Huntington’s Disease
Huntington’s disease (HD) is an autosomal-dominantly inherited neurodegenerative disorder. It has a prevalence of 5–7 per 100,000 people in European and North American populations.1 The first symptoms typically appear between the ages of 35 and 45 years and include minor uncontrollable movements and personality changes such as depression and irritability.1
Huntington’s Disease
Huntington’s disease (HD) is an autosomal-dominantly inherited neurodegenerative disorder. It has a prevalence of 5–7 per 100,000 people in European and North American populations.1 The first symptoms typically appear between the ages of 35 and 45 years and include minor uncontrollable movements and personality changes such as depression and irritability.1
Initially, motor symptoms mainly involve the small distal muscles, but later on the larger postural muscles also become affected, resulting in the characteristic choreatic movements. Over the years, cognitive functions gradually deteriorate leading to impairments in memory and attention. Progressive weight loss and muscle wasting, despite sustained or even increased caloric intake, are also hallmarks of the disease.2–4 The end stage of the disease is characterised by rigidity, dystonia, dementia and cachexia. In most cases, HD results in death about 15–20 years after clinical onset. HD is caused by an expanded sequence of a cytosine-adenine-guanine (CAG) repeat located near the 5’ end of the first exon of the huntingtin (HTT) gene.5 Healthy individuals typically have fewer than 36 CAG repeats, and repeats of 40 or more cause HD with complete penetrance.5 Individuals with 36–39 CAG repeats are at risk of developing HD, but penetrance is often incomplete.6 There is an inverse association between the length of the mutant CAG expansion and age of onset, which is modulated by the size of the CAG repeat tract in the normal allele,7 as well as by other genetic and environmental factors.8,9
Autonomic Symptoms in Huntington’s Disease
Although less well-known, autonomic nervous system (ANS) dysfunction can also accompany HD.2 Indeed, vegetative symptoms indicative of ANS dysfunction have repeatedly been reported in patients with HD and include hyperhydrosis, micturition and swallowing difficulties,10–12 sexual dysfunction13 and complaints suggestive of orthostatic intolerance.14,15 Vegetative symptoms are most prominent in the advanced stages of the disease,16,17 but autonomic complaints such as dizziness following standing up, excessive perspiration and tachycardia can occur even in mildly disabled HD patients (i.e. Shoulson and Fahn stages I and II), as well as in otherwise asymptomatic gene carriers.18–20
By means of a questionnaire study, we recently systematically delineated the characteristics and frequency of autonomic symptoms in HD patients and premanifest mutation carriers in comparison with non-mutation carrying control subjects.20 We also assessed the relation between autonomic symptoms and various other clinical characteristics in order to identify important predictors of autonomic problems in HD patients. We found a range of autonomic symptoms in HD patients, particularly in the gastrointestinal, urinary, cardiovascular and male sexual domains, some of which were also present in premanifest mutation carriers.20 The largest differences between HD patients and controls existed for the frequency of swallowing/choking, erection and ejaculation problems, dysphagia and sialorrhoea (see Table 1). Other relatively prevalent autonomic symptoms in HD patients were early abdominal fullness, straining for defecation, faecal and urinary incontinence, urgency, incomplete bladder emptying and light-headedness while standing up. Of these symptoms, only swallowing difficulties, sialorrhoea, urgency, and erection and ejaculation problems were also more frequent in HD patients compared with premanifest mutation carriers.
Premanifest mutation carriers experienced significantly more swallowing difficulties and light-headedness on standing up compared with controls. Motor impairment, as defined by the motor subscore of the Unified Huntington’s Disease Rating Scale (UHDRS), was not significantly associated with the degree of autonomic dysfunction in HD patients, even when various autonomic domains were analysed separately. In fact, only functional indices, i.e. total functional capacity, functional assessment and independence score, appeared to be significantly associated with autonomic dysfunction in HD patients. Moreover, the severity of autonomic symptoms also positively correlated with depressive symptoms and use of antidepressant drugs. Interestingly, depressive symptoms were identified as the only independent predictor of the degree of autonomic dysfunction in HD patients, accounting for 32% of the variation.20
The most prominent autonomic complaints in HD patients concerned the gastrointestinal tract, including swallowing difficulties, dysphagia and sialorrhoea.20 These symptoms may partly be accounted for by skeletal muscle inco-ordination due to striatal pathology.11 However, the absence of an association between gastrointestinal symptoms and UHDRS motor score, as well as the relatively high prevalence of swallowing difficulties even in premanifest mutation carriers, suggests that ANS dysfunction is also likely to contribute to gastrointestinal problems in HD.20 This notion is further supported by the comparatively high prevalence of other symptoms in HD patients, including early abdominal fullness, straining for defecation, urgency, incomplete bladder emptying and postural dizziness, which cannot be ascribed to motor impairment alone.20 Nevertheless, although ANS dysfunction is likely to contribute to various vegetative symptoms in HD, other potential contributing factors, such as endocrine and peripheral abnormalities,2,21 cannot be excluded at this moment. Therefore, further studies simultaneously applying both subjective and objective measures, such as the composite autonomic scoring scale,22 should be undertaken to more accurately delineate the role of ANS dysfunction in the pathogenesis of the aforementioned symptoms in HD.
The association between autonomic symptoms and both functional disability and depression in HD patients is intriguing. Although it is difficult to differentiate between cause and effect, autonomic symptoms are unlikely to be secondary to functional impairment, as, by definition, autonomic functions are not under voluntary control. It is rather more likely that symptoms such as dysphagia, sialorrhoea, and faecal and urinary incontinence could lead to social embarrassment, isolation and a negative impact on daily functioning. On the other hand, the relation between autonomic dysfunction and depression, which is also found in, e.g., Parkinson’s disease,23 is harder to explain since depression itself can be accompanied by several vegetative symptoms such as loss of libido.24 In fact, depression has been shown to be the only independent predictor of autonomic dysfunction in HD patients, indicating that its effect on autonomic symptoms is independent of, e.g. functional disability. Although antidepressant use was correlated with the extent of autonomic complaints in HD patients, adjustment for the severity of depressive symptoms rendered this relation insignificant,20 suggesting that the association between depression and autonomic dysfunction is unlikely to be secondary to medication. Longitudinal studies of autonomic symptoms are needed to more precisely delineate the temporal association between depression and autonomic dysfunction in HD.
Autonomic Function Tests in Huntington’s Disease
Several studies have investigated ANS function in HD patients by means of a series of standardised tests, such as the blood pressure response to sustained handgrip,18,25 the pupillary light reflex latency,25 the orthostatic blood pressure test,18,25–27 heart rate variability at rest, during the Valsalva manoeuvre and upon postural change,25–28 and using the sympathetic skin response (SSR) test,25–27 the cold pressor test and the simple mental arithmetic task.19
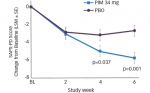
Compared with controls, the blood pressure response to sustained handgrip, a test of sympathetic function, was diminished in the patient group with a relatively long duration of disease.18,25 In contrast, the blood pressure response to sustained handgrip in a group of mildly disabled HD patients was elevated.18 The pupillary light reflex latency,25 as well as the SSR latencies,26,27 were prolonged in HD patients, suggesting parasympathetic and sympathetic dysfunction, respectively. The SSR amplitudes were also diminished in the patient group.26,27 Overall, patients showed lower heart rate variability (HRV) indices than controls.19,26–28 Spectral analysis of HRV, which yields several frequency bands of interest, suggested sympathetic hyperactivity in the premanifest gene carriers by a higher power of low frequency band (LFB; 0.04–0.15 Hz).18
Similarly, a higher power of LFB and an increase in the ratio between LFB and high frequency band (HFB; 0.15–0.40 Hz) was demonstrated in mildly disabled HD patients.18 LFB in the supine position reflects both sympathetic and parasympathetic activities and HFB reflects mainly vagal activity. A higher LFB/HFB ratio, which can be considered as a marker of sympathovagal balance, suggests a relatively higher cardiac sympathetic activity in the group of mildly affected HD patients.18 However, ANS hypofunction, predominantly parasympathetic dysfunction, was found in more advanced HD patients,18 and recently also in a group of moderately affected HD patients.28
Decreased heart rate variability in HD patients, as reflected by a high LFB/HFB ratio, may thus actually result from increased sympathetic activity, decreased vagal modulation or a combination of both.28 Therefore, further investigations are needed to elucidate which pathway is predominantly involved. Interestingly, the prolonged SSR latencies, smaller amplitudes and lower HRV detected in HD patients by some investigators seemed to closely correlate with various components of the UHDRS scores,26,27 suggesting that these measures may be useful as biomarkers to track disease progression.
Pathophysiology of Autonomic Dysfunction in Huntington’s Disease
The exact origin of impaired ANS function in individuals with HD remains to be elucidated. However, based on current knowledge, several possible explanations may account for autonomic dysfunction in HD. As there are no reasons to suspect damage to the peripheral nervous system in HD,18,26,27 the site of autonomic dysfunction is likely to be found in the central autonomic network including the hypothalamus and its connections to the cortex, limbic system, brainstem and spinal cord.29 Substantial hypothalamic pathology has indeed been found in both HD patients and animal models of the disease.2,30
Recently, a significant loss of dopamine D2 receptors, as well as microglial activation, was found in the hypothalamus of both HD patients and premanifest mutation carriers.31 As these abnormalities, as well as neuronal inclusions of mutant huntingtin, were seen throughout the hypothalamus,31,32 hypothalamic damage might account for the autonomic dysfunction that encompasses both sympathetic and parasympathetic functions.18,25–27 Alternatively, ANS dysfunction in HD, particularly sympathetic hyperactivity, might be interpreted as a release phenomenon due to diminished output from higher-order cortical regions to brainstem autonomic centers.19 Indeed, atrophic changes have been reported in the cortical regions that are involved in autonomic control, including the insular cortex and regions of the prefrontal cortex.33 Further studies combining autonomic functional tests with whole brain, and in particular hypothalamic, assessment are needed to more accurately pinpoint the sites of pathology within the central autonomic network in HD.
Management of Autonomic Complaints in Huntington’s Disease
Unfortunately, there are no clinical studies available that specifically address the management of autonomic complaints in HD patients. Therefore, at this stage, it is not possible to formulate evidence-based recommendations for the management of autonomic dysfunction in HD. However, various general (non-)pharmacological approaches for the treatment of dysautonomia are available which have been proven to be effective in other patient populations.34 In particular, the spectrum of autonomic complaints in patients with Parkinson’s disease largely overlaps with that reported by HD patients and, therefore, a similar approach may be effective in the latter group as well.35 For example, erectile dysfunction may be managed by sildenafil citrate, whereas botulinum toxin may be considered for the treatment of sialorrhoea.35 Whilst future interventional studies are needed to enable specific recommendations, clinicians should be aware of the high frequency of autonomic complains in HD patients and, until further data become available, manage these symptoms according to general approaches for the treatment of dysautonomias.34
Conclusion
In conclusion, autonomic symptoms are highly prevalent in HD patients and may even precede the onset of motor signs. As autonomic dysfunction is related to functional disability and depression in HD, increased clinical awareness and adequate management of autonomic symptoms in HD patients may lead to a considerable improvement of their quality of life. The precise origin of autonomic symptoms in HD remains to be elucidated, although pathology of the central autonomic network, including the hypothalamus, is likely to be involved. ■