Perfusion is defined as the steady-state delivery of nutrients and oxygen via blood to tissue per unit volume or mass and is typically measured in milliliters per 100g of tissue per minute.1 Because blood flow brings crucial nutrients, and because it is disturbed in many disease processes, monitoring of this key physiological parameter can often provide insight into disease.
Perfusion is defined as the steady-state delivery of nutrients and oxygen via blood to tissue per unit volume or mass and is typically measured in milliliters per 100g of tissue per minute.1 Because blood flow brings crucial nutrients, and because it is disturbed in many disease processes, monitoring of this key physiological parameter can often provide insight into disease.
The brain is an unusual organ in the hemodynamic sense, with a high metabolic rate that is sustained through high cerebral blood flow (CBF). CBF is defined as the volume of blood moving through a given brain region per unit time. Normal CBF is typically greater than 50–60ml/100g/min. Unlike other high-flow organs, the limited space inside the bony cranium requires an efficient regulation system, which is accomplished with a high capillary density but remarkably low cerebral blood volume (CBV). CBV is defined as the total volume of blood in a given region of the brain. CBV has units of milliliters of blood per 100g of brain tissue (ml/100g); normal CBV is 2–5ml/100g. Mean transit time (MTT) is a slightly more complex concept. Because the transit time of blood through the brain parenchyma varies depending on the distance traveled between arterial inflow and venous outflow, the MTT is defined as the average of the transit time of blood through a given brain region, integrated across these different paths. Mathematically, MTT is related to both CBV and CBF according to the central volume principle, which states that MTT = CBV/CBF.2,3 Conceptually, MTT can be thought of as the time required for blood to cross from the arterial to the venous side of the circulation. MTT is typically measured in seconds.
While magnetic resonance imaging (MRI) has traditionally been used to evaluate anatomy, with its main application being the central nervous system (CNS), the recent application of MRI to visualize tissue physiology or function has met with great success. Indeed, a whole new field known as functional MRI has arisen to apply these techniques. Because blood flow is altered in many pathophysiological states, from abnormal cognition through stroke to brain tumors, use of MRI to study blood flow is one of the most clinically relevant of the many forms of functional MRI. Dynamic susceptibility contrast, arterial spin labeling (ASL), and methods to measure permeability are the three techniques that have been used to quantify the perfusion of brain in many research and clinical applications. Rather than surveying the entire field of brain perfusion imaging, this article focuses on the use of perfusion MRI and, in particular, dynamic susceptibility contrast-enhanced MR imaging (DSC-MRI) to assess hemodynamics in meningiomas.
Basic Theory and Data Analysis of Dynamic Susceptibility Contrast-enhanced Magnetic Resonance Imaging
DSC-MRI, first described in 1991 by Rosen et al.,4 uses rapid measurements of MRI signal change after the injection of a bolus of a paramagnetic MRI contrast agent.5 This is the most commonly employed perfusion MRI technique and has been studied extensively in clinical settings. Gadolinium chelates with high magnetic susceptibility were used as contrast agents in DSC-MRI. Given their size and low lipophilicity, they are constrained to the intravascular space by a normal blood–brain barrier (BBB). These agents can be used as ‘tracers’ by injecting them as tight intravenous (IV) boluses and then imaging their initial passage through the brain vasculature. This requires larger-gauge IV catheters and higher injection rates (≥4ml/s), coupled with repeated rapid cine imaging of a volume of interest while the contrast passes through the capillary network. To record the tracer concentration during this passage faithfully, one must acquire images at a faster rate than the time it takes the bolus to pass through the tissue, which is usually in the order of several seconds. For DSC-MRI, this acquisition was commonly carried out by using a T2 (spin echo [SE]) or T2*-weighted (gradientenhanced [GE]) echo planar imaging (EPI) sequence.
Weisskoff and co-workers6–8 found that SE measurements are mainly sensitive to vessel sizes comparable to the water diffusion length during the time of echo (10μm), whereas GE measurements are equally sensitive to all vessel sizes. In practice, perfusion imaging performed using an SE approach requires twice the amount of contrast agent (usually 0.2mmol/kg) compared with imaging with GE-EPI (0.1mmol/kg). Furthermore, preliminary studies suggest that, in the brain, the microvascular CBV ‘visible’ by SE-EPI is roughly 45% of the ‘total’ CBV compared with measurements using GE-EPI.9
By detecting the arterial as well as the total tissue concentration as a function of time during a single transit, CBV can be determined from the ratio of the areas under the tissue and arterial concentration time curves.10 As arterial measurements (due to limited spatial resolution) are not readily quantifiable, relative CBV values are usually reported. Assuming uniform arterial concentration profiles in all arterial inputs, relative CBV measurements are determined by simply integrating the area under the concentration–time curve.11,12
Quantification of CBF and MTT, which are time-dependent parameters, is much more complex. The highest degree of quantification utilizes the deconvolution method and requires knowledge of an AIF. One must calculate the contrast concentration versus time curves from the signal intensity data. The area under the contrast concentration curve provides an estimate of CBV within the voxel, and the width of the contrast bolus is used as an estimate of the MTT of blood through the voxel. The regional CBF can then be calculated using the central volume theorem: CBF/CBV = MTT. Unfortunately, this approach to the measurement of CBF is subject to significant errors arising from a number of sources. These errors have led to modifications of the analysis method in an attempt to produce a more accurate, quantitative estimate of blood flow.
Absolute MTT values cannot be calculated because there are variables such as the dispersion of the contrast material following IV injection, cardiac output, and the precise amount of contrast entering and leaving a region of interest (ROI) at a given point in time that cannot be measured. The mean time to enhance (MTE) is related to the time to peak and to the width of the peak of the time–signal curve; MTE is computed and displayed only for the images between the last pre-enhancement image and the first post-enhancement image, equivalent to the bolus arrival time.
Among various perfusion parameters, regional CBV (rCBV) appears to represent regional variations in CBV accurately and is particularly used in the study of tumors.13 Some professional software can obtain half-quantified measurements of blood flow by using deconvolution techniques with an arterial input function; however, the intrinsic potential problems with this technique and consequent potential inaccuracies in quantitative measurements must also be considered.
Applications of Perfusion Magnetic Resonance Imaging in Meningiomas
There are two main types of brain tumor: primary brain tumors start in the brain, while metastatic brain tumors start somewhere else in the body and move to the brain. Meningiomas account for 30.1% of all primary brain tumors, making them the most common primary brain tumor.14
Brain tumors require a blood supply to grow and this in turn requires angiogenesis. More recently, angiogenesis has been recognized as a key element in the pathophysiology of tumor growth and metastasis.15 Once tumors grow beyond a diameter of 1–2mm, passive diffusion is no longer sufficient to support the viability of malignant cells, and neovascularization becomes a necessity.16 Therefore, tumors that grow beyond the occult stage are capable of activating the ‘angiogenic switch.’ The new blood vessels formed are generally less organized than the normal vessels and hence have altered perfusion characteristics with increased blood flow and volume.17–19
Meningiomas are highly vascular neoplasms and often show higher rCBV than other primary and metastatic brain tumors. Previous studies suggested that for meningiomas with atypical conventional MRI findings, calculation of rCBV ratios and construction of signal intensity–time curves may contribute to the differentiation of meningiomas from intra-axial tumors.20,21 Different meningioma subtypes also show different vascular characters. A study by Kimura et al. illustrated that among different subtypes of meningioma, perfusion values of angiomatous meningioma were the greatest and lowest for fibrous meningioma,22 and their results correspond to our experiences. By studying a group of 37 patients with newly diagnosed meningiomas, we found that the maximal rCBVs in both tumor parenchyma and peri-tumoral edema showed statistical differences between subtype meningiomas.23
In our results, from highest to lowest, the maximal rCBVs in tumor parenchyma were ranked as angiomatous, anaplastic, meningiothelial, and fibrous meningioma. In the peri-tumoral region, the maximal rCBV of anaplastic meningioma was highest, followed by fibrous, meningiothelial, and angiomatous meningioma.
When comparing the mean rCBVs of the two subtypes, our results showed that the maximum rCBVs in tumor parenchyma of angiomatous meningioma and in the peri-tumoral region of anaplastic meningioma were statistically greater (p<0.05) than those of other subtypes. From these studies, we presumed that some common benign subtypes of meningioma such as meningiothelial and fibrous meningiomas cannot be differentiated from atypical or anaplastic meningiomas simply by evaluating their parenchyma rCBV values. However, rare benign subtypes such as angiomatous meningiomas might show different perfusion characteristics.
Differentiating between malignant and benign meningiomas before surgery is important for both treatment planning and the prognosis appraisal. Although meningiomas do have some identifiable imaging features on conventional MR images, no special feature has been found to be reliable in predicting tumor grade. Sometimes, the aggressiveness of the tumor cannot be accurately characterized even on the basis of histopathological findings.24,25
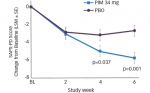
DSC perfusion MRI has also been used to assess the grade of meningiomas. However, the results of different studies are inconsistent. While Hakyemez et al.21 found that the rCBV of typical and atypical meningiomas were statistically different, Zhu et al.26 found no correlation between rCBV and tumor grade in two malignant and 12 benign meningiomas. In another study Yang et al.27 found no significant difference between the rCBV values of seven atypical and 15 benign meningiomas. In a series of 33 supratentorial meningiomas (25 benign and eight malignant), we measured the maximal rCBV (relative to the contralateral normal white matter) and corresponding relative MTE (rMTE) in the tumor parenchyma and peri-tumoral edema.28 While the maximal rCBV derived from the maximal blood volume regions in the parenchyma of benign meningiomas was higher than that of malignant meningiomas, the difference between the two showed no statistical significance. The rMTE in the parenchyma of both benign and malignant meningiomas were longer than those of normal brain tissue, but there was no statistically significant difference between benign and malignant meningiomas. We supposed these findings could be attributed to the immature and tortuous tumor vessels, which could result in increased leakage of contrast agent from vessels into the extravascular space and deceleration of blood flow in the tumor parenchyma. What is interesting in our results is that the maximal rCBV and corresponding rMTE of peri-tumoral edema of malignant meningiomas were significantly greater than those of benign ones (p<0.05). The increase in rCBV in the peri-tumoral edema of malignant meningiomas might be attributed to tumor invasion and angiogenesis in the adjacent brain tissue.29 Our results were also supported by previous molecular studies of meningiomas, which have shown that FLT1- and VEGF-positive cells are increased in the endothelium of intratumoral vessels and are associated with microvascular proliferations in peritumoral brain tissue of anaplastic meningiomas.30
Conclusion
DSC perfusion MRI can provide critical information on the vascularity of meningiomas that is not available with conventional MRI. DSC perfusion MRI measurements are helpful in the pre-operative subtyping and grading of meningiomas. Because of the limited patient numbers and the inconsistent results in published papers, perfusion MRI studies of meningioma with larger sample sizes are needed to investigate the reliability and reproducibility of this new technique before it can be used as clinical routine. ■