Despite significant advances in tumor imaging, neurosurgery, and radiotherapy, the prognosis for patients with malignant gliomas is extremely poor. The five-year survival rate for patients with glioblastoma (GBM), the most aggressive form of malignant glioma, is less than 5% after initial diagnosis.1 Factors that contribute to the dismal prognosis associated with GBM include its infiltrative nature throughout the brain, which limits the effectiveness of local treatment of surgical resection and targeting of radiotherapy, and the blood–brain barrier (BBB), which limits access of systemically administered therapeutics to the tumor.
In the past decade a number of drug delivery strategies have been developed to overcome challenges presented by the BBB. In particular, direct drug administration into the brain parenchyma, such as convection-enhanced delivery (CED), has shown promising results in both animal models and clinical trials.2–12 CED is a continuous infusion that uses a convective (versus diffusive) flow to drive the therapeutic agent throughout a larger region of tissue. This technique is well suited for the delivery of liposomes6,9,11–15 and particulate drug carriers,6,9,16,17 which have the potential to provide a sustained level of drug and to reach cellular targets with improved specificity. However, CED requires the use of potentially risky surgical procedures to position the catheter into the patient’s brain parenchyma.18,19 The convective flow to distribute the drug through the implanted catheter leads to measurable and significant inflammation and local edema because the drug solution infuses continuously beyond the tumor boundary into the adjacent normal brain tissue.4,7,9 This ‘spillover’ of drug to unwanted brain regions may be due to the pressure gradient of the convective bulk flow of CED and could lead to neural toxicity.20
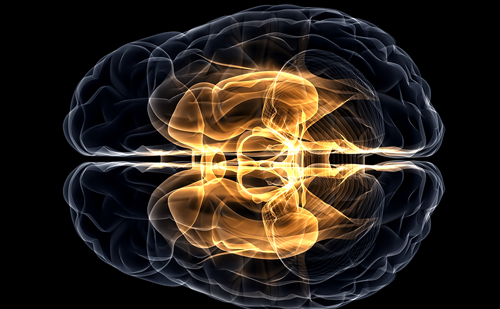
One technique that holds promise for bypassing the BBB to deliver drugs to the brain and eliminating the surgical risk and the spillover effect of drug to normal tissue is intranasal delivery. Intranasal delivery provides a practical, noninvasive method for delivering therapeutic agents to the brain because of the unique anatomic connections provided by the olfactory and trigeminal nerves. These nerves connect the nasal mucosa and central nervous system (CNS), allowing them to detect odors and other chemical stimuli.21,22 Intranasally administered drugs reach the brain parenchyma, spinal cord, and cerebrospinal fluid (CSF) within minutes by using an extracellular route through perineural and/or perivascular channels along the olfactory and trigeminal nerves without binding to any receptor or using axonal transport (see Figure 1).23,24 In addition to bypassing the BBB, advantages of intranasal delivery include rapid delivery to the CNS, avoidance of hepatic first-pass drug metabolism, and elimination of the need for systemic delivery, thereby reducing unwanted systemic side effects. Intranasal delivery also provides painless and convenient self-administration for patients, features that encourage its use for delivering therapeutic agents into the CNS.25 Many therapeutic agents, including growth factors, proteins, peptides, viral vectors, liposomes, and vaccines, have been delivered to the CNS through the nasal route and applied for the treatment of CNS disorders in both animals and humans.21,24,26–39 Thorne et al. reported that insulin-like growth factor-1 can be rapidly transported into the rat brain and upper spinal cord via the olfactory and trigeminal pathways.21 Thorne et al. have recently reported delivery of interferon-beta- 1b to the CNS in monkeys along the same neural pathways.29 In humans, intranasal delivery of insulin has been shown to improve memory in normal adults40 and in patients with early Alzheimer’s disease41,42 without changing blood levels of glucose or insulin.43 Also, intranasal oxytocin has been reported to improve trust in humans.44
In brain tumors, anticancer agents such as methotrexate,45 5-fluorouracil,46 and raltitrexed47 have been delivered successfully to the brain using intranasal delivery. Shingaki et al. reported that intranasally delivered methotrexate reaches the CSF and reduces tumor weight in rodent glioma allografts.48 Intranasal drug targeting to the brain of the chemotherapeutic raltitrexed is significantly higher than that with intravenous administration.47 However, these chemotherapeutic agents do not discriminate between tumor and normal tissue. Thus, the concentrations of drug required to kill tumor cells can also lead to toxicity in normal neural tissue. To achieve therapeutic efficacy without toxicity to normal tissue, the drugs need to preferentially target brain tumor while sparing normal tissue from damage.
Recently, two different therapeutic agents, including a glioma-adapted vesicular stomatitis virus strain, VSVrp30a,49 and an oligonucleotide telomerase inhibitor, GRN163,50 have been used to selectively target malignant gliomas and have shown impressive oncolytic activity without harming normal brain tissue. Both studies utilized intranasal delivery, resulting in targeted and effective delivery of the therapeutic agents to the tumor and inhibition of the tumor growth in human GBM xenografts. In addition, intranasal delivery of the telomerase inhibitor GRN163 doubled the survival time for xenografted animals without apparent toxicity. Although intranasal GRN163 delivery is extracellular, as described above, intranasal VSVrp30a likely involves viral transmission within the olfactory neural pathway to the brain. These findings support further development of intranasal VSVrp30a and GRN163 as potential therapies for brain tumor patients and perhaps as a means for treating multifocal brain tumors such as metastasis brain tumors and/or pediatric brainstem tumors, which are less amenable to potentially risky surgical procedures. Telomerase inhibitors, including GRN163, have reached the stage of clinical trials, so may soon become part of the available therapeutic armamentarium for cancer.
Given the promising results from recent animal studies, intranasal therapeutic agents would seem to be prime candidates for clinical trials in patients with brain tumors. Initial trials of intranasal perillyl alcohol have begun in patients with recurrent malignant gliomas, and a reduction in the size of the brain tumors has been reported.51,52 ■
Intranasal Delivery—A New Therapeutic Approach for Brain Tumors
Article
References
- CBTRUS Central Brain Tumor Registry of The United States. Available at: www,cbtrus,org/2007-2008/tables/report/2007/table22.pdf (accessed September 18, 2008).
- Huynh GH, Deen DF, Szoka Jr FC, Barriers to carrier mediated drug and gene delivery to brain tumors, J Control Release, 2006;110:236–59.
- Ozawa T, Santos RA, LambornK R, et al., In vivo evaluation of the boronated porphyrin TABP-1 in U-87 MG intracerebral human glioblastoma xenografts, Mol Pharm, 2004;1:368–74.
- Ozawa T, Gryaznov SM, HuL J, et al., Antitumor effects of specific telomerase inhibitor GRN163 in human glioblastoma xenografts, Neuro-oncol, 2004;6:218–26.
- Ozawa T,Afzal J, Lamborn KR, et al., Toxicitybiodistributionand convection-enhanced delivery of the boronated porphyrin BOPP in the 9L intracerebral rat glioma model, Int J Radiat Oncol Biol Phys, 2005;63:247–52.
- MacKay JA, Deen DF, Szoka Jr FC, Distribution in brain of liposomes after convection enhanced delivery: modulation by particle chargeparticle diameterand presence of steric coating, Brain Res, 2005;1035:139–53.
- KawakamiK M, Kioi, Husain SR, Puri RK, Distribution kinetics of targeted cytotoxin in glioma by bolus or convection-enhanced delivery in a murine model, J Neurosurg, 2004;101:1004–11.
- Lidar Z, Mardr Y, Jonas T, et al., Convection-enhanced delivery of paclitaxel for the treatment of recurrent malignant glioma:a phase I/II clinical study, J Neurosurg, 2004;100:472–9.
- Mamot C, Nguyen JB, Pourdehnad M, et al., Extensive distribution of liposomes in rodent brains and brain tumors following convectionenhanced delivery, J Neurooncol, 2004;68:1–9.
- Boiardi A, Eoli M, Salmaggi A, et al., Local drug delivery in recurrent malignant gliomas, Neurol Sci, 2005;26(Suppl. 1):S37–39.
- Saito R ,Krauze MT, Noble C, et al., Tissue affinity of the infusate affects the distribution volume during convection-enhanced delivery into rodent brains:Implications for local drug delivery, J Neurosci Methods, 2006.
- Saito R, Bringas JR, McKnight TR, et al., Distribution of liposomes into brain and rat brain tumor models by convection-enhanced delivery monitored with magnetic resonance imaging, Cancer Res, 2004;64:2572–9.
- Noble CO, Krauze MT, Drummond DC, et al., Novel nanoliposomal CPT-11 infused by convection-enhanced delivery in intracranial tumors:pharmacology and efficacy, Cancer Res, 2006;66:2801–6.
- Saito R, Krauze MT, Noble CO, et al., Convection-enhanced delivery of Ls-TPT enables an effectivecontinuouslow-dose chemotherapy against malignant glioma xenograft model, Neuro Oncol, 2006;8:205–14.
- Krauze MT, Noble CO, Kawaguchi T, et al., Convection-enhanced delivery of nanoliposomal CPT-11 (irinotecan) and PEGylated liposomal doxorubicin (Doxil) in rodent intracranial brain tumor xenografts, Neuro Oncol, 2007;9:393–403.
- Valtonen S, Timonen U, Toivanen P, et al., Interstitial chemotherapy with carmustine-loaded polymers for high-grade gliomas:a randomized double-blind study, Neurosurgery, 1997;41:44–8, discussion 48–9.
- Voges J, Reszka R, Gossmann A, et al., Imaging-guided convectionenhanced delivery and gene therapy of glioblastoma, Ann Neurol, 2003;54:479–87.
- Bobo RH, Laske DW, Akbasak A, et al., Convection-enhanced delivery of macromolecules in the brain, Proc Natl Acad Sci U S A, 1994;91:2076–80.
- Groothuis DR, The blood-brain and blood-tumor barriers: a review of strategies for increasing drug delivery, Neuro-oncol, 2000;2:45–59.
- Sandberg DI, Edgar MA, Souweidane MM, Convection-enhanced delivery into the rat brainstem, J Neurosurg, 2002;96:885–91.
- Thorne RG, Pronk GJ, Padmanabhan V, Frey WH, 2nd delivery of insulin-like growth factor-I to the rat brain and spinal cord along olfactory and trigeminal pathways following intranasal administration, Neuroscience, 2004;127:481–96.
- Dhanda D, Frey II WH, Leopold D, Kompella UB, Approaches for drug deposition in the human olfactory epithelium, Drug Delivery, 2006;5:64–72.
- Thorne RG, Emory CR, Ala TA, Frey II WH, Quantitative analysis of the olfactory pathway for drug delivery to the brain, Brain Res, 1995;692:278–82.
- Thorne RG, Frey II WH, Delivery of neurotrophic factors to the central nervous system:pharmacokinetic considerations, Clin Pharmacokinet, 2001;40:907–46.
- Romeo VD, deMeireles J, Sileno AP, et al., Effects of physicochemical properties and other factors on systemic nasal drug delivery, Adv Drug Deliv Rev,1998;29:89–116.
- Hanson LR, Frey II WH, Strategies for intranasal delivery of therapeutics for the prevention and treatment of neuroAIDS, J Neuroimmune Pharmacol, 2007;2:81–862.
- Liu XF, Fawcett JR, Hanson LR, Frey II WH, The window of opportunity for treatment of focal cerebral ischemic damage with noninvasive intranasal insulin-like growth factor-I in rats, J Stroke Cerebrovasc, 2004;Dis13:16-23.
- Zhao HM, Liu XF, Mao XW, Chen CF, Intranasal delivery of nerve growth factor to protect the central nervous system against acute cerebral infarction, Chin Med Sci, 2004;J19:257–61.
- Thorne RG, Hanson LR, Ross TM, et al., Delivery of interferon-beta to the monkey nervous system following intranasal administration, Neuroscience, 2008;152:785–97.
- Yamada M, Chiba T, Sasabe J, et al., Nasal colivelin treatment ameliorates memory impairment related to Alzheimer’s disease, Neuropsychopharmacology, 2008;33:2020–32.
- De Rosa R, Garcia AA, Braschi C, et al., Intranasal administration of nerve growth factor (NGF) rescues recognition memory deficits in AD11 anti-NGF transgenic mice, Proc Natl Acad Sci U S A, 2005;102:3811–16.
- Zhang J,Wu X, Qin C, et al., A novel recombinant adeno-associated virus vaccine reduces behavioral impairment and beta-amyloid plaques in a mouse model of Alzheimer’s disease, Neurobiol Dis, 2003;14:365–79.
- Lundstrom K, Alphavirus vectors for gene therapy applications, Curr Gene Ther, 2001;1:19–29.
- Tafaghodi M, Jaafari MR, Sajadi Tabassi SA, Nasal immunization studies using liposomes loaded with tetanus toxoid and CpG-ODN, Eur J Pharm Biopharm, 2006;64:138–145.
- AlsarraI A, Hamed AY, Alanazi FK, Acyclovir liposomes for intranasal systemic delivery: development and pharmacokinetics evaluation, Drug Deliv, 2008;15:313–21.
- Sharma S, Mukkur TK, Benson HA, Chen Y, Pharmaceutical aspects of intranasal delivery of vaccines using particulate systems, J Pharm Sci, 2008.
- Peek LJ, Middaugh CR, Berkland C, Nanotechnology in vaccine delivery, Adv Drug Deliv Rev, 2008;60:915–28.
- Gozes I, Giladi E, Pinhasov A, et al., Activity-dependent neurotrophic factor:intranasal administration of femtomolar-acting peptides improve performance in a water maze, J Pharmacol Exp Ther, 2000;293:1091–8.
- Banks WA, During MJ, Niehoff ML, Brain uptake of the glucagon-like peptide-1 antagonist exendin(9-39) after intranasal administration, J Pharmacol Exp Ther, 2004;309:469–75.
- Benedict C, Hallschmid M, Hatke A, et al., Intranasal insulin improves memory in humans, Psychoneuroendocrinology, 2004;29:1326–34.
- Reger MA,Watson GS, Frey II WH, et al., Effects of intranasal insulin on cognition in memory-impaired older adults: modulation by APOE genotype, Neurobiol Aging, 2006;27:451–8.
- Reger MA,Watson GS, Green PS, et al., Intranasal insulin improves cognition and modulates beta-amyloid in early AD, Neurology, 2008;70:440–48.
- Born J, Lange T, Kern W, et al., Sniffing neuropeptides: a transnasal approach to the human brain, Nat Neurosci, 2002;5:514–16.
- Kosfeld M, Heinrichs M, Zak PJ, et al., Oxytocin increases trust in humans, Nature, 2005;435:673–6.
- Wang F, Jiang X, Lu W, Profiles of methotrexate in blood and CSF following intranasal and intravenous administration to rats, Int J Pharm, 20032;63:1–7.
- Sakane T, Yamashita S, Yata N, Sezaki H, Transnasal delivery of 5- fluorouracil to the brain in the rat, J Drug Target, 1999;7:233–40.
- Wang D, Gao Y, Yun L, Study on brain targeting of raltitrexed following intranasal administration in rats, Cancer Chemother Pharmacol, 2005;1–8.
- Shingaki T, Sakane T, Yamashita S, et al., Transnasal delivery of anticancer drugs to the brain tumor:a new strategy for brain tumor chemotherapy, Drug Delivery System,1999;14:365–71.
- Ozduman K,Wollmann G, Piepmeier JM, et al., Systemic vesicular stomatitis virus selectively destroys multifocal glioma and metastatic carcinoma in brain, J Neurosci, 2008;28:1882–93.
- Hashizume R, Ozawa T, Gryaznov SM, et al., New therapeutic approach for brain tumors:Intranasal delivery of telomerase inhibitor GRN163, Neuro Oncol, 2008;10:112–20.
- da Fonseca CO, Landeiro JA, Clark SS, et al., Recent advances in the molecular genetics of malignant gliomas disclose targets for antitumor agent perillyl alcohol, Surg Neurol, 2006;65(Suppl. 1): S1:2–1:8, discussion S1:8–1:9.
- da Fonseca CO, Schwartsmann G, Fischer JN et al., Preliminary results from a phase I/II study of perillyl alcohol intranasal administration in adults with recurrent malignant gliomas, Surg Neurol, 2008;70:259–66, discussion 266–57.
Further Resources
Trending Topic
Brain metastases (BM) are the most frequent among intracranial brain tumours and their incidence is rising as therapeutic advances are improving the survival of patients with advanced cancer. The incidence of BM has been calculated as 9–17% based on various studies, although the true incidence is thought to be higher.1 Patients with BM have a […]
Related Content in Neurological Oncology

Glioblastoma Multiforme Glioblastoma multiforme (GBM) is the most malignant of the primary brain cancers with only about 12 % of patients surviving beyond 36 months (longterm survivors).1–4 Most GBMs are heterogeneous in cellular composition consisting of tumor stem cells, malignantly transformed mesenchymal cells, ...
AbstractThe management of aggressive pituitary tumours remains a challenge, however, the recent identification of temozolomide as a chemotherapeutic agent with significant efficacy against these tumours has heralded a new therapeutic era. There has been an exponential growth in the international ...

Most pituitary tumours are non-invasive, benign adenomas that remain confined to the sella turcica. Although there is, at present, no accepted definition of aggressive pituitary adenomas, one would suggest that these have a tendency to recur after initial surgery. They ...

The goal of glioma surgery is to maximize tumor resection while preventing a new post-operative neurologic deficit. For both low- and high-grade gliomas, increased extent of resection correlates with improved progression-free survival as well as with overall survival.1–5 While some ...

Gliomas are primitive cerebral tumours representing a heterogeneous group of intra-axial central nervous system neoplasms of glial origin with different histology, behaviour, molecular characteristics, natural history and thus prognosis.1–4 Four distinct tumour grades have been identified according to the degree ...
High-grade glioma (HGG) is the most common type of primary brain tumour in adults and accounts for >75% of the estimated 22,070 newly diagnosed malignant primary brain tumours in the US each year.1 More than half of HGGs are glioblastoma (GBM), the ...

New contrast-enhancing lesions discovered on routine follow-up brain imaging at or near the site of previously treated primary or metastatic brain tumours represent a challenge for radiologists and oncologists, as radiation-induced injuries may have an appearance that is virtually indistinguishable ...

Paraneoplastic neurological syndromes (PNS) were first described in the 20th century. A summary of observations dating back to 1982 was published in the seminal book by Henson and Urich.1 The detection of autoantibodies for myasthenia gravis (MG) and later for Lambert-Eaton ...

High-grade glioma (HGG) is the most common type of primary brain tumour in adults and accounts for >75% of the estimated 22,070 newly diagnosed malignant primary brain tumours in the US each year.1 More than half of HGGs are glioblastoma (GBM), the ...

In spite of their lack of propensity for hematogenous dissemination, the prognosis for adults afflicted with gliomas has not substantially improved, even with advances in neurosurgery, neuro-oncology, and radiation oncology.1,2 Although microsurgical resection remains the initial treatment of choice for ...

Although benign in nature, pituitary tumors continue to offer many opportunities for improvement in therapy. Goals of treatment include complete removal or ablation of tumor cells, maintenance of normal pituitary function, normalization of elevated hormone levels in endocrine-active tumors, and ...

The North American Brain Tumor Consortium (NABTC) is one of three multi-institutional consortia initially funded by the National Cancer Institute (NCI) in 1994 with the primary purpose of efficiently evaluating novel treatments in adults with central nervous system (CNS) tumors. Its ...
Latest articles videos and clinical updates - straight to your inbox
Log into your Touch Account
Earn and track your CME credits on the go, save articles for later, and follow the latest congress coverage.
Register now for FREE Access
Register for free to hear about the latest expert-led education, peer-reviewed articles, conference highlights, and innovative CME activities.
Sign up with an Email
Or use a Social Account.
This Functionality is for
Members Only
Explore the latest in medical education and stay current in your field. Create a free account to track your learning.

