Duchenne muscular dystrophy (DMD) is an X-linked recessive, progressive and universally fatal disease in the spectrum of dystrophinopathies,1 with an incidence of 21.4 patients in 100,000 live male births worldwide.2,3 Historically, patients with DMD would lose ambulation by the age of 10 due to muscle weakness and die by the age of 20 from respiratory failure and cardiomyopathy. With the addition of corticosteroids as well as improved supportive care, the average ambulation of patients with DMD has been prolonged to their early teens, and their average life span has increased until their late 20s to early 30s.4
DMD is caused by a mutation in the dystrophin gene (DMD), which encodes the protein dystrophin. The dystrophin protein is vital to the integrity of the muscle membrane. It forms a link between the cytoskeleton and the muscle fibre plasma membrane (sarcolemma).2 The lack of dystrophin is mechanically disadvantageous and causes continuous leakage of intracellular content, resulting in inflammation and fibrosis.5 Corticosteroid therapy (prednisone and deflazacort) was initially trialled to decrease the observed inflammation and appears to slow the progression of weakness in DMD.6
Current treatment options
The standard of care for DMD includes the use of classic, or chronic, corticosteroid therapy to improve motor and pulmonary function, reduce the need for scoliosis surgery, and delay the loss of ambulation and onset of cardiomyopathy.1,7 When using classic corticosteroids, patients with DMD often experience changes in physical appearance, increased risk of cataracts, mood disturbances and endocrine pathologies such as osteoporosis/bone fragility, growth failure, obesity, delayed puberty, glucose intolerance/diabetes and secondary adrenal insufficiency.8,9 Becoming non-ambulatory compounds increases the risk of steroid-induced osteoporosis/bone fragility and obesity.10 Alternate dosing regimens, such as high-dose weekend steroids or 10 days on/off dosing, have been developed with the goal of minimizing the side effects of DMD treatment while maintaining the benefit.8
Deflazacort was developed as a more targeted anti-inflammatory glucocorticoid receptor agonist with reduced mineralocorticoid receptor activity. However, deflazacort still carries strong glucocorticoid receptor transactivation, with significant concerns regarding an increase in cataracts, cushingoid features and growth stunting compared with prednisone.11
Other therapies have recently been approved by the US Food and Drug Administration (FDA) for certain mutations in the DMD gene. Exon-skipping therapy uses antisense oligonucleotides to convert genetically susceptible out-of-frame mutations to in-frame mutations, producing some functional dystrophin.12 Currently, four exon-skipping therapies are available for the fraction of DMD mutations that are amenable.12 The first microdystrophin gene replacement therapy, delandistrogene moxeparvovec, was approved by the FDA in June 2023 for boys with DMD between 4 and <6 years of age.13 This therapy is contraindicated in individuals with antibodies against the adeno-associated virus vector and those with deletions of any portion of exons 8 and/or 9 due to an increased risk of immunologic reaction. Several other gene replacement products are under active study.14 Gene replacement therapy protocols are not currently “curative” as they still do not produce full-length dystrophin proteins and do not reach every muscle cell in the body, among other reasons. They are also not suitable for all patients with DMD due to age restrictions, viral vector antibody status, and/or contraindicated mutations.
Vamorolone
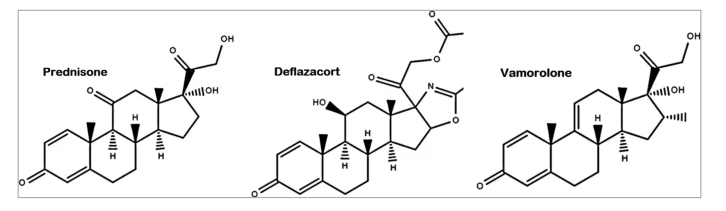
Vamorolone is a newly developed dissociative steroid. It differs from classic corticosteroids in that it contains a delta 9,11 double bond between C9 and C11 carbons instead of a carbonyl (=O) or hydroxyl (-OH) group on the C11 carbon (Figure 1).15 This change allows vamorolone to bind to the same target receptors with fewer side effects than classic corticosteroids.
Figure 1: The chemical structure of vamorolone versus prednisone
Classic corticosteroids affect the body in multiple ways.6 First, they activate the glucocorticoid receptor, which translocates to the nucleus and binds to the glucocorticoid response element. The downstream effects of glucocorticoid response element binding include transrepression and transactivation. Transrepression is the act by which the glucocorticoid response element inhibits the proinflammatory transcription factors nuclear factor κB (NF-κB) and activator protein 1 (AP-1), thereby acting as an anti-inflammatory agent. This process is also the mode in which classic corticosteroids induce immunosuppression.6 Transactivation promotes metabolic cascades via cyclic adenosine monophosphate (cAMP) and protein kinase A (PKA), resulting in the increase in glucose production via gluconeogenesis and the degradation of hepatic glycogen; lipolysis, which produces free fatty acids and glycerol; and proteolysis, which releases amino acids. Second, the chronic use of classic corticosteroids leads to insulin resistance, obesity and diabetes. Third, by a similar transactivation mechanism, classic corticosteroids lead to bone resorption and osteoporosis. Fourth, classic corticosteroids also stabilize (to a mild degree) the sarcolemmal membrane after injury in DMD.6 Lastly, corticosteroids are also agonists of mineralocorticoid receptors, resulting in sodium and water retention, leading to hypertension, all of which can negatively impact an already weakened heart.7
Vamorolone binds as a partial agonist to the glucocorticoid receptor and a potent antagonist to the mineralocorticoid receptor (hence the term “dissociative”).16 It maintains the positive subactivities of the glucocorticoid receptor, including transrepression of proinflammatory factors and improved membrane stabilization while “dissociating” the negative subactivities, such as the transactivation of the metabolic cascade, bone turnover and mineralocorticoid effects.17 Furthermore, vamorolone has been shown to act as an antagonist to mineralocorticoid receptors.17 Other mineralocorticoid receptor antagonists, such as eplerenone or spironolactone, have been used to treat dystrophic cardiomyopathy for years.18 Vamorolone’s mineralocorticoid antagonism has similar efficacy to eplerenone, making it a potentially dual-acting drug for patients with DMD.16 A table comparing vamorolone’s subactivities to those of prednisone and deflazacort is presented in Table 1.
Table 1: Subactivities of vamorolone, prednisone, and deflazacort
|
| Anti-inflammatory (NF-kB inhibition)/Transrepression | Glucocorticoid Response Element (GRE)/ Transactivation | Mineralocorticoid receptor | Linear growth | Bone turnover | Weight gain | Mood changes | Cataracts |
| Vamorolone | Agonist | None | Antagonist | Normal | Normal | Increased | Mild increase | Unknown |
| Prednisone | Agonist | Agonist | Agonist | Stunted | Increased | Increased | Increased | Increased |
| Deflazacort | Agonist | Agonist | Weak agonist | Stunted | Increased | Increased | Mild increase | Increased |
NF-kB = Nuclear factor kappa B.
Vamorolone has been investigated in human clinical trials for the treatment of DMD since 2015, and an New Drug Application has been submitted to the FDA this year.19 The phase I trial investigating vamorolone for the treatment of DMD was conducted in 2015 with 86 adults receiving either a single dose or 14 doses of vamorolone and showed this drug to be safe.17
The phase IIa trial investigating the safety of vamorolone for the treatment of DMD in 48 boys aged 4 to <7 years was initiated by the Cooperative International Neuromuscular Research Group in 2016. This 4-week study (2 active weeks and 2 washout weeks), in which patients were given a dose of either 0.25, 0.75, 2.0 or 6.0 mg/kg/day, showed no safety concerns in relation to vamorolone.20 A 24-week extension trial then showed that patients receiving the higher doses of vamorolone (2.0 or 6.0 mg/kg/day) demonstrated improvements in muscle function and biomarker data, suggesting reduced side effects with similar benefits in patients receiving the higher doses of vamorolone compared with those receiving classic corticosteroids.21 A longer-term extension trial of 18 and subsequently 30 months at vamorolone doses of 2.0 and 6.0 mg/kg/day met the primary endpoint measure, change in time-to-stand velocity from baseline to 30 months, and was comparable to historical prednisone data.22 Additionally, vamorolone showed an improved linear growth trajectory compared with prednisone.
A double-blind, randomized IIb clinical trial was then conducted in 2018 to compare vamorolone 2 mg/kg/day, vamorolone 6 mg/kg/day, prednisone 0.75 mg/kg and placebo. Vamorolone and prednisone demonstrated improvements in many of the motor endpoints, such as time to stand velocity, 6-minute walk test and time to run/walk 10 m velocity, studied (time to stand velocity, 6-minute walk test and time to run/walk 10 m velocity) compared with placebo. Vamorolone showed normal linear growth (height) compared with prednisone, which stunts linear growth, and bone turnover serum markers were improved in patients treated with vamorolone compared with those treated with prednisone.23 A post-hoc, cross-study analysis presented at the World Muscle Society in 2022 showed that vamorolone demonstrated an improved height and body mass index profile of vamorolone compared to prednisone and deflazacort.24
Vamorolone was shown to have some negative side effects, including cushingoid features, stomach upset and weight gain.22 The incidence of cataracts and its impact on cardiomyopathy in DMD has not been clinically established for vamorolone.
While vamorolone has only been trialled in DMD, it is possible that its improved safety profile may be relevant to other diseases that are currently treated with classic corticosteroids as first-line therapies. Some preclinical studies have already been conducted to investigate the vamorolone in other contexts.25–27
In conclusion, vamorolone is a promising anti-inflammatory agent with equivalent benefits, less stunting of linear growth and less bone turnover than has been observed with daily classic corticosteroids.