The clostridial neurotoxins (CNTs) (tetanus toxin [TeNT] and seven serologically distinct botulinum neurotoxins [BoNT/A–BoNT/D]), are among the deadliest agents known. They are bacterial enzymes produced by anaerobic, spore-forming bacteria of the genus Clostridium. Each toxin is composed of a heavy chain (HC) and a light chain (LC) linked via a disulfide bond. CNTs bind to high-affinity surface neuronal receptors, mediated by their HCs. The receptors are composed of polysialic gangliosides in conjunction with proteins presented by recycling synaptic vesicles (SVs). Following entry into neurons via recycling SVs, acidification of the vesicle triggers the translocation of the LC into the cytosol, where it cleaves essential components of the vesicle fusion machinery (neuronal soluble ethylmaleimide attachment receptors [SNAREs]). It is widely assumed that BoNT/A remains at the synaptic terminal and its effects are confined to the injection site. BoNT/A inhibits synaptic transmission near the site of injection; local effects at the neuromuscular junction (NMJ) result in flaccid paralysis. Antonucci et al. showed that catalytically active BoNT/A is retrogradely transported by central neurons and motoneurons and is then transcytosed to afferent synapses, in which it cleaves SNAP-25.1 SNAP- 25 cleavage by BoNT/A was also observed in the contralateral hemisphere after unilateral BoNT/A delivery to the hippocampus. Aoki et al. believed that this was due to a high dose of a research toxin, unreported antibody specificity, and the lack of reported controls for nonspecific protein transport and detection methodology.2
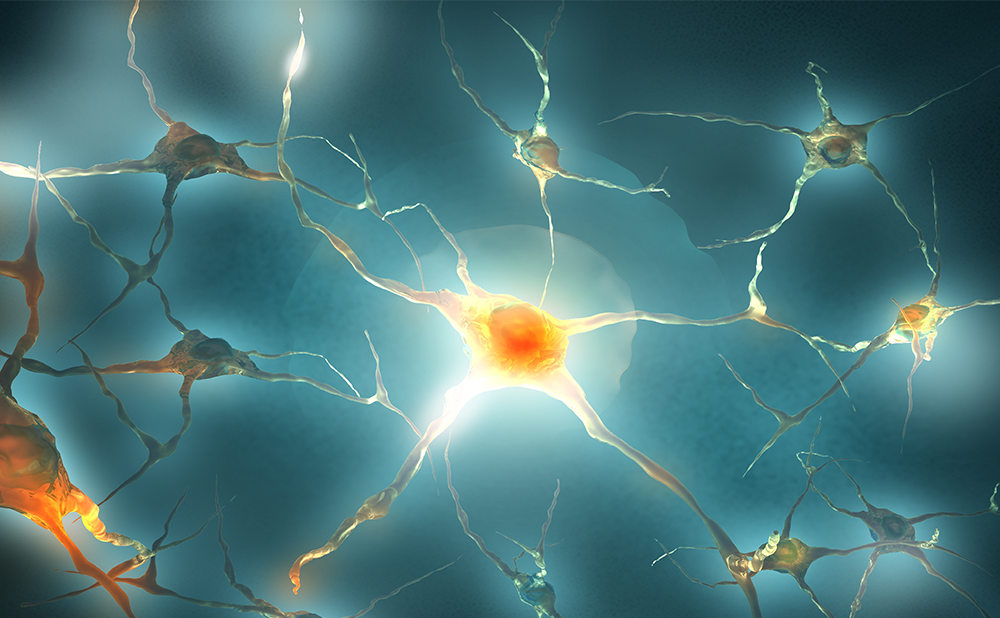
Now Bomba-Warczak et al. present additional evidence that toxins can spread within networks of neurons to have distal effects, and might be transferred between neurons.3 They investigated the potential distal effects of BoNT/A, BoNT/D, and TeNT using central neurons grown in microfluidic devices. Rat hippocampal neurons were seeded in one macrochannel (soma chamber). Axons projected through the microchannels to the opposing macrochamber (axon chamber). For toxins to go to the soma side from the axon side, and to be released in an active form, the LC must remain linked to the HC. This can occur if the toxin is in a non-SV compartment that does not undergo significant luminal acidification. The authors found that toxins not only can enter the SV2-dependent pathway, which leads to local effects and results in substrate cleavage throughout the cell, but they can enter via an alternative receptor pathway, which leads to distal effects. The alternative pathway relies on non-acidified organelles that mediated retrograde transport to the somatodendritic compartment. Toxins were then released into the media, where they entered and exerted their effects upon upstream neurons. These findings directly demonstrate that these agents undergo transcytosis and interneuronal transfer in an active form, resulting in long-distance effects.
In conclusion, BoNT/A, BoNT/D, and TeNT enter neurons via two separate entry pathways: a canonical synaptic vesicle recycling pathway that leads to local effects, and a distinct secondary uptake pathway that directs these toxins to a common, non- acidified, retrograde carrier. This secondary pathway leads to distal effects in neurons upstream from the cells that mediate the initial uptake of these agents.