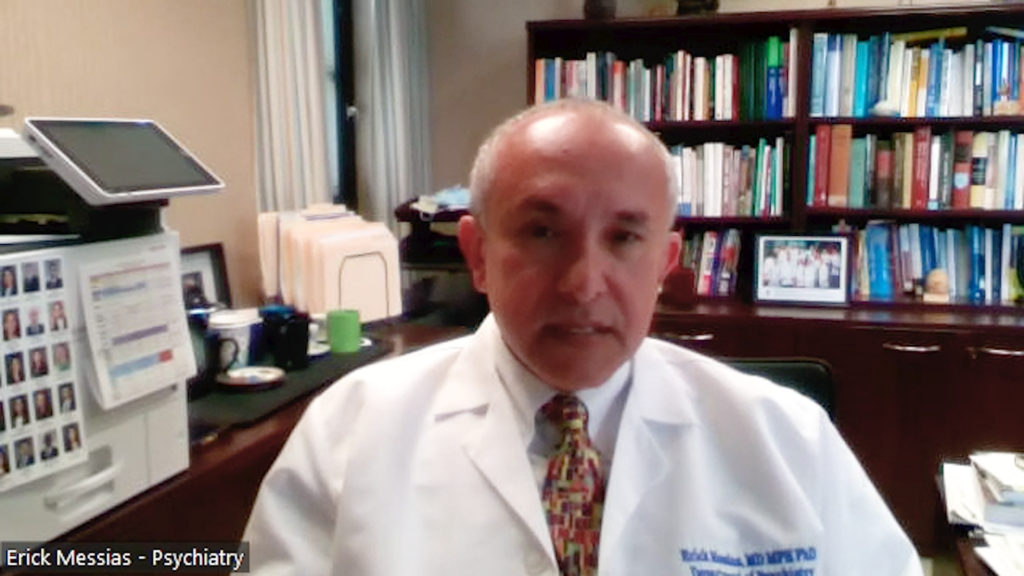
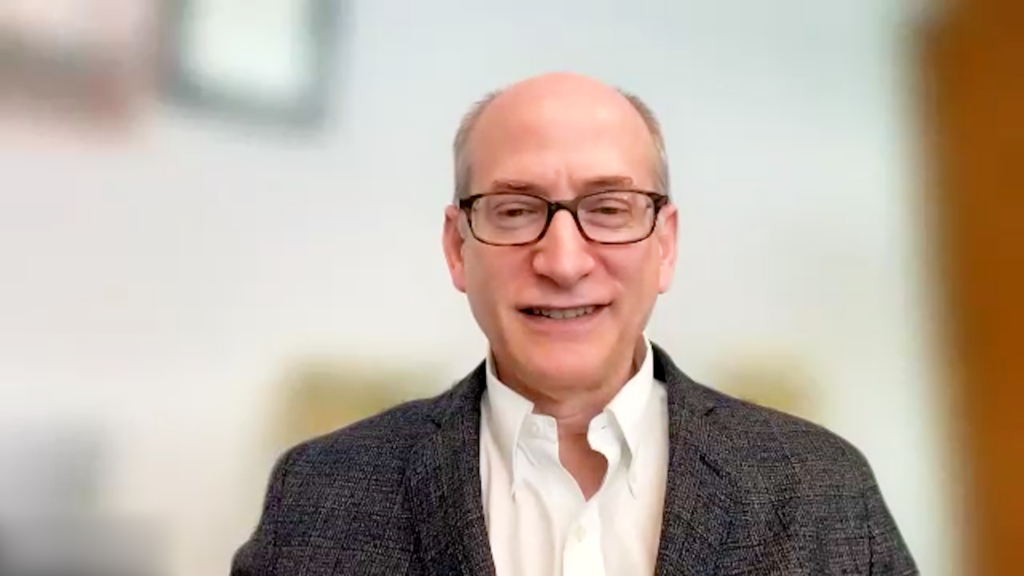
The discovery of the rapid antidepressant effects of ketamine shifted the biology and treatment of psychiatric disorders, emphasizing targeting glutamate signaling, rather than monoamine signaling, for schizophrenia and depression. Research highlights synaptic deficits, network disinhibition, and synaptic loss in schizophrenia, while identifying glutamate synaptic dysfunction and the efficacy of ketamine for depression. In this touchNEUROLOGY interview, we speak with Prof. John Krystal (Yale University, New Haven, CT, USA) to discuss the core findings from studies on ketamine’s effects in patients with schizophrenia; targeting deficits in glutamate signaling to treat psychosis and reduce secondary increases in striatal dopamine release in the context of schizophrenia and also explores the evolution of understanding depression highlighting glutamate synaptic dysfunction and the recognition of ketamine as an effective treatment for treatment-resistant symptoms.
The abstract entitled ‘New Biology and New Treatments for Schizophrenia and Mood Disorders: My 30-Year Journey With Ketamine Research‘: Nasrallah Award Lecture, was presented at the American Psychiatric Association, 20-24 May 2023, San Francisco, CA, USA.
Questions:
- What core findings emerged from studies on ketamine’s effects in patients with schizophrenia? (0:11)
- In the context of schizophrenia, how are deficits in glutamate signaling being targeted to treat psychosis and reduce secondary increases in striatal dopamine release? (4:01)
- How has the understanding of depression evolved with the identification of glutamate synaptic dysfunction and the recognition of ketamine as an effective treatment for treatment-resistant symptoms? (5:03)
- What novel strategies are used for enhancing ketamine’s effectiveness in depression treatment? (8:25)
- What questions remain unanswered, and what is on the horizon in the development of ketamine for schizophrenia and mood disorders? (11:07)
Disclosures: see below
Support: Interview and filming supported by Touch Medical Media. Interview conducted by Katey Gabrysch.
Filmed as a highlight of APA 2023
Access more content on psychiatric disorders here
Transcript
What core findings emerged from studies on ketamine’s effects in patients with schizophrenia?
Around 1990, my colleagues and I started studying the effects of ketamine and healthy subjects as a way of understanding glutamate synaptic dysfunction in schizophrenia. What’s come out of that work? Out of our work? Out of basic scientists following up on on our work? Out of were conducted by many of our colleagues are a few simple ideas.
First, glutamate synaptic dysfunction, unhealthy people can recapitulate many of the signs and symptoms and cognitive impairments that you see in schizophrenia. Second, the idea that that there are two types of circuit dysfunction that are mimicked by giving an NMDA receptor antagonist. One of these kinds of circuit dysfunctions involve deficits and glutamate signaling. A second kind of network dysfunction is that ketamine can produce a loss of inhibitory tuning of networks. They become noisy, they become error prone, mental representations can become less precise learning can be compromised as a result. So both of these dysfunctions occur simultaneously when you produce when you give ketamine to people, and they are both present in people with schizophrenia, particularly early in the course of schizophrenia.
Where this is taking us in medications, again, is in two separate directions. First, there’s an interest in medications that can compensate for the glutamate signaling deficits associated with the synaptic dysfunction in schizophrenia.
These are drugs that can facilitate NMDA receptor function such as the glycine transporter one inhibitors. Or perhaps drugs that could stimulate other glutamate receptors such as the ampa glutamate receptor or certain metabotropic glutamate receptors. It also draws our attention to drugs that can restore inhibitory tuning. Some examples of these drugs are MGLR2 agonists, which showed some promise but haven’t yet panned out as treatments for schizophrenia.
But it turns out that two new emerging antipsychotic mechanisms also restore inhibitory tuning. One of these mechanisms is TAR one agonism. And another one, and that’s an example of that is the Synovian drug. Eulaterant, and two other drugs target a different mechanism which restores inhibitory tuning. Particularly in cortical inputs into the stratum. One of those mechanisms is m four positive allosteric modulation or m four muscarinic agonism in combination with a peripheral muscarinic receptor blocker. The drugs that have those properties are being developed by Sarival Pharmaceuticals and Karuna Pharmaceuticals. So this is a really exciting time. We’re going from the neurobiology to treatment and really coming up with new treatments that may alleviate the symptoms of schizophrenia without blocking the dopamine d two receptor.
In the context of schizophrenia, how are deficits in glutamate signaling being targeted to treat psychosis and reduce secondary increases in striatal dopamine release?
Basically, we have we have two general approaches. One is to compensate for glutamate synaptic deficits by facilitating glutamate signaling using drugs that directly or indirectly enhance glutamate signaling like a glycine transporter one blocker.
The alternative is to provide is to use a drug that restores inhibitory signaling. And examples of those drugs are MGLR2 agonists, which unfortunately didn’t work that well.
But two new treatment mechanisms, muscarinic m four agonism and tarr one agonism. And there are examples of those drugs which seem to treat psychosis without blocking dopamine d two receptors.
How has the understanding of depression evolved with the identification of glutamate synaptic dysfunction and the recognition of ketamine as an effective treatment for treatment-resistant symptoms?
Our testing of ketamine grew out of a shift in our thinking about the neurobiology of depression. For much of the last 30 years or so, people have focused on monoamines as the primary mechanism of pathology and depression. Presumably deficits in serotonin signaling or deficits in norepinephrine signaling that might be related to pathology in those nerve cells in the brain. As my colleagues and I were shifting, our focus to the cortex and limbic system we began to focus our thinking upon the traditional intrinsic signaling mechanisms of the cortex and limbic system. Predominantly glutamate as the main excitatory mechanism and gaba as the main inhibitory mechanism. Subsequent work in depression from many groups, including my colleagues here at Yale, have suggested that there are at least two, you might say, fundamental or archetypal kinds of synaptic dysfunction for glutamate in depression. One, reduced efficacy of glutamate synaptic signaling to reduced numbers of glutamate synapses in the brain.
A third type of dysfunction involves loss of glutamate homeostasis arising from pathology in the supporting gleal cells of the brain. With those three kinds of problems, we can understand why some of the effects of ketamine might be therapeutic. Two things that ketamine does in animals, in stressed animals, are to restore synaptic efficacy and to regrow synapses. We find evidence for that for both of those properties of ketamine and human. So, for example, Carlos Zarate’s group and projects led by Allison Nugent found that ketamine treatment can restore normal synaptic function as measured by the magnitude of sensory evoked potentials.
We, my colleagues, here at Yale, in a project led by Irina Esterlis and Sophie Holmes found that ketamine could regrow synapses in patients who had synaptic deficits. So many of what we found in the animal models is now being shown in early studies in depressed patients.
In other words, what we see is that ketamine can mobilize the brain’s own resilience mechanisms in a much more rapid and effective way than traditional anti depressive treatment and thereby seem to treat symptoms more rapidly and more effectively particularly for those patients who haven’t responded to traditional antidepressants.
What novel strategies are used for enhancing ketamine’s effectiveness in depression treatment?
What we and others are thinking these days is that the initial rapid effect of anti depressant that you begin to see within a few hours may take place before the synapses are regrown, but that the maintenance of the antidepressant effects depends on the persistence of the regrown synapses. So with that in mind, we’re very interested in strategies that protect the newly regrown synapses from being eliminated, and a variety of strategies are emerging. The simplest, you might say, or the most basic, is to combine ketamine with psychotherapies. There is evidence of both digital therapy and in person cognitive behavioural therapy, which probably exercises the circuits of the brain, and in so doing causes local neurotrophic effects that protect regrown synapses. You might call that an example of activity dependent plasticity.
Another strategy which is very new and is suggested by a study that we publish just a few years ago now, is to combine ketamine with a drug that protects the newly regrown synapses from being eliminated. In order to understand how this combination works, you need to understand that one of the ways that synapses are eliminated in the brain is when the immune cells of the brain called microglia become activated, and in a pro inflammatory way and engulf and eliminate synapses. In order to deal with that, we have combined an immunosuppressive drug called rapamycin, which inactivates the pro the pro inflammatory micro glial actions, we’ve combined that drug rapamycin with ketamine. So we believe that that combination, which appears to extend the duration of ketamine efficacy, acts by taking advantage of the fact that ketamine regrows the synapses, and rapamycin protects them from being degraded.
What questions remain unanswered, and what is on the horizon in the development of ketamine for schizophrenia and mood disorders?
We think that with ketamine as with the emerging research on psychedelics, and and potentially MDMA for post traumatic stress disorder. As well as with the new antipsychotic medications that I had mentioned earlier that we’re in an era where advances in neuroscience are producing many new treatment options. At least many treatment options that should be available in the years to come. That being said, all of this work is one step forward. There are still going to be many new kinds of treatments needed. In particular, we would like to be able to better develop treatments that can be personalized, where we understand the personal biology of a person with depression or PTSD or schizophrenia or bipolar disorder, and use that knowledge of their personal biology to guide the specific treatment that they’re given.
We would prefer to be treating patients in the world where we knew right off the bat, who needed ketamine, as opposed to waiting for them to fail multiple antidepressants in order to become eligible for treatment.
We would prefer to be able to know who was not going to respond to a drug like ketamine. So we could spare them the potential cost and risk of a a treatment like that. So we in some ways, we are farther ahead than we’ve ever been in the science of the psychopharmacology of psychiatry. In other ways, it feels like we’re just at the beginning of an era where scientific knowledge of the biology of the disorder and the needs of individual patients gets people more rapidly to more effective and better tolerated treatments.
Subtitles and transcript are autogenerated
Disclosures:
John Krystal is a consultant for: Aptinyx, Inc. Biogen, Idec, MA Bionomics, Limited (Australia) Boehringer Ingelheim International Cerevel Therapeutics, LLC Clearmind Medicine, Inc. Cybin IRL (Ireland Limited Company) Enveric Biosciences Epiodyne, Inc. EpiVario, Inc. Evidera, Inc. Janssen Research & Development Jazz Pharmaceuticals, Inc. Leal Therapeutics, Inc. Otsuka America Pharmaceutical, Inc. Perception Neuroscience, Inc. Praxis Precision Medicines, Inc. Spring Care, Inc. Sunovion Pharmaceuticals, Inc. Tetricus, Inc; receives grant/research support from: AstraZeneca Pharmaceuticals provides the drug, Saracatinib, for research related to NIAAA grant “Center for Translational Neuroscience of Alcoholism [CTNA-4] Novartis provides the drug, Mavoglurant, for research related to NIAAA grant “Center for Translational Neuroscience of Alcoholism [CTNA-5] Cerevel provides the drug PF-06412562 for A Translational and Neurocomputational Evaluation of a D1R Partial Agonist for Schizophrenia (5 U01 MH121766-03); on the advisory board for: AE Research Foundation Advisory Board Biogen, Idec, MA Biohaven Pharmaceuticals BioXcel Therapeutics, Inc. (Clinical Advisory Board) Cerevel Therapeutics, LLC Delix Therapeutics, Inc. Eisai, Inc. EpiVario, Inc. Freedom Biosciences, Inc. Jazz Pharmaceuticals, Inc. Neumora Therapeutics, Inc. Neurocrine Biosciences, Inc. Novartis Pharmaceuticals Corporation Perception Neuroscience, Inc. Praxis Precision Medicines, Inc. PsychoGenics, Inc. Takeda Industries Tempero Bio, Inc. Terran Biosciences, Inc. Tetricus, Inc.; and major stock shareholder in: Stock Biohaven Pharmaceuticals Spring Care, Inc. Stock Options Biohaven Pharmaceuticals Medical Sciences Clearmind Medicine, Inc. EpiVario, Inc. Neumora Therapeutics, Inc. Tempero Bio, Inc. Terran Biosciences, Inc. Tetricus, Inc.