“Continued support for research, and for the patients themselves, is absolutely critical. I’m grateful for the opportunity to help bring some of this work to light.”
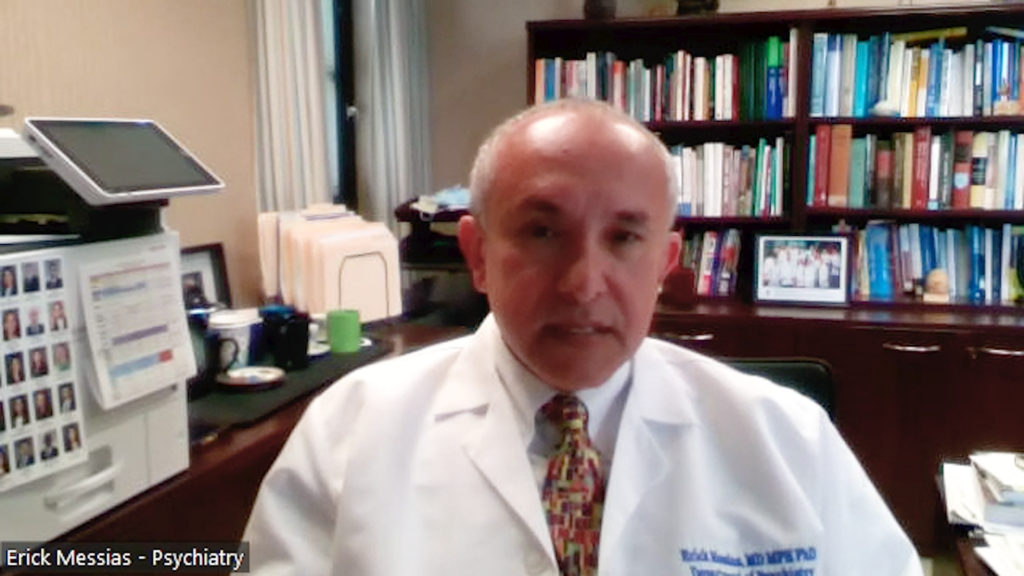
Dr Anissa Abi-Dargham is Chair of Psychiatry and Behavioral Health at the Renaissance School of Medicine at Stony Brook University and a pioneering researcher in molecular brain imaging and schizophrenia. With a career spanning over three decades, including pivotal roles at Columbia University, Yale, and the National Institute of Mental Health, her work has shaped our understanding of dopamine’s role in psychosis and the potential for more targeted, personalized treatments. Following her receipt of the 2025 APA Award for Research in Psychiatry,1 we spoke with Dr Abi-Dargham about her ground-breaking research, the future of psychiatric therapeutics, and what this recognition means for collaborative science.
Photo credit: Stony Brook Medicine/Jeanne Neville
1. Could you tell us a little about your background?
I’m Dr Anissa Abi-Dargham, I’m a medical doctor and currently Chair of Psychiatry and Behavioural Health at Stony Brook University. My career has been largely focused on research, particularly in the area of schizophrenia. I’ve been a full-time researcher for the last couple of decades. Before coming to Stony Brook University, New York, in 2016, I spent 20 years at Columbia University, and before that, I was at Yale University for 6 years. Prior to that, I worked at the National Institute of Mental Health (NIMH) in Washington, D.C., where I completed my first research fellowship in schizophrenia. My second fellowship was at Yale, focusing on molecular brain imaging.
I went to medical school in Beirut, Lebanon, where I was born, and moved to the US in 1985 to complete my psychiatry residency in Memphis, Tennessee. So, it’s been Lebanon, Memphis, D.C., Yale, Columbia, and now Stony Brook!
2. Congratulations on receiving the 2025 APA Award for Research in Psychiatry. What does this award mean to you, and how does it reflect the collaborative nature of your work?
Thank you. It really is an honour to receive this award, particularly because the APA is the primary organization representing clinicians and practising psychiatrists in the United States. I’ve received other recognitions before, like the Lieber Award for outstanding research in schizophrenia and election to the National Academy of Medicine but receiving this from a group so closely tied to clinical practice felt particularly special.
“Our work is very much multimodal and it’s not something one person can do alone, it’s the result of sustained collaboration.”
I didn’t even know I’d been nominated, so it was a lovely surprise. It also felt special to have the chance to present to a broad audience, and I felt that I was able to convey the excitement and relevance of our research and data, which spans many years and requires teamwork across disciplines.
Our work is very much multimodal and it’s not something one person can do alone, it’s the result of sustained collaboration. So, while I received the award, it felt like recognition of efforts across my entire team.
3. What were the key ideas you presented at the APA, and how has your work shaped our understanding of schizophrenia?
My research journey began in the early ’90s, when I became fascinated with psychosis and the dopamine system. All antipsychotic drugs at the time targeted dopamine, there was a lot of interest in understanding if there are abnormalities in dopaminergic transmission in brains of patients with schizophrenia, particularly the D2 receptor.
I had been interested in schizophrenia because I was interested in understanding how people become psychotic. That was a concept that fascinated me when I was in high school. So, as my research career began, I looked at dopamine, mostly because the dose of antipsychotics is related to their affinity at one of the dopaminergic receptors (the D2) which meant that D2 targeting was the driving mechanism to treat psychosis. In addition, dopamine is a critical neurotransmitter that plays roles in cognition, especially prefrontal cortical mediated cognition, decision-making, reward processing, and movement. These systems are often impaired in people with schizophrenia. Movement is also impaired in diseases like Parkinson’s, as this is related to loss of dopamine. Similarly, cognitive deficits, psychosis (a disturbance in perception), and anhedonia or reward dysfunction, or the inability to experience pleasure, are all dopamine-related functions, and they’re all affected in schizophrenia.
Using positron emission tomography (PET) imaging, we developed and validated methods to visualize dopamine transmission in the brain and found different alterations in different brain regions. Excess dopamine in the striatum, which is associated with psychosis, and too little in cortical regions like the prefrontal cortex, which affects cognition and motivation.
This imbalance led us to ask what’s regulating dopamine? That took us into studying other systems like the cholinergic and kappa opioid receptor systems. My APA talk traced this body of work, years of multimodal imaging and collaborative studies that map molecular abnormalities to cognitive and clinical outcomes.
4. How might your research and understanding influence future therapeutic approaches?

The goal of this work is twofold, identifying therapeutic targets and discovering biomarkers. The more we understand about the functional effects of molecular abnormalities, the more precise we can be in developing treatments.
One promising area in biomarker development is neuromelanin-sensitive MRI, which uses MRI to detect dopamine metabolism indirectly. It’s much less invasive than PET and could serve as a biomarker of dopamine vulnerability across different conditions such as psychosis, substance use, and more.
We have also been exploring D1 partial agonists, drugs that mimic dopamine at D1 receptors, which are important for cognition. We recently completed a multisite study using this approach, and we’re analysing the data now.2
Another area is brain circuitry. Dopamine influences entire circuits, connecting the prefrontal cortex to striatum, thalamus, and back to the cortex again. We had a striking case where deep brain stimulation of the substantia nigra resolved resistant auditory hallucinations. This suggests that circuit-level interventions, whether invasive or non-invasive like transcranial magnetic stimulation (TMS), could be promising.
We are also seeing pharmaceutical interest in kappa opioid receptor antagonists and muscarinic agonists. Our work has shown that the kappa system may drive anhedonia in schizophrenia, making it a compelling target. Similarly, the cholinergic system’s interaction with dopamine is crucial, and it’s exciting to see the muscarinic M1/M4 agonist drug developed by Karuna Therapeutics receive FDA approval. But that’s just the beginning, multimodal imaging could help refine which interventions may work well for which patients.
5. What current innovations in psychiatry excite you the most?
One standout development is the approval of a new drug for schizophrenia, the first non D2 drug in 50 years. It’s generated enormous interest and has sparked a wave of research into muscarinic receptor modulators. That’s a very active area right now and incredibly encouraging for the field.
6. Is there anything else you’d like to add?
Just a heartfelt thank you for highlighting research in mental health. Disorders like schizophrenia are devastating and often emerge early in life, becoming chronic illnesses. Continued support for research, and for the patients themselves, is absolutely critical. I’m grateful for the opportunity to help bring some of this work to light.
About Dr Anissa Abi-Dargham
Anissa Abi-Dargham, MD, is Chair of Psychiatry and Behavioral Health, Lourie Endowed Chair in Psychiatry, SUNY Distinguished Professor, and Associate Dean for Clinical and Translational Science at Stony Brook University’s Renaissance School of Medicine.
Dr Abi-Dargham is an expert in the areas of molecular imaging, pharmacology, schizophrenia and addiction. She is an internationally recognized leader in the use of molecular imaging of the human brain to study schizophrenia and its comorbidity with addiction. In recognition for her work, she received the Leiber Prize for outstanding research in schizophrenia from the Brain and Behavior Research Foundation, she was elected to the National Academy of Medicine in 2016 and served as President of the American College for Neuropsychopharmacology (ACNP) in 2017. She is a Special Lecturer at Columbia University in New York, where she spent the last twenty-two years of her career prior to her move to Stony Brook University in 2016. She directs the Multi Modal Translational Imaging Lab at Stony Brook and oversees a multidisciplinary team with expertise in multiple neuroimaging modalities used in tandem to address important questions about the brain mechanisms of schizophrenia.
Editor: Katey Gabrysch, Editorial Director.
Disclosures: No funding was received in the publication of this article. Dr Anissa Abi-Dargham is a consultant for Sunovion, has received grant/research support from National Institutes of Health, is on advisory boards for AbbVie, Herophilus, Maplight, Neurocine, Suniovion, Terran Life Sciences, and has received honoraria/honorarium from AbbVie, ACNP, and Bristol Meyers.
Cite: Understanding of dopamine’s role in psychosis: An interview with Dr Anissa Abi-Dargham, APA 2025 award winner. touchNEUROLOGY. 17 June 2025.
References:
- Abi‑Dargham A. Misfiring Signals: Dopamine Dysfunction in Schizophrenia-From Neural Pathways to Behavioral Manifestations: Award for Research in Psychiatry. American Psychiatric Association Annual Meeting. Los Angeles. 2025 May 19.
- Fonteneau C, Tamayo Z, Price A, Pan L, Afriyie-Agyemang Y, Agrawal S, et al. Rationale and study design of a brain-based clinical trial [preprint]. medRxiv. 2025. Available from: https://doi.org/10.1101/2025.04.18.25326082v1
Register now to receive the touchNEUROLOGY newsletter!
Don’t miss out on hearing about our latest peer reviewed articles, expert opinions, conference news, podcasts and more.