Diagnosis of Cervical Dystonia
Diagnosis of Cervical Dystonia
Dystonia involves a lack of synergy of antagonist and agonist muscles, resulting in irregular and unco-ordinated movements.1 Clinically, focal dystonia occurs when the involuntary movements are isolated to one body part such as a limb (writer’s cramp), the larynx (spasmodic dysyphonia), or the eyes (blepharospasm). Cervical dystonia (CD), a form of focal dystonia involving the neck muscles, presents with abnormal postures of the neck. While typical CD presents with tilt (laterocollis), turn (torticollis), and/or pulling forward (anterocollis) or backward (retrocollis), any combination of these may be seen. In addition, some patients present with superimposed tremor and/or pain. While the involuntary movement is always part of CD presentation, in some patients pain can be the prominent complaint.2
The incidence of CD is reported to be 1/250,000 people,3 but the numbers are often thought to be higher due to delays in referral and an inability to accurately diagnosis CD. In a European study, the prevalence of primary dystonia in patients over 50 years of age was 732 per 100,000,4 suggesting that the true prevalence of primary dystonia may be significantly higher than the published rates. A 2008 study in an ethnically diverse population identified 66 incident cases of CD from 8.2 million person-years of observation. The minimum estimation of the incidence of CD in this population is 0.80 per 100,000 person-years. The incidence was higher in Caucasian individuals and 2.5 times higher in women than in men.5
The cellular pathology of CD is unknown, but functional magnetic resonance imaging (fMRI) of patients with CD demonstrated increased activation in the caudate nucleus, putamen, and thalamus.6 Recent work in non-human primate studies revealed that lesions in brain stem areas involved in the control of muscular tone with gamma-aminobutyric acid (GABA)-ergic manipulations in various basal ganglia nuclei or thalamus also lead to dystonia, suggesting that the illness is associated with aberrant sensory representations interfering with motor control.7 Patients with dystonia may often manifest a sensory trick, such as a touch or movement that temporarily alleviates the CD symptoms. These clinical findings support the fMRI discoveries suggesting the interaction of sensory and motor pathways in the pathophysiology of dystonia.
The diagnosis of CD is based solely on clinical signs and symptoms. While there is one commercial genetic test for dystonia (DYT-1), for almost all cases of isolated CD there is no diagnostic test.8 A recent screening tool was developed as part of a larger study of familial dystonia: the Beth Israel Dystonia Screen (BIDS). A computer-assisted telephone interview was tested on 193 individuals from 16 families with CD and cranial dystonia and correlated with a videotape assessment as the gold standard. The BIDS correctly identified patients with CD as having a positive response to at least two of five screening questions and a sensitivity for CD of 100% and a specificity of 92%.9 However, despite the success of the BIDS there remains no diagnostic imaging or blood test to confirm the clinical suspicion. The diagnosis of CD remains clinical and may often result in patients making recurrent trips to specialists for confirmation. In a recent large study the duration of the period between showing symptoms and diagnosis was 3.9 and 5.3 years for women and men, respectively.5
In most cases CD is idiopathic, but in rare patients CD may be present in cases with a genetic, traumatic, or iatrogenic cause. Idiopathic CD typically peaks in later years, but an early age at onset is not uncommon. Patients may report subtle symptoms over years and family members may report a gradual increase in symptoms over time. In older literature, a remission rate of 10–120% was reported, but persistent remission in patients has not been reported since the advent of botulinum toxin (BoNT) treatment. The ability of patients to transiently moderate their symptoms with sensory tricks such as using a tooth pick or closing one eye suggests a diagnosis of CD.
Recently, attention has been paid to the increasing role of genetics in the diagnosis of dystonia. Familial dystonia is usually limited to generalized dystonia but isolated CD in a few large families has been reported. Only one genetic form of dystonia, DYT-1, is available commercially. Ongoing research into other forms of dystonia continue, but the majority of genetic forms of dystonia remain generalized and/or present with specific features unique to that syndrome, such as rapid onset,11 alcohol responsive (myoclonic dystonia),12 or responsive to L-dopa (dopa-responsive dystonia).13
Secondary dystonia may arise from trauma, overuse, and/or medications.14 Tardive dystonia present similarly to idiopathic CD.15 While the newer antipsychotic medications are said to have less chance of iatrogenic movement disorders, tardive dystonia remains an issue with all medications that block dopamine. The use of metoclopramide for nausea remains a risk factor for developing tardive syndromes.16 Additionally, patients may experience minor or major trauma to the neck, acting as a precipitant to CD.17 The role of trauma in the development of CD is less clear than the role of overuse in musicians or other occupational dystonia.18 Regardless of the etiology of CD, the treatment remains the same as idiopathic CD.
Treatment
Oral Medications
The treatment of CD includes oral medications, such as anticholinergics and benzodiazepines, and antispasmodics, such as baclofen. The efficacy of oral medications in focal dystonia is limited. Only one study compared BoNT with oral medications (trihexyphenidyl).19 BoNT injections provided more efficacy and fewer side effects than oral trihexyphenidyl in patients with comparable CD. While a wide variety of other oral medications has been used, only trihexyphenidyl has been studied in a large clinical trial. Levetiracetam has been studied in at least two open label trials and both demonstrated no improvement.20,21
Botulinum Toxin for Cervical Dystonia
The accepted first-line therapy for CD is intramuscular injection of botulinum toxin. A recent report by the American Academy of Neurology (AAN) panel of experts noted that BoNT should be first-line treatment for CD.22 The panel noted that seven class I studies of the use of BoNT in CD demonstrated efficacy.23–26 While Simpson addressed the efficacy of BoNT injections in the treatment of CD, the authors did not differentiate between the efficacy, quality, or volume of literature in the different formulations of serotype A and the formulation of serotype B.
Worldwide, there are four main BoNT products available for clinical use (see Table 1): BOTOX® (Allergan, Inc., Irvine, US), Dysport® (Ipsen Pharmaceuticals, Slough, UK), Myobloc®/Neurobloc® (Solstice Neurosciences, Inc., South San Francisco, US/Solstice Neurosciences Ltd, Dublin, Ireland), and Xeomin® (Merz Pharmaceuticals GmbH, Frankfurt, Germany). Three of the four are BoNT serotype A (BoNTA) products (BOTOX, Dysport, and Xeomin), and Myobloc is a BoNT serotype B (BoNTB) product. All BoNTs are biological products originating from one of the seven naturally occurring serotypes of clostridium botulinum. Production within a serotype varies by manufacturer, and therefore no generic equivalent is available for these toxins. Thus, trade names will be used to clarify which formulation is being discussed (see Table 1).
Use of Botulinum Toxin Serotype A for the Treatment of Cervical Dystonia
Botulinum Toxin Serotype A Formulated as Botox®
As of 2008, the only form of BoNTA available worldwide is Botox. First introduced into the US market in 1989 as a treatment for strabismus,27 Botox is currently approved in CD, strabismus, facial injections, and medically refractory hyperhidrosis.
The largest trial of BoNTA studied 170 subjects with CD at 21 centers and is detailed in the package insert.28,29 This trial has been referred to in reviews of CD treatment, but the study itself has not been published in its entirety in a peer-reviewed publication. The study included only patients with a good response to previous Botox injections. Using a 3D measurement tool to gauge degree of turn, tilt, or other postures, the physicians followed the change in patients treated with active Botox or placebo.30 In an enriched sample of only CD responders, half received a second injection of placebo and the remainder a second treatment of Botox. The difference between the BoNTA- and placebo-treated groups on the Cervical Dystonia Severity Scale (CDSS) was 1.03 to 3.13 (corresponding to an improvement of approximately 5.15º to 10.65º in head position) (p≤0.046) at weeks two, four, six, eight, and 10. In addition, a Physician’s Global Assessment score was statistically significant at weeks two, four, six, and eight. According to the package insert, the common adverse events (AEs) for the Botox-treated patients were upper respiratory infections, neck pain, back pain, dysphagia, and rhinitis.
Botulinum Toxin Serotype A Formulated as Dysport®
In a large, multicenter, double-blind, randomized, controlled trial in the US, 80 patients with CD were randomly assigned to receive one treatment with Dysport (500 units) or placebo. Over the 20-week trial, Dysport demonstrated more improvement in the total Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS) score than placebo at weeks four, eight, and 12. The median duration of response to Dysport was 18.5 weeks. Side effects were generally similar in the two treatment groups; only blurred vision and weakness occurred significantly more often with Dysport.
In a similarly sized multicenter dose escalation, 75 patients were randomly assigned to receive treatment with placebo or total doses of 250, 500, or 1,000 Dysport units divided between two muscles. Those treated with 500 or 1,000 units demonstrated significant changes in the modified Tsui score at week four versus placebo (p<0.05). The 1,000-unit dose was found to be more effective, but was associated with an increased risk for side effects. The authors noted that because of neck weakness and voice changes, the starting dose should be 500 units. The most common AEs were dry mouth (21, 18, and 33 with 250, 500, and 1,000 units, respectively), neck muscle weakness (11, 12, and 56% with 250, 500, and 1,000 units, respectively), and dysphagia (21, 29, and 39% with 250, 500, and 1,000 units, respectively).
Botulinum Toxin Serotype A Formulated as Xeomin®
The newest BoNTA on the market is Xeomin. It is described as a purified, freeze-dried form of BoNT, and is reportedly free from completing proteins.31 Trials have focused on head-to-head trials with Botox. No placebo-controlled trial of Xeomin in patients with CD has been reported. In the non-inferiority study, both drugs were similar in the treatment of patients with CD.32 A total of 466 patients with CD were recruited from 51 European centers into a large clinical trial of Xeomin in patients with CD. There was no difference in efficacy between Xeomin and Botox on day 28 after injection using the total score on the Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS). Both treatment groups improved with the injections and the authors propose that the clinical effect of the two drugs were similar in this patient population.
Which Toxin Should Be Used for Cervical Dystonia?
The selection of which BoNTA to use rests entirely with the familiarity of the physicians with each formulation. The number of units used clinically for different forms of BoNTs varies according to serotype and formulation. The gold standard for the comparison of serotypes and formulations remains the mouse unit. Units of BoNT products are determined by mouse lethality assays to establish the intraperitoneal dose that results in lethality of 50% of a population of mice (IP-LD50).33 Each formulation is unique and not interchangeable. Differences in drug product excipients and production conditions such as mouse strains, environmental conditions, intra- and interlaboratory variations, and/or toxin diluents prevent direct comparisons of potency.34 There is no generic form of BoNT.
In a large, multicenter trial comparing BoNTB with BoNTA (Botox), 139 BoNTA-responsive patients with CD were randomized to receive either product.35 Comella et al. reported no difference in the improvement noted in the TWSTRS total score at week four. As noted with placebo-controlled trials of BoNTB,36 the frequency and severity of dysphagia and dry mouth were significantly greater with Myobloc (dysphagia: BOTOX 19% versus Myobloc 48%; dry mouth: BOTOX 41% versus Myobloc 80%). In those benefiting from either drug, the BoNTA-treated group had a modestly longer duration of benefit (Botox 14 weeks, Myobloc 12.1 weeks; p=0.033).
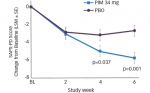
Recently, Myobloc was compared with Botox in a large, randomized, clinical trial of toxin-naïve patients suffering from CD.37 The patients in Comella et al., discussed above, all had prior exposure to Botox but not Myobloc. As with other similar trials, the change in the TWSTRS total score at week four was the primary efficacy outcome. Of the 111 toxin-naïve patients participating, similar improvement in TWSTRS total scores was seen in both groups after four weeks. In this study the median duration of effect of BoNTA and BoNTB did not differ and there were no significant differences in the occurrence of injection site pain and dysphagia. As noted in all other studies with BoNTB, dry mouth was more frequently reported.
Frequency of Treatment
The recommended frequency of treatment with BoNT stems from studies of antibody formation. Most physicians treat patients no more than every three months based on concerns for antibody formation with more frequent, high-dose injections. The theory proposed is that higher dose and more frequent injections have the potential to immunize a patient to the protein in the neurotoxin complex. Some studies have used an enzyme-linked immunosorbent assay (ELISA), which measures antibodies, but the ability to measure antibodies that specifically block the activity of the toxin has become more of a focus.38,39 The gold standard for measurement of blocking antibodies remains the mouse protection assay.40 Early studies reported that antibody formation is associated with more frequent and higher doses of BoNT.40 Early reports of with BoNTA (Dysport and Botox) in CD suggested that the incidence of neutralizing antibodies ranged from 4 to 17% depending on the formulation used.41 More recently, a newer formulation of Botox demonstrated an antibody rate of 1.2% (four of 326 patients participating) after a mean of 2.5 years (range 3.2 months to 4.2 years) of treatment. In a longitudinal study of BoNTB in 100 patients with CD, one-third of the patients who were negative for BoNTB antibodies at the beginning of the study became positive for BoNTB antibodies at the last visit, suggesting a high likelihood of development of blocking antibodies after long-term treatment with BoNTB antibodies.
Side effects of BoNT injections for the treatment of CD are generally mild, dose-related, and well tolerated. Intramuscular injections of BoNTA in the neck are associated with neck weakness, dysphagia, and exacerbation of neck pain. Dry mouth has been reported with BoNTA, but in all studies is more common after treatment with BoNTB.42–47 The correct conversion ration of doses between the two common forms of type A, Dysport, and Botox, remains unsettled. In a cross-over study of patients with CD comparing Dysport with Botox at conversion factors of 3:1 and 4:1 (Dysport:Botox), total AEs were significantly higher with Dysport: 17.6% of patients experiencing AEs with Botox versus 33% with Dysport (3:1) and 36% for Dysport (4:1).48 Of note, the incidence of dysphagia was greater with both Dysport treatments (15.3 and 17.3% in the 1:3 and 1:4 dose conversion rate groups, respectively) compared with Botox treatment (3%).49 These results reinforce the need for independent assessment of patients by physicians rather than relying on a mathematical calculation when changing formulations, otherwise the risk of applying a fixed-dose ratio between formulations or serotypes could lead to relatively under- or overdosing, potentially leading to a suboptimal therapeutic response or higher incidence of adverse effects. There appears to be a 1:1 conversion rate between Xeomin and Botox, but more studies are needed.
Usefulness of Electromyography
The use of electromyography (EMG) to guide BoNT remains one of personal choice by the treating physician. The AAN position paper on BoNT noted that there are insufficient data on the use of EMG with BoNT injections.22 Comella et al. randomized 52 patients with CD to treatment with EMG and to clinical examination only for muscle selections. The EMG group demonstrated a greater improvement.49 EMG mapping has also been advocated as improving the accuracy of the injections.50
Impact of Cervical Dystonia on Quality of Life
The impact of CD on quality of life (QOL) is a relatively new area of study. A new scale—the CD Impact Profile (CDIP-58)—was developed as a tool to measure the health impact on CD in eight health dimensions (head and neck symptoms, pain and discomfort, upper limb activities, walking, sleep, annoyance, mood, and psychosocial functioning). Built on patient interviews, the CIDQ-58 may be a useful complement to the more traditional TWSTRS scale often used in therapeutic CD trials.51 In trials of CD patients treated with BoNTA the CIDQ-58 subscales were more sensitive in detecting statistical and clinical change than similar subscales of the Medical Outcome Study Short Form-Health Survey (SF-36), Functional Disability Questionnaire (FDQ), and the Pain and Activities of Daily Living subscales of the TWSTRS.52
Patients with CD often suffer from depression.53 In a health-related QOL study, depression was found in 47.5% of patients. While this improved when treated with BoNTA, depression, female sex, poor financial situation, and living alone were all predictors of worse health-related QOL. After treatment with BoNTA, improvements were noted in all areas of the SF-36, a visual analog scale, TWSTRS, and the Montgomery-Asberg Depression Rating Scale (MADRS).55 While patients improved, the TWSTRS results did not correlate with any of the SF-36 subscores, suggesting a benefit to including QOL scales in large trials.54 Likewise, in a study of QOL in patients with focal dystonia (blepharospasm, CD, writers cramp), depression and anxiety were the most important predictors of poorer health-related QOL in all three forms of dystonia.55
One of the few studies to look at CD treatment with BoNT and employment status in 62 CD patients (patients were between 31 and 66 years of age and had been treated for a median of five years) found that the employment rate fell from 84% at the onset of CD to 47% before the initiation of BoNT treatment. With long-term BoNT treatment, 72% of those who worked at the initiation of treatment remained employed, and 67% of those on sick leave returned to work. The younger patients and those with a higher premorbid education status were more likely to return to work.56
Conclusion
The diagnosis of CD is based on clinical presentation. Intramuscular injection of BoNTA is the mainstay of therapy and should be considered as first-line. As new formulations become available, physicians will need to evaluate the dose and side effect profile for each patient. Treating physicians should also consider QOL and employment concerns when determining when to initiate therapy. The availability of BoNTA for patients with CD has significant benefit for patients with the illness. ■
Acknowledgments
In the last year, Allison Brashear, MD, has been a consultant serving on advisory boards for Allergan and Merz. In the last five years she has had research relationships with Elan, Allergan, Merz, and Ipsen Pharmaceuticals. Dr Brashear is not an employee of nor does she own stock in any of these companies. She does not receive patent royalties for any work with botulinum neurotoxins.