Chronic inflammatory demyelinating polyneuropathy (CIDP) is an acquired progressive sensorimotor neuropathy of the peripheral nerves and nerve roots that appears to be immune-mediated by both the cellular and humoral immune systems. It is caused by chronic damage to the myelin sheaths of the neurons of the peripheral nervous system. It has a variable prognosis, with many patients experiencing a relapsing and remitting course, but does respond well to medical therapy.1 The contributing factors to the development of CIDP are highly debated, and no single mechanism has been defined. However, some reports indicate that a number of cases may have been a result of viral illness or vaccination.2,3 CIDP shares many common events and effects as Guillain–Barré syndrome (GBS), such as areflexia, slowed nerve conduction and increased cerebrospinal fluid (CSF) protein. Thus, the two are often linked in research.4 However, unlike GBS, CIDP has a longer onset of symptoms, with diagnostic criteria placing the onset of symptoms over at least an 8-week period.1 The relationship between GBS and vaccination was first proposed in 1976, when a mild increase in cases was observed up to 8 weeks following vaccination against swine flu.5,6 While the majority of cases of CIDP are not linked to vaccination, the possibility of vaccination as an antecedent event for some cases of CIDP has called into question the safety of giving vaccines to patients currently suffering from CIDP. The GBS/CIDP Foundation International currently recommends that patients diagnosed with either condition within 2 weeks of receiving a vaccine should not receive the same vaccine again.7 All other cases should be discussed with the patient’s neurologist before receiving vaccinations. In this study, we will review data regarding vaccination as an antecedent event to CIDP and data regarding the use of vaccines in patients with a current diagnosis of CIDP.
Methods
An extensive search of “CIDP,” “CIDP and vaccines” and “CIDP vaccines” was conducted using PubMed, Google Scholar, Up to Date and Medscape. Articles discussing vaccinations as an antecedent event of CIDP and articles discussing vaccination administration to patients with previously diagnosed CIDP are included in this study. Articles were limited to those published in English between 1 January 1995 to 1 April 2020. Articles under consideration were reviewed and divided into two categories: articles that addressed vaccination as an antecedent event to CIDP and articles that addressed the administration of vaccines to patients with existing CIDP. Articles were further divided by article type: case study, case series, database review and research study.
Results
Four articles were found discussing vaccination as an antecedent event to CIDP: two case studies, one case series, and one database review (Table 1). Of the two case studies, one reported a case following the influenza vaccine and the other following the AH1N1 influenza vaccination.2,8 The case series identified three cases following the influenza vaccine.9 The case following the AH1N1 vaccine, presented by Remiche et al., was unique in that the patient was found to have an underlying hereditary neuropathy.2 The fourth article was a review of the Italian CIDP database that reviewed data on the anteceding events of 411 patients, where 1.5% claimed vaccinations 1–42 days before the onset of CIDP.10
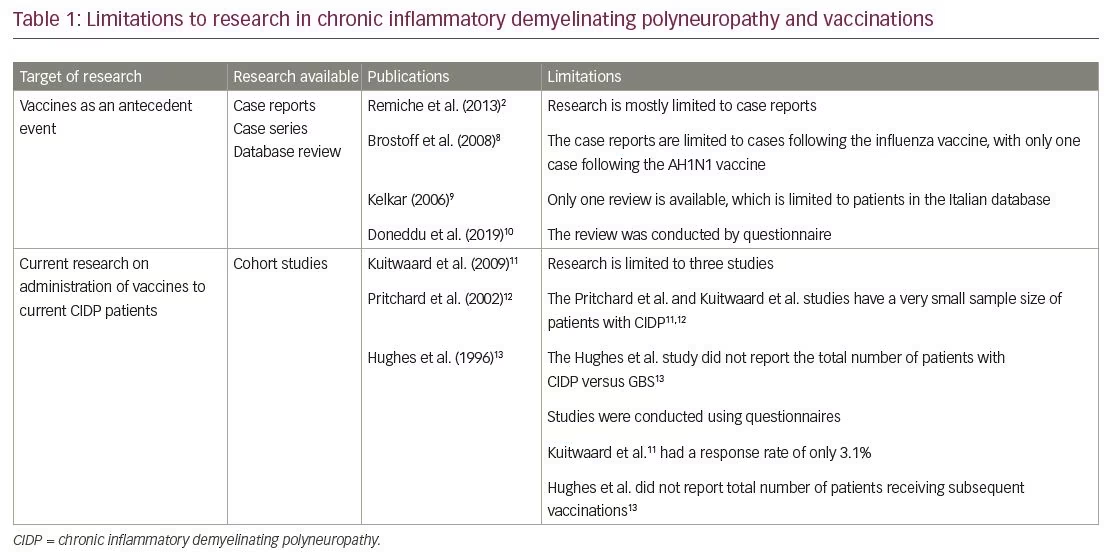
Three articles were discovered discussing the worsening of CIDP symptoms following subsequent vaccinations.11–13 All articles discussing the recurrence of CIDP following routine vaccines combined data from patients with GBS and those with CIDP (Table 1). The studies of Kuitwaard et al. and Pritchard et al. reported fewer patients with CIDP compared with patients with GBS, with one study including 76 patients with CIDP out of a total of 321 who completed the questionnaire, and the other only including 179 patients with CIDP out of a total of 1,114.11,12 Furthermore, both studies included a small sample size of patients who received a vaccine following their initial diagnosis, with 24 out of the 76 in the Kuitwaard et al. study and 65 of the 179 in the Pritchard et al. study. Both studies reported a higher proportion of patients with CIDP experiencing worsening of their symptoms following the administration of a vaccine relative to that of patients with GBS; 11% of the patients with CIDP reported worsening symptoms compared with only 2.6% of patients with GBS.11,12 However, the percentage of patients with worsening symptoms was different between the two studies. In the study by Kuitwaard et al., 5 out of 24 (20%) patients with CIDP experienced worsening symptoms after receiving a flu vaccine, compared to 5 out of 65 (8%) in the study performed by Pritchard et al.11,12 This is most likely a product of the small sample sizes of each study.
The third study, by Hughes et al., did not differentiate between patients with CIDP and GBS, reporting a total of 110 patients that had either CIDP or GBS.13 They reported two possible cases of relapse following subsequent vaccinations, one recurrence of GBS following several different immunizations and one report of relapse of peripheral neuropathy following tetanus immunizations. The total number of patients who received vaccinations following their initial diagnosis was not reported in the study.
Discussion
One of the difficulties of establishing antecedent events to CIDP is the chronic nature of the disease. The onset of CIDP, by clinical criteria, must take place over 8 weeks.1 This makes attributing a single event to the beginning of the disease difficult, as the actual date of disease onset is rarely straightforward. Overall, there is very little literature reviewing the association between vaccination and the onset of CIDP. Out of four available reports on the possible association, two were case studies, and one was a case series. The full database analysis showed that out of 411 patients who reported an event prior to diagnosis, only 1.5% had received vaccinations.10 Furthermore, the case report presented by Remiche et al. described a pre-existing neurological disease that may have influenced the development of CIDP following vaccination.2 Thus, of the available data, there are only 13 cases identifying vaccination as an antecedent event to CIDP, with one case that may be confounded by a pre-existing underlying illness.
The reports addressing the use of vaccines in patients with a prior CIDP diagnosis are also limited in number, and those available contradict each other at times. The percentage of patients with CIDP that develop worsening symptoms was far greater in the study by Kuitwaard et al. than in the study by Pritchard et al., with 20% versus 8% of CIDP patients experiencing worsening symptoms reported by Kuitwaard and Pritchard, respectively.11,12 Furthermore, the study by Hughes et al. reported only one patient with continuously relapsing peripheral neuropathy following vaccinations.13 This may be due, in part, to the overall small size of all three reviews and the larger sample size included in the study by Pritchard et al.12 Furthermore, only 89 patients with CIDP were represented between the studies by Pritchard et al. and Kuitwaard et al., contrasting with the much larger sample size of 417 patients with GBS. In both studies, the rate of worsening symptoms in CIDP was higher than the rate of GBS recurrence of 0% and 4%, respectively.11,12 This may be related to the larger sample size of patients with GBS present in both studies, as well as the relapsing, remitting nature of CIDP itself. Hughes et al. did not report the number of patients with CIDP versus those GBS included in their study.13
Conclusion
Given the limited amount of information regarding CIDP and vaccines, more research is required to determine further if there is genuinely a correlation between vaccination and CIDP. While the available data show a possible association, it is also limited in quantitative data and a definitive association cannot be determined. Furthermore, the chronic onset of CIDP makes determining antecedent and contributing events difficult. Also, the relapsing and remitting nature of the disease makes it difficult to assess whether worsening symptoms following revaccination can be attributed to the vaccine itself. Therefore, we feel that more information is needed in order to determine if vaccinations are safe to use in patients with CIDP, as the studies in our review showed cases of both the development of CIDP after vaccination and the worsening of CIDP symptoms following revaccination. Future studies should be conducted with larger sample sizes of CIDP patients to establish proper guidelines for this disease.