Restless legs syndrome (RLS) is a common but frequently unrecognised condition characterised by uncomfortable and unpleasant sensations in the legs and an urge to move.1 The symptoms begin or worsen during periods of rest or inactivity, and they are relieved by activity.2 This relief generally persists for as long as the activity continues.
Restless legs syndrome (RLS) is a common but frequently unrecognised condition characterised by uncomfortable and unpleasant sensations in the legs and an urge to move.1 The symptoms begin or worsen during periods of rest or inactivity, and they are relieved by activity.2 This relief generally persists for as long as the activity continues.
Another central characteristic of RLS is the worsening of symptoms in the evening or during the night.1 Studies that have investigated circadian patterns in RLS occurrence have shown that the severity of leg discomfort follows a circadian rhythm, with a maximum occurring after midnight and a minimum occurring at 10:00am.3 Even if the underlying neurobiology of RLS is still not fully understood, the most accredited hypothesis recognises involvement of the diencephalic A11 dopaminergic neurons.4 These dopaminergic cells seem to be able to modulate the nociceptive afferents by means of their projections into the dorsal horns of the spinal cord.5 Specific lesions in A11 nuclei of mice induced some features similar to those of human RLS, with a long latency of sleep, reduced sleep time and several episodes of standing upright.5
The majority of RLS patients complain of poor sleep.6 Most patients report difficulty falling asleep since both immobility and circadian factors facilitate the occurrence of RLS symptoms at bedtime.3 However, some patients fall asleep rapidly but wake up shortly after with unpleasant leg sensations that force them to get up and walk around in order to alleviate the symptoms.3
Sleep laboratory investigations have shown that more than 85% of patients with RLS also experience stereotyped repetitive movements once asleep, a condition known as periodic limb movements during sleep (PLMS).3 PLMS are characterised by rhythmical extensions of the big toe and dorsiflexions of the ankle with occasional flexions of the knee and hip. A PLMS index (number of PLMS per hour of sleep) greater than 15 for the entire night of sleep is considered pathological.1 In addition to PLMS, RLS patients show also PLM during wakefulness, known as PLMW.3
RLS can occur in all ethnic backgrounds. Epidemiological studies have shown that Caucasians are most affected.7 Most Caucasian surveys show an approximate 10% prevalence, while surveys from south-eastern Europe and Asian populations report much lower prevalences. A rate of 3.2% has been reported in Turkey,8 3.9% in central Greece9 and 0.6% in Singapore.10 In an epidemiological survey conducted in the US and five European countries,11 RLS symptoms of any frequency were reported by 7.2% of the general population: symptoms occurred at least two times per week and were reported as moderately or severely distressing by 2.7%. These subjects were defined as RLS sufferers and probably required treatment.
Primary or secondary forms may be recognised in RLS.3 In the primary forms, there is substantial evidence of a genetic contribution to RLS. Familial aggregation has been well documented, with about 50% of idiopathic cases reporting a positive family history of RLS: in most pedigrees, it segregates in an autosomal dominant fashion, with a high penetrance rate (90–100%).12
Linkage studies in RLS families have revealed eight loci, but no causally related sequence variant has been identified using this approach.12 A recent genome-wide association study of RLS identified common variants in three genomic regions: MEIS1, BTBD9 and MAP2K5 on chromosomes 2p, 6p and 15q, respectively.13 Each genetic variant was associated with a greater than 50% increase in the risk of RLS. MEIS1 has been implicated in limb development, raising the possibility that RLS has components of a developmental disorder.13 A genome-wide significant association with a common variant in an intron of BTBD9 on chromosome 6p was found independently in the Icelandic population.14 An association between this variant and PLMS without RLS (and the absence of such an association for RLS without PLMS) suggests that it is a genetic determinant of PLMS.14
The most common causes of secondary RLS are iron deficiency, end-stage renal disease and pregnancy.1–3 Peripheral neuropathies of different origin, diabetes and multiple sclerosis have been seen at higher than expected frequencies in RLS patients.15–17 Moreover, RLS has been reported as an adverse event resulting from treatment with several drugs.18 The majority of published papers focusing on this issue are case reports, but in a recent prospective study that addressed this problem for the class of second-generation antidepressants, RLS was observed in 9% of patients.19
Pharmacological Treatment of Restless Legs Syndrome
Pharmacological treatment should be limited to those patients who suffer from clinically relevant RLS symptoms, including intermittent RLS with impaired sleep quality or quality of life.12,20 Dopaminergic agents are considered first-line treatment.3,20
Several open-label studies have documented the short-term efficacy of levodopa given with a dopa-decarboxylase inhibitor.3 Dosages of standard levodopa of between 100 and 200mg improve RLS symptoms as measured on a visual analogue scale.21 Levodopa is a short-acting medication, and the immediate response without a long titration period is appreciated by patients.3 However, a possible side effect of levodopa is morning rebound, characterised by the presence of RLS symptoms occurring de novo as a consequence of evening or night-time treatment.3 With levodopa, it is also possible to observe a rebound of PLMS in the later part of the night, if levodopa is administered only at bedtime.3 However, the most relevant clinical side effect of levodopa therapy is augmentation.22 Augmentation is a phenomenon characterised by an earlier onset of symptoms by at least four hours, or an earlier onset by between two and four hours plus at least one of the following compared with symptom status before treatment: shorter latency to symptoms when at rest; extension of symptoms to other body parts; greater intensity of symptoms; and shorter duration of relief from treatment.22 Augmentation is probably triggered by intense dopaminergic stimulation of the D1 receptor compared with the D2 and D3 receptors, predominantly at the spinal level.23 It has recently been shown that iron deficiency and sleep deprivation may increase the risk of augmentation.23 Prevalence rates of augmentation in open-label trials with levodopa range from 18.6 to 82%.24 A recent study showed augmentation in 36 of 60 patients (60%) treated for six months with levodopa (median daily dose 300mg).25 Increased severity of RLS and higher dosage of levodopa are associated with higher risk of developing augmentation: maximum dosages of 300–400mg should not be exceeded.20
Several double-blind controlled studies have shown that both ergoline (cabergoline, pergolide) and non-ergoline (ropinirole, pramipexole, rotigotine) dopamine agonists are able to control RLS symptomatology.12 In a short-term follow-up study, the D2 receptor agonist bromocriptine was found to be effective in treating RLS and PLMS.26 However, bromocriptine is frequently associated with severe adverse effects, especially nausea.27 Pergolide, another D2 receptor agonist, has been more extensively studied and its efficacy has been well-documented in short- and long-term follow-up studies.28,29 An open follow-up of a controlled study in 28 RLS patients showed that the beneficial effect of pergolide persisted for at least one year in 22 patients (79%): five subjects (18%) discontinued medication, predominantly because of nausea, and six (21%) developed augmentation.29 Cabergoline, a longacting D2 receptor agonist, was also used successfully to treat RLS, and the beneficial effects of a low dose of drug (mean dosage 2.2mg) on symptoms has been demonstrated to persist for up to one year.30 A recent controlled study with cabergoline showed a frequency of augmentation of 4%.31
Retroperitoneal, pericardial and pleuropulmonary fibrosis are well known but rare complications of treatment with ergolinic dopamine agonists.32 Recently, two studies also showed that pergolide and cabergoline were associated with an increased risk of cardiac-valve regurgitation compared with non-ergot-derived dopamine agonists.33,34
In the last few years two non-ergoline-derivative agonists, pramipexole and ropinirole,12,20 have been extensively studied for RLS treatment. A recent double-blind, placebo-controlled study confirmed the efficacy of pramipexole, a full agonist with high affinity for the D3 receptor subtype, at a median dose of 0.35mg/day.35 In a long-term follow-up study, of 78% of patients who took pramipexole for more than a year, 96% showed sustained improvement in their RLS symptom severity after a mean 30 months of treatment.36 Augmentation with pramipexole was reported in open trials, ranging from 8.3 to 39%.37–39 Some randomised, placebo-controlled trials have shown that ropinirole is also effective for the treatment of RLS.27 A long-term open-label study over 52 weeks showed that ropinirole (mean dose 1.90mg/day) maintained therapeutic efficacy in 83% of RLS patients as measured by the clinical global impression (CGI) scale.40 There have been no reports of augmentation in the published studies, but the phenomenon has not been systematically assessed.20
Sleepiness associated with sudden onset of sleep was reported in patients with Parkinson’s disease (PD) treated with pramipexole and ropinirole.41 In RLS patients, sleepiness might be seen during treatment with dopamine agonists, but is much less problematic;3 moreover, the use of these compounds in RLS may, in contrast to PD, reduce the risk of sudden onset of sleep, probably due to their beneficial effect on sleep.42 Striatal and limbic dysregulation have been suggested in PD as putative factors in compulsive behaviours arising from dopamine agonists.43 Recently, behavioural complications, such as pathological gambling and punding, have also been reported in some RLS cases under dopaminergic treatment.44
Opioids may be prescribed for severe cases of RLS, especially in patients unresponsive to other treatments.20 Although there is little evidence of tolerance of or addiction to opioids in the RLS literature,20 the prescription of these compounds should be restricted to patients without a previous history of substance abuse.
A subjective improvement of RLS with gabapentin at doses of 200–2,000mg/day has been reported in some open-label trials and one placebo-controlled study.27 As shown in a six-week placebo-controlled study, gabapentin has a good side-effect profile.45 Other anticonvulsants, such as carbamazepin and valproic acid, have been evaluated in RLS but seem to be less effective than gabapentin.20
Rotigotine – A New Non-ergot Dopamine Agonist
Rotigotine is the levorotary enantiomer of a racemic aminotetraline compound with structural similarity to dopamine. It is a non-ergot agonist of all dopamine receptors (D1–D5), with the strongest affinity for D3 receptors.46 Its bioavailability after oral ingestion is very low due to extensive gastrointestinal metabolism.47 High lipid solubility makes rotigotine an ideal candidate for transdermal application. Recent experimental data on pharmacokinetics with the patch show that rotigotine has the potential to induce continuous dopamine receptor stimulation.48 Rotigotine, as a transdermal patch, is absorbed through the skin by transcellular, intercellular (lipophilic) and follicular (hydrophilic) routes.49 After transdermal application, the drug reaches the systemic circulation with a lag-time of two to three hours, and maximum plasma concentration is reached after 16 hours.50 In healthy subjects treated with a dose of 4mg/24 hours for a period of 14 days, plasma level analysis showed a stable level after two to three days, consistent throughout the subsequent treatment period without accumulation or change in clearance.51 Dose adjustment due to age, gender, weight or renal or hepatic impairment is not necessary.52 Moreover, rotigotine showed no effects on CYP450 enzyme activity in in vitro and in vivo studies, indicating a low risk of drug–drug interactions.53
Rotigotine for the Treatment of Restless Legs Syndrome
In the last few years, from January 2004 to December 2009 (PubMed database), four studies on rotigotine in RLS have been published.54–57 These four European studies included one proof-of-principle study (one week duration), one placebo-controlled six-week dose-finding study, one placebo-controlled six-month study and a one-year open-label study (see Table 1). Currently, most of the available publications on rotigotine concern the clinical effects in PD.27
Stiasny-Kolster et al. performed the first trial by using three fixed doses (0.5, 1 and 2mg/24 hours) of rotigotine in 63 patients with idiopathic RLS who had discontinued other RLS medication four weeks before enrolment.54 The authors reported that after one week of therapy, as measured using the International Restless Legs Syndrome Scale (IRLS), there was a significant dose-related improvement in restless leg symptoms from baseline scores (baseline range: 25.0±5.0–26.6±5.0). For the 0.5, 1 and 2mg/24 hours doses, improvements in IRLS were -10.5 (0.5mg/24 hours; p=0.41), -12.3 (1mg/24 hours; p=0.18) and -15.7 points (2mg/24 hours; p<0.01) compared with 8 points for placebo.
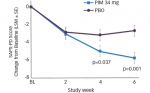
A few years later, Oertel et al., in a multicentre, double-blind, placebo-controlled dose-finding study with dosages of rotigotine ranging from 0.5 to 4mg/24 hours, confirmed a dose-dependent effectiveness in idiopathic RLS patients.55 The authors randomly assigned 341 patients to one of five fixed dosages of rotigotine (0.5, 1, 2, 3 or 4mg/24 hours) or to placebo for six weeks. The chosen outcome measures were the total score of the IRLS, the RLS-6 scale, the CGI, the Epworth Sleepiness Scale (ESS) and the Quality of Life questionnaire for RLS (RLS-QoL). At baseline the IRLS score in the six treatment groups ranged from 27.4±6.1 to 28.2±6.6. The improvement in the IRLS score was related to the dosage of rotigotine, with the following values: -10.6 (0.5mg/24 hours), -15.1 (1mg/24 hours), -15.7 (2mg/24 hours), -17.5 (3mg/24 hours) and -14.8 (4mg/24 hours) compared with placebo (-9.2). Rotigotine was significantly superior to placebo for all dosages except for 0.5mg/24 hours. Similar results were obtained by the CGI. Since the efficacy of the lowest dose of 0.5mg/24 hours was not proved, and the highest dose (4mg/24 hours) lacked additional benefit, the authors identifed the therapeutic range for a maintenance dose of rotigotine to be 1–3mg/24 hours. The same authors prospectively tested the long-term efficacy and safety of rotigotine (0.5–4mg/24 hours) in a five-year open extension of the six-week trial. In a one-year interim analysis, the results from 295 of the original 341 patients with idiopathic RLS were reported. After one year of treatment, 220 patients remained in the follow-up study, with a retention rate of 74.6%.57 The mean daily dose of 2.8±1.2mg/24 hours improved the IRLS score by 17.4±9.9 points from a mean baseline score of 27.8±5.9 points. The most frequently applied dose was 4mg/24 hours, in 40.6% of patients. The rotigotine patch was well tolerated by the majority of patients. The long-term efficacy of rotigotine was also confirmed in terms of quality of life and sleep satisfaction.
Of the four trials listed in Table 1, the multicentre randomised, doubleblind, placebo-controlled trial by Trenkwalder et al. included the most patients.57 A total of 458 patients with moderate to severe idiopathic RLS were randomised to receive 1, 2 or 3mg/24 hours of rotigotine or placebo for six months. At baseline, the mean IRLS score was 28.1. The mean improvement in this score from baseline at the end of the study was significant in a dose-dependent fashion: -13.7 in the 1mg group, -16.2 in the 2mg group, -16.8 in the 3mg group and -8.6 in the placebo group. Similar dose-related improvements were obtained by using CGI (CGI-item 1 [severity of symptoms]: -2.09 in the 1mg group, -2.41 in the 2mg group, -2.55 in the 3mg group and -1.34 in the placebo group) and the quality of life questionnaire. An IRLS sum score of 0 at the end of the maintenance phase, which indicated freedom from disease symptoms, was recorded for 79 of 333 patients (24%) in the rotigotine groups (21 of 112 [19%] in the 1mg group, 23 of 109 [21%] in the 2mg group and 35 of 112 [31%] in the 3mg group), compared with 14 of 114 patients (12%) in the placebo group.
Another six-month double-blind trial has been performed in the US and published in abstract form.58 Five hundred and five patients with moderate to severe RLS were randomised to fixed dosages of 0.5, 1, 2 or 3mg/24 hours rotigotine transdermal patch or placebo. After uptitration to the randomised dosage, allowing for one backtitration in case of intolerable side effects, patients were maintained on a stable rotigotine dosage for six months. Efficacy analysis showed significant improvement on IRLS sum scores as well as CGI item 1 (severity of symptoms) for rotigotine doses of 2–3mg/24 hours. At baseline, the IRLS score was 23.3±5.0 and CGI Item 1 was 4.7±0.7. After six months of 0.5, 1, 2 and 3mg/24 hours rotigotine or placebo treatment, respective net improvements in IRLS compared with placebo were -2.2±1.2, -2.3±1.2, -4.5±1.2 (p<0.001) and -5.2±1.2 (p<0.001), and net improvements for CGI Item 1 compared with placebo were -0.35±0.19, -0.32±0.19, -0.65±0.19 (p<0.001) and -0.90±0.19 (p<0.001).
Apart from the clinical efficacy findings mentioned above, a sleep laboratory study evaluated PLM index (PLMI) and the PLMI associated to arousals (PLMSAI).59 This trial, which randomised a total of 67 patients, in comparison with the previous fixed dosage studies, included titration to an optimal rotigotine dose of between 1 and 3mg/24 hours, followed by a four-week maintenance period. Polysomnography was performed at baseline and at the end of the maintenance period, with a significant drop in PLMI score in the rotigotine recipients. The PLMSAI score also improved to a greater extent in the rotigotine group than in the placebo group. At the end of maintenance treatment, the PLMI had decreased from 50.9 at baseline to 8.1 for rotigotine versus 37.4 to 27.1 for placebo. The IRLS score in the rotigotine group was reduced from 26.3±6.4 to 9.7±9.1 and in the placebo group from 25.4±6.3 to 15.1±8.3 (p<0.02). Twenty-six per cent of rotigotine-treated subjects had an IRLS score of 0 (no RLS symptoms).
Concerning safety and tolerability, all studies showed that rotigotine transdermal patch was generally well tolerated by patients with moderate to severe RLS.54–57 Most adverse events were of mild to moderate severity, including the symptoms usually associated with dopaminergic side effects such as nausea, fatigue, insomnia, dry mouth, dizziness and vertigo. Across all trials, the most common drug-related adverse event was skin irritation at the application site. This adverse event was reported in 43% of patients in the six-month European trial,57 in 40% in the one-year open-label extension study56 and in 54% in a three-year open-label extension study.60 Discontinuation of treatment due to skin irritation was reported in approximately 13% of patients in the one-year extension study.56 The use of dopamine agonists in PD may sometimes be restricted by the appearance of psychiatric side effects such as hallucinations, delusions or impulse control disorders;61,62 however, information on these side effects was not included in these publications.
Recently, a specific scale for measuring the phenomenon of augmentation (Augmentation Severity Rating Scale [ASRS]) has been developed.25 In the six-month European study, the ASRS scores remained low throughout the trial, with small fluctuations.57 Retrospective reanalysis of IRLS and ASRS data by augmentation experts showed rates of clinically relevant augmentation of 1.5% (versus 0.5% in the placebo group) over six months in double-blind conditions63 and of 2.9% over 12 months in the open-label study.64 However, none of these patients discontinued the treatment because of augmentation.
Conclusion
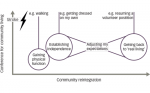
Like many chronic disorders, RLS varies considerably in terms of both symptom severity and degree of impact on health and wellbeing. In patients with mild RLS, good sleep hygiene should be recommended. Patients should be advised to avoid alcohol, caffeine or heavy meals before going to sleep. Bedtime hours should be regular and activity gradually reduced in the evening. Pharmacological treatment should be limited to those patients who suffer from clinically relevant RLS symptoms. Most patients with idiopathic RLS respond robustly to dopaminergic agents. The best strategy is to start pharmacological therapy cautiously and at the lowest recommended doses. Augmentation, mainly characterised by the occurrence of RLS symptoms earlier in the day, is a phenomenon that may be observed with dopamine agonists.
Recent papers agree in defining rotigotine as a well tolerated drug with good efficacy in idiopathic RLS, with control of both daytime and nocturnal symptoms even at long-term follow-up intervals. The dose used in published studies ranges between 0.5 and 4mg/24 hours; however, the European Medicines Agency (EMA)-approved dose ranges between 1 and 3mg/24 hours. The constant drug concentrations over 24 hours seem to be a favourable strategy to also cover daytime symptoms and to avoid augmentation. Application-site reactions may limit the suitability of rotigotine for some patients; otherwise, the tolerability and safety of the rotigotine patch is similar to or better than the oral nonergot dopamine agonists.
In the last few years, some surveys have shown that there is a significant association between certain health factors and RLS. In severe RLS, a significant relationship with health problems such as cardiovascular diseases and hypertension has been found.65–68 Sleep loss and the presence of PLMS might explain the increased cardiovascular risk in RLS patients, and this increased risk may also help to justify the pharmacological treatment of moderate/severe RLS cases. ■