In 1945 Karl Ekbom coined the term ‘restless legs syndrome’ (RLS), which is still sometimes referred to as Ekbom’s syndrome. RLS is a common sensorimotor condition characterized by predominantly nocturnal dysesthesias relieved by limb movement. RLS is not a new disorder, having been documented in the medical literature for over half a century.1 However, in recent years RLS has been receiving increased attention following approval, in May 2005, by the US Food and Drug Administration (FDA) of the first agent indicated for the treatment of the condition. Also in 2005 the epidemiology and pathophysiology of RLS were reviewed by the RLS Foundation in the RLS Medical Bulletin2 (available at www.rls.org).
This article summarizes the current understanding in these fields and highlights the advances made since 2005. The clinical diagnosis and management of RLS are beyond the scope of this article and have been reviewed elsewhere.2–4
Epidemiology
Definition
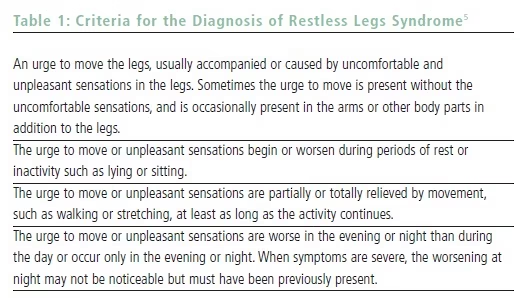
Epidemiological characterization necessitates a clear definition of disease. The first formal criteria for the diagnosis of RLS were published by the International RLS Study Group (IRLSSG) in 1995. These criteria were updated in 2002 (see Table 1) and represent the current ‘gold standard’ for diagnosis of RLS.5 The presence of RLS correlates with periodic leg movements of sleep (PLMS) on polysomnography and periodic leg movements of wakefulness (PLMW) on the suggested immobilization test,6 but the diagnosis remains purely clinical. Hence, epidemiological studies rely on subjective reports. The IRLSSG criteria do not specify a cutoff of symptom frequency or severity, although there are many people in whom RLS symptoms are mild and do not impair quality of life (QOL). There has not been a universally accepted definition of clinically significant RLS, although the International RLS Study Group Rating Scale (IRLS) is currently the best validated measure of severity, with a score greater than 10 points (of 40 possible total points) indicating moderate to severe disease.7 Future research will likely employ published validated instruments to define clinically significant RLS.
Prevalence
Ekbom estimated the prevalence of RLS to be 5% in the general population. Subsequent survey studies have estimated the population prevalence of the disorder to be 1–29%.8 The RLS Epidemiology, Symptoms, and Treatment (REST) trial is the largest survey study to date of RLS prevalence. Questionnaires were completed by 23,052 patients presenting to primary care practices in the US and four Western European countries during a two-week period. Any degree of RLS symptoms was experienced by 11.9% of respondents, 9.6% had at least weekly symptoms, and 551 (2.4% of total respondents, 3.4% of respondents with complete data) had at least twice-weekly symptoms and endorsed a negative impact on QOL.9 Recently, similar figures have been reported in the Irish10 and Spanish11 primary care populations.
Prevalence estimates derived from primary care patients may overestimate general population prevalence because older and sicker persons are over-represented. However, a 1996 random digit dialing survey of adult Kentucky residents estimated a 10% prevalence of RLS in the adult population,12 which is similar to that found in the REST study.
International variations in the prevalence of RLS and the genetic and sociocultural differences that may account for this variation remain poorly understood. Most prevalence studies of RLS have been conducted on Caucasian populations. Prevalence estimates in East Asian studies included 0.1% in a Singaporean survey13 and 12.1% in a large Korean survey.14 (The latter study used a single question—“Have you ever experienced symptoms of RLS?”—so the prevalence of clinically significant RLS is probably much lower.) A Japanese survey found RLS symptoms in 5% of respondents but clinically significant RLS in 1.5%.15 Recently, Rangarajan et al. reported the results of a door-to-door survey of 1,266 individuals in Bangalore, India. They found a prevalence of RLS of 2.1% using the IRLSSG criteria, and 1.2% reported RLS that disrupted sleep.16 The prevalence of RLS in African populations has not been studied.
In summary, symptoms of RLS are quite common, and the population prevalence of RLS severe enough to cause impairment in QOL and warrant medical treatment is probably about 2–3%. This makes clinically significant RLS two to six times as prevalent as epilepsy in developed countries (estimated prevalence of 0.5–1%).17
Demographic Distribution
Many epidemiological studies have found some degree of female predominance among RLS sufferers, but reported female–male ratios vary from one to three. The female–male ratio among subjects with RLS in REST was 2.1, but this ratio did not differ significantly from the female–male ratio of all survey respondents.9 In the Kentucky telephonebased survey, the odds ratio (OR) for RLS in females was 1.33.12 In contrast, Lee et al. found an OR of 2.64 (95% confidence interval (CI) 1.24–7.74) in an American community sample,18 and Berger et al. found an OR of 1.98 (95% CI 1.25–3.13) in a German population.19 The weight of evidence would suggest that about twice as many women as men suffer from RLS, but the physiological basis for this difference and the degree to which this figure may be exaggerated by reporting bias are not known.
Population-based studies have found an increasing prevalence of RLS with age. Phillips et al. found a 3% prevalence of RLS symptoms in persons <30 years of age, about 10% in persons 30–79 years of age, and 19% in persons 80 years of age and older.12 Berger et al. found a steady increase from 4% in the third decade to 15% in the eighth decade.19 The IRLSSG has defined criteria for the diagnosis of RLS in children,5 and Kotagal and Silber retrospectively diagnosed RLS in 32 of 538 patients presenting to a pediatric sleep disorders clinic.20 However, populationbased studies assessing the prevalence of RLS in the pediatric population are lacking. As many adult RLS patients report an onset of symptoms in childhood,21 there is reason to believe that substantial numbers of children and adolescents are affected.
Race
Racial differences in RLS have not been completely explored. Anecdotally, African-Americans are under-represented in RLS specialty clinics.8,18 However, an analysis of a community-based sample of 1,071 adults in Baltimore found the prevalence of clinically significant RLS to be 4.7% in African-Americans and 3.8% in Caucasians. There was no statistically significant difference in the prevalence between groups before or after adjustment for other demographic variables.18 Thus, the relative absence of African-Americans in specialty clinics likely has much more to due with access to and utilization of healthcare than with biological differences.
Associated Conditions and Exposures
RLS is encountered with greater than expected frequency in several general medical conditions, and the RLS occurring in these conditions is often referred to as secondary RLS. The most well-established secondary causes of RLS are renal failure, iron deficiency, and pregnancy. RLS is common, with 20% prevalence, in the hemodialysis population, tends to be more severe than primary RLS, and is a predictor of mortality in this population.22 Iron deficiency has long been thought to be associated with RLS.23 O’Keffe et al. demonstrated significantly lower levels of ferritin (a sensitive indicator of body iron stores) in RLS patients than in controls,24 and this finding has been reproduced in several subsequent studies.8 Ekbom first noted an increased prevalence of RLS in pregnancy, and Manconi et al. have applied IRLSSG criteria to 200 consecutively enrolled pregnant women and found prevalences of 27 and 12% for symptoms at least twice monthly and at least three times weekly, respectively.25
Less well-characterized associations have been found with myelopathy, diabetes mellitus, neuropathy, and Parkinson’s disease. RLS has anecdotally been seen in spinal lesions, and Hogl et al. prospectively demonstrated incidence of transient RLS following spinal anesthesia.26 Although their findings failed to reach statistical significance (p=0.1), Skomro et al. found double the prevalence of RLS among type II diabetics compared with controls.27
Dopamine antagonists (antipsychotics and anti-emetics) have been shown to cause motor restlessness and increased PLMS, and may cause RLS.2 Although antidepressant medications have been anecdotally reported to cause or exacerbate RLS, a review of 200 patients presenting to a sleep clinic (45% with RLS and 38% on antidepressants) found no association between RLS and antidepressant use.30
There is a higher prevalence of periodic limb movement disorder and RLS among children with attention deficit hyperactivity disorder (ADHD) versus controls,31 and a small non-controlled trial of dopaminergic treatment in children with RLS and ADHD demonstrated significant improvement in both conditions, suggesting an etiological link.32 The association between RLS and ADHD is deserving of, and likely to receive, more study in the near future.
The association between physical inactivity and RLS is another area deserving further study. Phillips et al. reported an OR for RLS of 3.32 (95% CI 1.67–6.30) for persons exercising for less than three hours per month,12 and a single small randomized trial of prescribed exercise for RLS demonstrated significant improvement in RLS severity.33 While inconclusive, these findings suggest that physical inactivity may be a modifiable risk factor for RLS.
Medical Attention Seeking and Physician Awareness
In the REST population, 65% of respondents with clinically significant RLS (at least twice-weekly symptoms) reported seeking medical attention for their symptoms within the preceding 12 months. Of this 65%, only 25% received a diagnosis of RLS.9 In the more recent Irish primary care study, only 32.4% of patients with moderate to severe RLS reported previously seeking medical attention for the symptoms, and only four of 24 patients (16.7%) who sought medical attention had received a diagnosis of RLS despite the majority of these patients reporting disruption of sleep and impairment in QOL.10 Clearly, improved patient and physician awareness of RLS would increase the rates of diagnosis. Currently, the pharmaceutical industry is investing heavily in promoting both patient and physician awareness of RLS.34 There has been exponential growth in the number of scientific articles about RLS published in recent years (see Figure 1). Even with this growth, RLS is relatively infrequently discussed in the medical literature. In the first eight months of 2007, 94 articles were indexed in Medline with the major medical subject heading (MeSH) of RLS compared with 1,828 articles indexed during the same time period with the major MeSH of epilepsy.
Genetics
The proportion of RLS patients with an affected first-degree relative has consistently been found to be higher than would be expected by chance alone, suggesting an inherited susceptibility to disease. Among a nonrandom sample of RLS patients, Walters et al. found that 81% of patients with onset of symptoms before 20 years of age had a positive family history compared with 58% of patients with later-onset symptoms.32 The results of a segregation analysis of 238 RLS patients, 537 first-degree relatives, and 133 spouses revealed strong evidence for an autosomal dominant pattern of inheritance in patients with early-onset RLS (symptoms prior to 30 years of age), but no similar indirect evidence for a single gene responsible for later-onset disease.35
Before 2006, three susceptibility loci had been identified on chromosomes 12q (RLS1), 14q (RLS2), and 9p (RLS3).36 Three more susceptibility loci, on chromosomes 20p (RLS4), 2q (RLS5), and 6p (RLS6), have subsequently been identified.37 Despite the strong evidence for a genetic component to RLS, attempts to identify culpable genes have so far been disappointing.38 Given that a subset of RLS patients probably have disease associated with single gene mutations, the potential discovery of disease-causing genes holds promise for better elucidating the molecular mechanisms of RLS.
Pathophysiology
The basic pathophysiological mechanisms of RLS remain poorly understood. Pharmacological, physiological, pathological, and neuroimaging studies have implicated dopaminergic systems, brain iron metabolism, and the endogenous opioid system. However, deciphering which observed changes are causative and which are secondary phenomena remains elusive.39
Dopaminergic Systems
Since the serendipitous finding by Akpinar in 1982 that relatively small doses of levodopa provided relief in RLS, it has been shown conclusively that levodopa and the dopamine agonists improve the symptoms of RLS.2 This has led to the conclusion that dopaminergic systems must play some

role in the pathophysiology of RLS. The fact that co-administration of domperidone (a peripheral dopamine antagonist) does not decrease the efficacy of pergolide (a dopamine agonist) in treating RLS lends support to the hypothesis that central rather than peripheral dopaminergic systems are responsible for RLS.40
Multiple single positron emission tomography (SPECT) studies have failed to find a difference between RLS patients and controls in dopamine transporter (DAT) binding in the striatum.2 However, in a positron emission tomography (PET) study of 16 RLS patients and 16 matched controls, Cervenka et al. found significantly reduced D2-binding potential in the thalamus and anterior cingulate cortex of RLS patients. They hypothesized that since these regions are involved in central sensory processing, impaired central dopaminergic transmission may account for the sensory symptoms of RLS.41
The diencephalospinal dopaminergic tract originating from the A11-A14 nuclei has received much attention as the potential anatomical site of dopaminergic dysfunction in RLS. This system projects to the limbic system, sensory cortex, and spinal cord.8 The proximity to circadian control centers in the hypothalamus may offer some explanation for the circadian pattern of symptoms observed in RLS.4 A rat model for the study of this system has been developed.42
Paulus and Trenkwalder have published a detailed hypothesis of how downregulation of D2 receptors (and overstimulation of D1 receptors with increasing dopaminergic therapy) may lead to augmentation and the delayed clinical worsening of symptoms seen in 60% of patients treated with levodopa.43
Brain Iron Metabolism
Iron deficiency has long been associated with RLS, and iron therapy has been effective in some cases.23 Earley at al. demonstrated markedly reduced cerebrospinal fluid ferritin levels and elevated transferrin levels in RLS patients compared with controls, even though there was no difference in serum ferritin levels.44 Thus, brain iron metabolism may be implicated in RLS even in the absence of total body iron deficiency.
A magnetic resonance imaging (MRI) study in five RLS patients and five controls demonstrated reduced iron concentration in the substantia nigra and putamena of RLS patients,45 and a subsequent larger study found decreased regional brain iron concentration in early-onset RLS patients relative to controls (but not late-onset RLS compared with controls).46 A pathological examination of the substantia nigra of RLS patients provided further evidence for regional iron deficiency. Surprisingly, transferrin receptor quantity was decreased (the opposite of what is seen in an irondeficiency state) and iron-regulatory protein 1 (IRP1) was deficient, leading to the hypothesis that a primary protein dysfunction in the brain iron-regulation system may be responsible for RLS.47
Relationship Between Brain Iron and Dopamine
Multiple potential biochemical links exist between the dopaminergic system and brain iron metabolism. Iron is a co-factor for tyrosine hydroxylase, the rate-limiting enzyme in the synthesis of dopamine.48 The dopamine transporter (DAT) is also impaired during iron deficiency.39 Further research will shed light on a unifying theory of RLS pathogenesis.
Opioid Systems
Successful amelioration of RLS symptoms has been demonstrated with oral opioids.4 A PET study assessing opioid binding found no group differences between 15 RLS patients and 12 controls, but did find significant negative correlation with RLS severity and 11C-diprenorphine uptake in the caudate nuclei, medial thalami, and anterior cingulated gyri.49 The pathophysiological significance of these findings remains unclear.39
Conclusion
RLS is a common disorder and likely causes significant morbidity in about 2% of the population. Women are more commonly affected, and the prevalence increases with age. The etiology and pathophysiology of RLS remain poorly characterized, but there has been a surge of interest in the disorder in recent years, and continued research will likely refine our growing understanding of this disorder. Enhanced awareness among patients and clinicians will likely continue to make RLS a common topic in clinical practice.