Current medical care focuses primarily on symptom management, optimizing functions that are in continual decline, and the provision of ever-increasing levels of assistance. Symptomatic therapies using existing medications can help specific symptoms, such as depression, emotional dyscontrol, obsessive thinking, psychosis, chorea, rigidity, dysphagia, and weight loss. While medications, counseling, and rehabilitative modalities may improve the quality of life (QOL) for HD patients, there is no evidence that they appreciably slow the progression of the disease.To date, there is no clinically proven treatment for HD. The development of transgenic and knock-in mouse models of HD that replicate the phenotype observed in HD patients has been instrumental in identifying potential therapeutic candidates. Many potential therapies that separately target the previously mentioned mechanisms have now been tested in genetic models of HD, some of which significantly improved the clinical and neuropathological phenotype of HD mice and, as such, are immediate candidates for human clinical trials in HD patients since they are US Food and Drug Administration (FDA) approved compounds. This pre-clinical success been translated to early phase clinical studies in order to determine optimal dose ranges for HD patients and provide useful biomarkers.
Agents disrupting pathologic interactions of mutant huntingtin, either soluble or within aggregates, may target early pathogenic processes in HD. Proteolysis of mutant huntingtin and transglutaminase upregulation are thought to be proximal events in HD whereby abnormal and toxic fragments of huntingtin are released forming protein aggregates in neurons.These aggregates persist, indicating protein misfolding and failed proteolysis. In addition, transglutaminase upregulation catalyzes the formation of gamma-glutamyl isopeptide bonds between polyglutamine tracts, rendering the resulting cross-linked protein complexes insoluble. The resulting huntingtin aggregates sequester proteins including chaperones, proteasomal proteins, normal huntingtin, and transcription factors, which disturb protein homeostasis.
While the role of huntingtin aggregates continues to be debated, the evidence points to a proximal toxicity residing in mutant huntingtin, its proteolytic fragments, and their interactions with other proteins. Two such agents currently in clinical trials that inhibit mutant huntingtin aggregation and proteolysis are cystamine and minocycline, respectively. Cystamine is an aminothiol molecule that has multiple mechanisms of action through which it could counter some of the pathogenic cellular processes occurring in HD. Foremost, it is a potent inhibitor of transglutaminase. Cystamine also increases cellular levels of glutathione, an antioxidant that can provide protection from oxidative injury and may play a role in inhibiting apoptosis. Cystamine might also affect transcriptional dysfunction in HD secondarily by reducing sequestered transcription factors in insoluble huntingtin aggregates. While it is not certain which mechanisms are most important, cystamine clearly suppresses huntingtin protein aggregation and extends survival in HD mice. A safety and tolerability trial in HD patients using cysteamine, an analog of cystamine, is currently under way.1
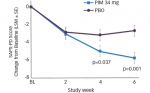
Minocycline, a second-generation tetracycline antiapoptotic compound, has been used for decades as an antimicrobial agent for rheumatoid arthritis (RA), acne, and rosacea, and is indicated for the treatment of infections. It has recently been shown to inhibit caspase activity. Mutant huntingtin undergoes proteolytic processing, in part by the pro-apoptotic enzyme caspase-3, releasing an N-terminal fragment that forms macromolecular aggregates with itself and other proteins. The caspase inhibiting function of minocycline reduces proteolysis of mutant huntingtin and the formation of cytotoxic N-terminal fragments and extends survival in HD mice. Minocycline is well tolerated and safe in HD patients. A recent clinical trial using minocycline in a small cohort of HD patients for 24 months showed stabilization of motor and neuropsychological functions, amelioration of psychiatric symptoms, and improved outcomes. An open-label, placebo-controlled multi-center, phase II, clinical trial using minocycline is in progress.2
Direct interactions between mutant huntingtin and transcription factors underlies transcriptional dysfunction in HD, perturbing cellular function and compromising protective mechanisms, ultimately leading to neuronal death and is therefore an important therapeutic target. An imbalance of repressing (methylation) and activating (acetylation) transcriptional influences affects subsets of critical survival genes and chronically stresses cellular homeostasis. Experimental studies show that transcriptionally active agents, such as aureolic acid antibiotics and histone deacetylase inhibitors, significantly ameliorate the phenotype in different models of polyglutamine disorders. These compounds have been used as chemotherapeutic agents, in which the anti-tumor properties are ascribed in part by selectively modulating gene expression/transcription.
One such compound, mithramycin A, is a DNA antibiotic that modifies and enhances DNA binding. The mechanism of action involves gene silencing, inhibiting methylation of histone H3 and, as such, improves the neuropathogenic outcome in HD models by partially restoring perturbed gene transcription. Mithramycin is significantly better than any other single compound to date in extending survival in HD mice. The author is actively pursuing safety and tolerability trials using mithramycin and its analogs in HD patients.
Histones are important nuclear proteins that help to regulate transcription. Histone acetylation, a marker of gene activation, is significantly decreased in HD. Histone deacetylases alter nucleosome structure locally and inhibit transcription. Histone deacetylases (HDAC) inhibitors can promote transcription activation by relaxing DNA conformations, improving histone acetylation. While a number of HDAC inhibitors are currently under development, such as anti-cancer drugs, the butyrates are the most developed for clinical use in humans. Experimental findings in HD mice show efficacy using both sodium butyrate and sodium phenylbutyrate in slowing the clinical symptoms and reducing the neuropathological sequela. Phenylbutyrate is currently the most feasible for testing in HD because of the preponderance of pharmacokinetic, toxicity, and dosing information available about this compound. It has been safe and well tolerated in several clinical studies for cancer. The pre-clinical findings of increased efficacy in HD mouse models provided the rationale for beginning clinical testing of HDAC inhibitors in HD patients. A multi-center, doubleblind, placebo-controlled study with open-label follow-up to determine the safety and tolerability of phenylbutyrate in HD patients is under way.
A number of studies in HD patients and HD model systems have validated mitochondrial dysfunction/ energy insufficiency and oxidative stress pathways as promising therapeutic targets. Energy is critical to the biological and molecular regulation of multi-cellular functions and, as such, reduced energy levels threaten cellular homeostasis and integrity. Compounds such as creatine and coenzyme Q10 (CoQ10) buffer neuronal energy demands and are attractive candidates for targeting these important disease mechanisms. Creatine levels are reduced in HD. Creatine is present as free creatine or phosphocreatine (PCr). PCr provides an energy buffer to re-phosphorylate adenosine diphosphate (ADP) to adenosine triphosphate (ATP) at sites of energy consumption (creatine phosphate (PCr) shuttle hypothesis). Creatine administration increases brain concentrations of PCr. If the recovery of PCr is dysfunctional in HD patients or if energy stores are diminished, then creatine supplementation may augment PCr production and provide neuroprotection in HD patients.
Previous studies have demonstrated the neuroprotective effects of creatine in in vitro and in vivo models of neurological diseases, particularly HD. Creatine is safe and tolerable in HD patients, resulting in increased brain concentrations, and may be effective in stabilizing disease progression. The safety of chronic administration over a long period of time has yet to be established. In addition, it remains unclear whether optimal creatine dosing has been determined. It may well be that higher doses of creatine (30–40g per day) are necessary to significantly slow the disease process. Consequently, a dose escalation study to determine whether there is a maximally tolerated dose in HD, as well as whether there are doses at which serum and brain levels of creatine are maximized, has been initiated.
CoQ10 has also been shown to be effective in slowing the progression of neurological phenotypes, as well as ameliorating neuronal damage in experimental models of HD. CoQ10 is essential for complexes I and II electron transfer activities during oxidative phosphorylation. CoQ10 shuttles electrons from complexes I and II to complex III and plays a vital role in ATP production. CoQ10 also has membrane-stabilizing properties and acts as an antioxidant. The therapeutic rationale includes targeting improved cellular energy production and reducing oxidative stress. CoQ10 is efficacious in animal models of HD.Treatment with CoQ10 in HD patients showed a trend toward slowing functional decline and a trend toward a beneficial effect on cognitive tests and behavior. It has recently been suggested that higher doses of CoQ10 may provide greater efficacy in treating neurodegenerative diseases. CoQ10 has recently been shown to be efficacious in early Parkinson’s disease (PD). CoQ10 is relatively safe for long-term exposure. A CoQ10 dosage of 2,400mg has been chosen for use based on dosage ranging tolerability studies performed in HD. A double-blind, placebo-controlled, randomized, multi-center study using CoQ10 at 2,400mg per day was being planned at the time of press in HD patients.
There is evidence that NMDA receptors and postsynaptic signaling are altered in HD, resulting in excitotoxicity, and may represent potential therapeutic targets. Amantadine, a non-competitive NMDA receptor antagonist, and riluzole, an inhibitor of glutamate release, have been shown to reduce dyskinesias, while remacemide, an NMDA receptor antagonist, did not show significant benefit in HD. In addition, lamotrigine, an anti-epileptic that also inhibits glutamate release, was not efficacious. Current support for targeting glutamatergic synaptic modulation as a potential target in HD is not enthusiastic given the weak/equivocal results of tested therapies.
While recent experimental evidence suggests that ribonucleic acid interference (RNAi) may be a potential therapeutic strategy for treating HD, selective gene silencing faces significant methodological and molecular challenges before it enters human clinical trials.
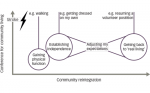
An important implication of the multiple levels of molecular pathology and treatment in HD is that it will most likely be necessary to combine neuroprotective therapies to maximize neuroprotection and reach the greatest efficacy.