes are usually limited to the Global Assessment of Efficacy and Tolerability at the end of the study (mostly single-injection studies). Sometimes the Disability Assessment Scale (DAS), and, more recently, the Goal Attainment Scale (GAS) have been used.8–14
The interval between injections is a factor that has not been widely debated. Many reviews give no specific recommendations on injection interval and state that more research is required.9–12,15 The French guidelines, however, recommend a 3-month interval although they agree that long-term studies are missing.13 The UK guidelines state that although patients may become biologically resistant to BoNT-A as a result of antibody formation, it is rarely reported in practice. They recommend a review at three to four months post-injection, when the effect of the toxin is likely to have worn off.8 Current product labelling of BoNT-A formulations recommends injection intervals of ≥10 weeks16 (incobotulinumtoxinA in Europe only) to ≥12 weeks17–21 for the treatment of CD. For spasticity, the current standard of care is injection intervals of at least 3 months.22–24 However, some patients may experience re-emergence of symptoms before the next dose is administered. This may lead to reduced patient satisfaction during the latter part of the injection cycle. In practice, physicians compensate for this by giving larger doses, which may have adverse effects, or by giving adjunctive therapies.
Two recent surveys have evaluated patient satisfaction with current dosing regimens of BoNT-A for the treatment of CD and spasticity. These involved structured patient interviews that were conducted in Germany, France, the US and Canada. All participants had received ≥2 injection sessions with BoNT-A. In the survey in CD, patients receiving abobotulinumtoxinA (aboBoNT-A, Dysport®, Ipsen Ltd) or onabotulinumtoxinA (onaBoNT-A, Botox®, Allergan Inc) were included.25 In the survey in spasticity, patients receiving aboBoNT-A, incobotulinumtoxinA (incoBoNT-A, Xeomin®, Merz Pharmaceuticals) and onaBoNT-A were included.26 Interviews were conducted either at 7–8 weeks or 9–10 weeks after the patient’s last injection session; these time frames were considered to allow sufficient time for the BoNT-A to confer peak clinical effects.
In the CD survey, patients (n=136) usually received BoNT-A treatment at intervals of every 9–10 weeks (4.4 %), every 11–12 weeks (42.7 %), every 13–14 weeks (27.2 %), every 15–16 weeks (10.3 %) or >17 weeks (15.4 %). The mean (standard deviation [SD]) interval between injection sessions was 14.0 (3.7) weeks.25 Patient satisfaction tended to follow the peak and waning of treatment effect. Satisfaction was greatest when patients were recalling the time of peak treatment effect. At this time point, the majority of patients (77.5 %) were very satisfied with treatment. Fewer patients were very satisfied at the time of the interview (7–10 weeks after the previous injection session; 50.7 %), and fewer again recalled being very satisfied just prior to the last injection session (13.7 %), when the effects of the previous dose would be diminishing.25 At this time point, 39.2 % of patients reported not being satisfied at all. When asked for their preferred injection interval preferences, patients’ responses varied, with a mean preferred injection interval of 12.9 weeks, although 46 % of patients would have preferred intervals of ≤10 weeks. Around half of patients stated that, given the choice, they would have a re-injection on the day of the interview (31.6 % somewhat; 22.1 % very much).25
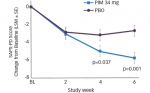
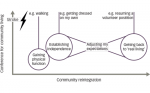
In the spasticity survey (n=79), when asked about the interval at which they normally receive injection sessions, 54.5 % of patients stated they received injections at intervals of more than 12 weeks.26 When asked about their preference for injection intervals, 78.9 % stated that they would prefer an interval shorter than 12 weeks, and 43.4 % would prefer intervals of 10 weeks or less. The majority of patients stated a preference for re-injection on the day of their interview (36.7 % somewhat; 36.7 % very much so). Interviews were conducted 7–10 weeks after the most recent injection. As seen in the CD survey, patient satisfaction tended to follow the peak and waning of treatment effect. Satisfaction was greatest when patients recalled the time of peak treatment effect. For this time point, the majority of patients (68.2 %) were very satisfied with treatment. Few patients recalled being very satisfied just prior to the last injection session (9.1 %), when the effects of the previous dose would be diminishing. There was a striking difference between the injection intervals given (54.5 % >12 weeks) and the injection intervals preferred (78.9 preferred an interval of <12 weeks, see Figure 1). The majority of patients stated that, given the choice, they would have a re-injection on the day of their interview (31.6 % somewhat; 22.1 % very much so).26
In summary, the mean BoNT-A injection interval for patients is approximately 14 weeks. However, nearly the half of patients with CD and spasticity would prefer intervals of 10 weeks or less. Patient satisfaction levels generally follow the onset, peak and trough of clinical effect. Satisfaction was lowest just prior to the next injection session, which may have been due to symptom re-emergence. Shorter injection intervals may therefore improve overall patient satisfaction.
Joseph Jankovic
Baylor College of Medicine, Houston, Texas, US
Dr Jankovic began by reinforcing the conclusion of the previous presentation: that some patients might benefit from more frequent injections than the currently recommended minimum injection intervals of ≥12 weeks, which is based on data published more than 20 years ago.1 Three recent double-blind clinical trials have, for the first time, investigated on-demand, flexible injection intervals to allow treatment individualisation.27–29 In these trials, patients were able to visit the physician when they felt a repeat injection was necessary. The physician then objectively verified the need for a repeated injection, and retreated where indicated. In two trials, the study design was a randomised, placebo-controlled, double-blind main period, in which patients received a single injection of placebo or incoBoNT-A,30,31 and in one study this was followed by an open-label extension period comprising a maximum of five injection sessions at ≥6-week intervals (the maximum study duration was 88 weeks for an individual patient; see Figure 2).27,28 The third study evaluated the safety of two different doses of incoBoNT-A in a randomised, double-blind fashion as an extension to the CD placebocontrolled study. The study permitted flexible injection intervals as short as 6 weeks if patients had a clinical need for re-injection. Important inclusion criteria were Jankovic Rating Scale (JRS)32 severity subscore ≥2 in blepharospasm and Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS) 33 total score ≥20 in CD.
The mean study duration of the blepharospasm extension study was 52.6 weeks (range 6.3–75 weeks); 79.4 % received at least four of the maximum five possible injections. The mean (SD) injection interval was 12.6 (4.5) weeks (median 12 weeks). The majority (94.9 %) of re-injections were administered after intervals of 6 to 20 weeks: 23.7 % were 6 to ≤10 weeks; 32.2 % >10 to ≤12 weeks; 24.7 % >12 to ≤14 week; and 19.4 % >14 weeks. The mean total doses (SD) of incoBoNT-A ranged from 64.7 (22.4) U (unit of biological activity) at the first injection to 72.7 (22.0) U at the fifth injection visit, range: 15.0 to 100.0 U.28 The mean JRS sum scores significantly improved from each injection visit to the respective control visit 6 weeks later (p<0.001 for all sessions; see Figure 3), with mean (SD) improvements at the control visits ranging from –1.6 (1.8) to –2.4 (2.2). The mean (SD) JRS sum scores at the injection visits decreased across the study duration from 5.9 (1.4) to 4.9 (1.2). The mean JRS sum score at the trial termination visit (TTV) was significantly lower than at the first and the fifth injection visit (p<0.001). Similar patterns were seen for the JRS severity and frequency subscores (p<0.001 for all changes from injection to control visit; p≤0.002 for all changes from first or fifth injection visit to the TTV). The mean Blepharospasm Disability Index (BSDI) mean scores significantly improved from each injection visit to the respective control visit (p≤0.001 for all). BSDI mean score at the TTV was significantly lower than at the 1st injection visit (p=0.043). Improvements from injection to control visits were significant for each single item score of the BSDI (p≤0.038 for all). Investigators rated the tolerability of treatment for each injection cycle at the subsequent injection visit and at the TTV (for the fifth or last injection session) Investigator Global Assessment of Tolerability (IGAT) scale ranges from 1 (very good) to 4 (poor). The tolerability was rated ‘good’ or ‘very good’ for the vast majority of patients (≥96.4 % for each injection cycle, see Figure 4). At each contact, patients were directly questioned about adverse events (AEs) that could indicate toxin spread (stomach and bowel disturbances, drooping of eyelids, vision problems, dry mouth, swallowing difficulties, speech problems, shortness of breath, respiratory infection, local weakness, facial weakness and general body weakness). The most frequently reported AEs were eyelid ptosis and dry eye symptoms as expected. Frequencies of drug-related AEs per injection cycle ranged from 7.1 % to 11.8 % for eyelid ptosis and from 3.6 % to 6.9 % for dry eye symptoms. In total, 43.1 % of patients reported ≥1 AE over all five injection visits during the open label extension phase.
In the CD studies, patients (n=219 completing the main randomised, double-blind, placebo-controlled period; 214 in the extension randomised, double-blind study) were randomised to at the beginning of the studies to 240 U or 120 U (or placebo in the main phase). Evaluation of TWSTRS scores showed a significant improvement over the extension period (see Figure 3).27 At every contact, patients were questioned about AEs; the most frequently reported treatment related AEs were dysphagia, injection-site pain, neck pain, muscular weakness and musculoskeletal pain (see Table 1). No serious treatment-related AEs were reported.
There was a wide range of injection intervals: ≤10 weeks (22.5 %), >10 to ≤12 weeks (24.6 %), >12 to ≤14 weeks (19.4 %) and >14 weeks (33.5 %) No differences were seen in the overall occurrence of AEs between the injection groups (p=0.1117).27
An additional safety analysis in the CD study evaluated the incidence of dysphagia, muscular weakness, neck pain and injection site pain according to injection interval. The frequency of AEs per injection session was lower in the 6–7 week injection interval than the AE rate in longer injection intervals and in comparable single injection trials.29 Investigators rated treatment tolerability for each injection cycle at the subsequent injection visit or at the TTV (up to 20 weeks after the last injection). Using the IGAT scale, tolerability was rated ‘good’ or ‘very good’ for the vast majority of patients (≥91.5 % for all treatments) in both dose groups.27
Antibody assays were performed at screening, control visit day 6, final visit of main phase, reinjection visits and TTV. These were assessed by a validated fluorescence immunoassay for antibodies (FIA-AB). Positive FIA-AB samples were tested with a validated mouse ex vivo hemidiaphragm assay (HDA). No patients had developed neutralising antibodies (nAbs) at study termination, including those patients that required reinjection at week 6. It should be noted that 2.6 % of the onaBoNT-A pre-treated patients had nAbs at screening.28,29
In conclusion, incoBoNT-A was well tolerated and effective over the study period in the treatment of blepharospasm and CD after a total of maximum six injections. Injections administered in shorter injection intervals were as well tolerated as those given in long-injection intervals. No cumulative AEs were reported with repeated doses and the majority of AEs were mild or moderate and temporary. The clinical study data support the relative safety of short-injection intervals for incoBoNT-A.
Alberto Albanese
Istituto Nazionale Neurologico Carlo Besta, Milan, Italy
Professor Albanese began by summarising the evidence-based reviews that have resulted in BoNT-A becoming the first-choice treatment for most types of focal dystonia.34–36 BoNT-A has been given an American Academy of Neurology level A recommendation in this ndication.37 BoNT-A provides dose-related temporary denervation, targets specific muscles, maintains strength in non-treated muscles, corrects deformity without generating generalised weakness and reduces pain independently of muscle tone. Treating more severely dystonic muscles may also quell hyperactivity in other involved muscles.38 In addition, results are long lasting.39 However, when using a patient-centric approach, we need to guarantee reproducible results with guaranteed safety and tolerability.
Three formulations of BoNT-A are currently available: onaBoNT-A, aboBoNT-A and incoBoNT-A. All contain neurotoxin type A, derived from the Hall strain of Clostridium botulinum, but differ in their exact molecular composition and excipient. The formulations are supplied as powder that is reconstituted in saline for injection. In aboBoNT-A and onaBoNT-A the powder in the vial contains BoNT-A, however, the active 150 kDa neurotoxin is part of a larger complex with other proteins, for which no biological activity, influence on the diffusion profile or change of the stability of the neurotoxin have been demonstrated, although additional denatured/inactive neurotoxin is likely to be present.40 By contrast, incoBoNT-A contains only active neurotoxin. In an analysis of neurotoxin content of the three formulations, the mean concentration of BoNT-A in onaBoNT-A was 0.73 ng per 100 unit vial (coefficient of variation [CV] = 3.5 %), in aboBoNT-A, 0.65 ng per 100 units (CV = 11.4 %) and 0.44 ng per 100 unit vial of incoBoNT-A (CV = 1.9 %).41
In placebo-controlled studies in CD, all three formulations have demonstrated efficacy and safety, showing improvements in postural head deviation, TWSTRS reduction and decrease in pain rating. Most AEs have been mild and transient; some dysphagia and injection pain, blurred vision and muscle weakness has been reported.1,31,42–44 Three comparative studies have also been reported in CD. In a study designed to establish whether a ratio of 1:3 aboBoNT-A: onaBoNT-A is equivalent, the mean time to retreatment was 3 days shorter in the aboBoNT-A group than in the onaBoNT-A group (not significant).45 In another study, higher improvement of Tsui scores (primary outcome criteria) was seen with aboBoNT-A compared with onaBoNT-A (ratios of 1:3 or 1:4 were used). No significant difference was seen between the 1:3 and 1:4 groups, and more AEs were reported with aboBoNT-A, the most frequent being dysphagia (3 % with onaBoNT-A, 15.6 % with aboBoNT-A 1:3, and 17.3 % with aboBoNT-A 1:4), but the effect was minor.46 In the first comparative study of onaBoNT-A and incoBoNT-A in CD, a 1:1 ratio was used. No difference was seen between the two groups in the mean change from baseline in TWSTRS severity score 1-month post injection.47
In terms of blepharospasm, the use of BoNT-A is based on four placebo-controlled trials.30,32,44,48 Three comparative studies have also been reported, and all show no differences in efficacy and safety outcomes between onaBoNT-A and incoBoNT-A.49–51 Using a 4:1 ratio for aboBoNT-A and onaBoNT-A, similar results were obtained for the two treatments, suggesting that this conversion factor is a good estimate of their comparative clinical potencies.52 In addition, numerous placebo-controlled trials support the use of all three formulations of BoNT in spasticity.53–67
In terms of switching from one product to another, while several studies have shown that a 1:1 ratio of onaBoNT-A: incoBoNT-A is appropriate for clinical dose conversion,41,68–74 the potency of aboBoNT-A relative to onaBoNT-A has been estimated to range from 1:2 to 1:11.75,76 A randomised controlled trial suggested a ratio of 1:3 but the products are still not equivalent at this ratio.77 Recent studies suggest that 1:4 may be more appropriate.73,78 AE rates are comparable for all three products with conversion ratios of 1:1 for onaBoNT-A and incoBoNT-A; and 1:4 for incoBoNT-A/onaBoNT-A and aboBoNT-A.68,79
In summary, in terms of a patient-centric approach, all three BoNT-A formulations have been shown to be effective and well tolerated in a range of indications but the switch from aboBoNT-A to onaBoNT-A or incoBoNT-A is more difficult due to the variable relative potency.