![]() Multiple sclerosis (MS) is a chronic neurological condition that often presents with vague or intermittent symptoms, making early recognition particularly challenging in primary care. As diagnostic delays can significantly impact long-term outcomes, timely identification and referral are critical.
Multiple sclerosis (MS) is a chronic neurological condition that often presents with vague or intermittent symptoms, making early recognition particularly challenging in primary care. As diagnostic delays can significantly impact long-term outcomes, timely identification and referral are critical.

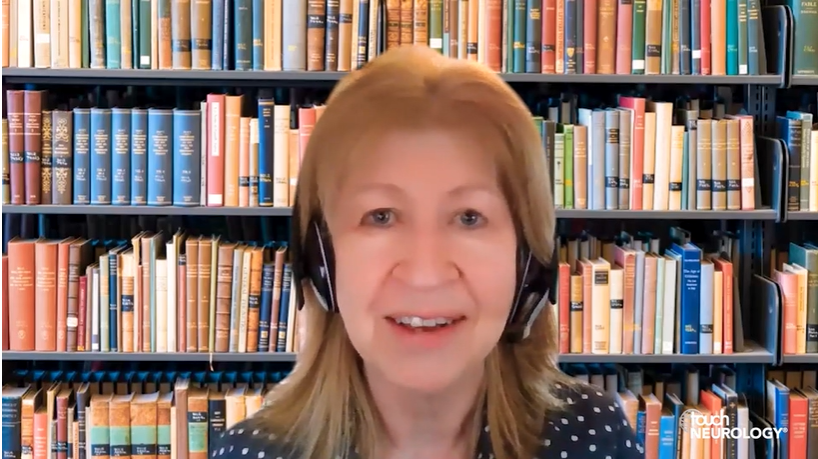
In alignment with the mission of the National Multiple Sclerosis Society (NMSS) and in recognition of #WorldMSDay, we talk with Dr Lisa Doggett (UT Health Austin, TX, USA), member of the South Central Board of the NMSS, and a physician who has personally navigated the diagnostic journey of MS, offering a unique dual perspective as both a primary care provider (PCP) and a person living with the condition. Drawing on clinical insight and lived experience, the discussion highlights early presentation, strategies to improve collaboration between primary care and neurology, and the importance of patient-centred communication throughout the diagnostic process.
1. From your experience, what are the most common signs PCPs might miss or misattribute when it comes to early signs and symptoms of MS? How can neurologists support PCPs in recognizing those early red flags to lead to more accurate referrals?
MS can be difficult to recognize. PCPs may miss early MS signs like subtle sensory changes (numbness, tingling), atypical vision problems, unexplained fatigue or weakness, and bowel or bladder issues, as these can mimic other conditions. The relapsing-remitting course experienced by most patients with MS can also make the diagnosis tricky—when symptoms improve, they may be forgotten and ignored. Neurologists can support primary care providers by establishing clear referral pathways, promoting MS education and guideline awareness (such as the McDonald criteria), and communicating directly after seeing referred patients, whether by sharing clinic notes or phoning the provider to discuss a difficult or ambiguous case. Timely access to MRI scans is also essential. Ultimately, close collaboration between neurology and primary care improves early detection and leads to more appropriate referrals.
2. Once a referral from primary care is made, how can neurologists ensure the patient feels seen, heard and not dismissed—especially when symptoms are vague or intermittent?
Neurologists can ensure patients feel heard by:
- Active listening: Prioritizing the patient’s subjective experience and allowing time and space for them to describe symptoms without interruption.
- Validating concerns: Acknowledging how even subtle symptoms can impact a patient’s life, rather than dismissing them.
- Thorough examination: Conducting a comprehensive neurological exam, looking for even small abnormalities (my initial exam was normal except for barely detectable nystagmus).
- Clear communication: Explaining the diagnostic process, differential diagnoses and the rationale for further testing helps foster transparency and trust.
- Empathy and reassurance: Expressing empathy for the patient’s uncertainty and providing reassurance that their concerns are being taken seriously, regardless of the final diagnosis.
3. As someone who has experienced the diagnostic process first-hand, you’ve seen how delays can affect health outcomes. What are some ways neurologists can reduce those delays—especially for patients whose symptoms don’t “fit the mould”?
Diagnostic delays are common in MS, and they can contribute to disease progression. To reduce diagnostic delays, especially when a patient has atypical symptoms, neurologists should:
- Expedite urgent referrals that raise concern for MS.
- Emphasize detailed history-taking, prompting patients about seemingly unrelated past events, such as “pinched nerves” or unusual visual symptoms.
- Broaden diagnostic thinking.
- Prioritize early MRI imaging.
- Apply the McDonald criteria appropriately while excluding other conditions.
- Use biomarkers, such as CSF analysis.
- Seek consultation from an MS specialist when a case remains uncertain.
4. What systems or habits do you think foster the best collaboration between neurology and primary care once a diagnosis is confirmed?
To ensure optimal care post-MS diagnosis, neurologists should encourage patients to maintain regular check-ins with their PCPs. Too often, comorbidities are missed or inadequately managed because MS eclipses everything else. Some patients only see their neurologist and miss critical screening tests and vaccines that would be recommended and typically managed by their PCP. For patients with complex needs —due to disability, non-medical factors or co-morbidities—closer collaboration may be required. This could include phone calls or even joint visits, where feasible. At the very least, neurologists should ensure that electronic health records and treatment plans are shared with the PCP.
5. Which type of healthcare providers (PT, pharmacist, mental health professional, etc) made a positive impact on your diagnostic journey?
I was fortunate to get diagnosed just eight days after my most significant symptoms started. My main symptom was vague dizziness, followed by taste and visual changes. I think that if I hadn’t been a physician, my complaints might have been dismissed. I had a major advantage because I knew who to call and had direct access to a neurologist, family physician, and ear, nose and throat (ENT) doctor who provided advice during the week after my symptoms started.
The ENT doctor fit me in for an urgent appointment and took me seriously. Despite a pretty unremarkable exam he ordered the MRI, and then a neuroradiologist talked me through the findings and made the diagnosis.
Since that time, I have worked with a balance physical therapist, an optometrist, acupuncturist, and several yoga instructors—with varying results. Despite my initial skepticism, a mindfulness-based stress reduction (MBSR) class and subsequent daily meditation practice significantly reduced my most notable symptoms and improved my ability to cope with the uncertainty of MS.
6. What are three takeaways that you want neurologists to understand about the diagnostic journey of MS (from your perspective both as a PCP and a person living with MS)?
- Listen to patients – Get a detailed history and take their concerns seriously. To diagnose MS, in particular, if the presentation is atypical (as it often is), look for a historic pattern of unusual neurologic symptoms. Go ahead and get that MRI if MS is a real possibility.
- Stay curious – When a diagnosis is unclear, keep looking for answers. Consult with colleagues for help, and don’t give up or be too quick to label someone with a diagnosis that could be wrong.
- Early treatment is essential – High-efficacy therapies, especially when initiated early, can dramatically improve outcomes in MS. Once the diagnosis is made, rapid initiation of a disease-modifying therapy should be a top priority.
About Dr Lisa Doggett
Dr Lisa Doggett is a family and lifestyle medicine physician and writer based in Austin, TX, USA. Diagnosed with multiple sclerosis (MS) in 2009, she provides lifestyle coaching and preventive care consultations for people with MS at the Multiple Sclerosis and Neuroimmunology Center, UT Health Austin, the clinical practice of Dell Medical School at The University of Texas at Austin. Her award-winning memoir, Up the Down Escalator: Medicine, Motherhood, and Multiple Sclerosis, chronicles her journey from physician to patient while directing a clinic for people without insurance.
Editor: Katey Gabrysch, Editorial Director.
Disclosures: No funding was received in the publication of this article.
Cite: Recognizing multiple sclerosis early: An interview with Lisa Doggett. touchNEUROLOGY. 15 May 2025
Learn more about the National MS Society here.
Register now to receive the touchNEUROLOGY newsletter!
Don’t miss out on hearing about our latest peer reviewed articles, expert opinions, conference news, podcasts and more.