Every year, more than 15 million people worldwide suffer from a stroke, making it the third most common cause of death in developed countries.1 Another serious aspect of stroke is that 50 % of stroke survivors remain long-term disabled causing limited mobility and dependency in activities of daily living (ADL).1 Considering the established claim of the International Classification of Functioning, Disability and Health (ICF), 2 the central approach of neurological rehabilitation must be to enable patients to participate in personal and occupational life by decreasing their dependency in the performance of ADL and increasing patient’s mobility. 3
Countries differ profoundly in the way they organise stroke rehabilitation. Nevertheless, half of patients still need help with ADLs 3 months post stroke even in countries with well-established nationwide rehabilitation programmes. 4 Therefore, in the last few years, the scientific community developed new therapy regimes, 5,6 to increase and decrease excitability of functionally re-organised brains, such as non-invasive brain stimulation techniques like transcranial direct current stimulation (tDCS) or repetitive transcranial magnetic stimulation (rTMS). 7,8 In addition, the course of recovery can be accelerated by paralleling physiotherapy with the application of drugs. 9
But still, the way rehabilitation therapy is applied to stroke patients is mostly based on therapists’ experience and epidemiological data. The success of the therapy could be substantially increased by incorporating knowledge over the patient’s functional brain organisation after stroke. In the following article we will explain this thought in relation to the human action–observation system and networks involved in mirror training (MT).
The Human Action–Observation System
The human action–observation system (also named the human mirror neuron system [MNS]) is derived from ‘mirror neurons’ within area F5 of the ventral premotor cortex (vPMC) of monkeys. With the use of single neuron recording a class of neurons with ‘mirror’ character was discovered: these neurons are active during both goal-directed action (motor performance) and observing the same motor act (visual information without any active movement) 10–12 as well as during hearing of a specific motor act. 13 Activation of the premotor cortex (vPMC) during observation of a goal-directed action is a specific form of brain organisation, which is of particular interest in stroke rehabilitation. Due to the close anatomical connection between premotor cortex and primary motor cortex (M1), merely observing a goal-directed action is sufficient to induce higher excitability in M1. 14 Many stroke patients with a lesion of the pyramidal tract and consequently with a paresis of arm/hand are unable to increase their output from M1. By activation of the premotor cortex via MNS – with pure visual information from observation of a video demonstrating a goal-directed action – an excitability increase and a reinforcement of the primary motor cortex is possible. Ertelt and colleagues15 showed that action observation via video (videotherapy) in association with physiotherapy is superior to sole physiotherapy of stroke patients. The development of videotherapy was based on the assumption that the observation of a goal-directed action activates its neuronal motor representations particularly the premotor cortex, among others. 16–20 It must be considered that direct evidence of mirror neurons in human PMC is still absent. Yet, many functional magnetic resonance imaging (fMRI) studies find a network of parieto-frontal regions (including the premotor cortex) which are active during both observation of goal-directed movement and during active performance of goal-directed action. 21–23
Relatively easy implementation is one of the great advantages of videotherapy: the treatment can be administered as a home-based training programme. An individualised set of videos can be given to the discharged patient to continue exercises at home at comparably low economic cost. But one has to bear in mind that with the knowledge that the parieto-frontal functional interaction is relevant for action observation and videotherapy, it is assumable that stroke-related affection of this network causes a non-beneficial course when this therapy is applied. That means the knowledge of functional organisation after stroke could be a generator for the choice or non-choice of a specific therapy regime.
Mirror Therapy
While an active movement is needed to improve hand/arm function in association with observation of goal-directed movement (videotherapy), many patients are not able to move their hand or are not able to perform a hand grip. The specific brain information processing of the illusionary hand movement, which is behind the mirror while the other hand is moving (MT), is also of particular interest for rehabilitation of these specific stroke patients with almost no hand and finger movements.
In MT a mirror is positioned orthogonally in front of the centre of the patient’s body. The less-affected (healthy) extremity is moved and observed in the mirror (see Figure 1).
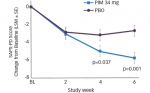
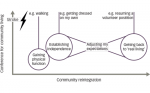
Ramachandran and colleagues24 are pioneers in the field of MT and were the first to use it to reduce phantom pain after amputation of an extremity. From that time, studies also described the effect of MT in patients suffering from other pain syndromes, for example with complex regional pain syndrome (CRPS) in combination with imagination of extremity movement. 25 MT increases range of motion, speed of action and accuracy of some stroke patient’s paretic arm. 26 In the last years several clinical randomised controlled trials investigated the effect of MT. However, different results were reported presumably due to variable study designs. In two studies arm and leg function showed greater functional improvement after MT compared with a therapy without a mirror. 27,28 In another study, the control group, receiving 50 % more occupational therapy time than the intervention group did not show any significant differences in the hand function in comparison to the MT group. But patients with a hand plegia benefited significantly more from MT compared with the control group. 29 Michielsen and colleagues30 investigated home-based MT 1 hour per day 5 days per week for 6 weeks. The hand function in the MT group increased after the 6 weeks training period compared with the control group. Six months later there was no difference between both groups. It is ambiguous whether or not patients continued training by themselves between the end of the 6 weeks training period and 6 months later. Although, a meta-analysis provided evidence for the positive effectiveness of MT; 31 others emphasised that not all patients benefit from MT. 32 Thus, the question is which patients would benefit from MT for the best individual outcome? To select MT as an effective rehabilitation application, the first way is to understand which specific brain networks are involved in MT. Then, the knowledge whether these networks are disrupted by the lesion is the generator for choice or rejection of MT. Despite the choice of the best-matched therapy regime, it must be considered that other factors also affect the recovery process after stroke, such as the patient’s intrinsic motivation and a supportive social environment. These factors are hard to control therefore we did not consider them in the following.
As an example, a recent study investigated neuronal networks involved in MT. 33 Two groups with healthy subjects trained the same tasks with their right hand. The first group (intervention group, mirror group) performed the task by looking in the mirror. In the second group (control group), a board instead of the mirror was positioned orthogonally to the centre of the patients’ body and the task was performed by looking straight forward (see Figure 2). In both groups, the left hand was immobilised. After several training days, the left hand of the mirror group showed better test results compared to the control group.
With the use of fMRI the training-induced plasticity between the two groups was compared. Training with a mirror increased functional interaction between medial premotor regions (supplementary motor area [SMA]) with lateral premotor areas as well as with the primary motor cortex (M1) contralateral to the trained right hand (see Figure 3). SMA activation was suggested to be a result of the illusory bimanual hand movement. It could be assumed that observing the right hand movement in the mirror with the impression the left hand is being moved represents an illusionary bimanual movement, which leads to SMA activation.
The lateral premotor cortex activation could be based on the human action-observation network during the observation of their own hand in the mirror, which is involved in MT.
Knowing which parts of the network are involved in training-induced plasticity of MT, it now becomes possible to predict the benefits of MT depending on the identification of the patients’ lesion.
The following example in Figures 4 and 5 shows two chronic stroke patients (stroke occurrence was more than 2 years before starting MT): patient A benefited from MT with a better hand function after training. His lesion is outside the certain regions of MT-related network (see the white mark up in Figure 4). Therefore, training-induced plasticity is attainable in the associated MT-related network.
Patient B’s lesion is located within the MT-related network, therefore no plasticity occurred and his hand function did not improve with MT.
Conclusion
Considering higher stroke incidence with demography development and the importance of stroke related socio-economic factors, highly efficient therapy of disability after stroke is required.
MT is a relatively new approach to force motor recovery after stroke, but not each patient will benefit from MT. Therefore, we need an individualised therapy regime. For this way, predictive factors can help in decision-making of the right individualised therapy regime. We also need further innovations in the field of stroke recovery research.