Dystonia is a neurological syndrome characterised by involuntary, sustained, patterned and repetitive contractions of opposing muscles, leading to twisting and repetitive movements or abnormal postures of the body part involved.1–4 Dystonic movements must be distinguished from other hyperkinetic involuntary movements such as chorea, myoclonus, tremor or tics. Dystonias can be classified according several factors: age at onset, body distribution and aetiology. Dystonias in which symptoms typically begin after 26 years of age are classified as adult-onset dystonias, whereas dystonias beginning earlier are generally called young-onset dystonias.4,5 Focal dystonias involve a single body area, segmental dystonias affect contiguous body parts and generalised dystonias involve at least one leg, the trunk and another body part.1–5 Multifocal dystonias (two or more non-contiguous body parts) and hemidystonias (one side of the body) are less frequent body distributions.6 As for aetiology, primary dystonias are those in which dystonia (± tremor) is the only sign and symptom and no secondary cause or neurodegeneration is found. Conversely, secondary dystonias include a structural or a metabolic cause.1,2,7 In turn, the primary dystonias can be either sporadic or inherited.1,2,7
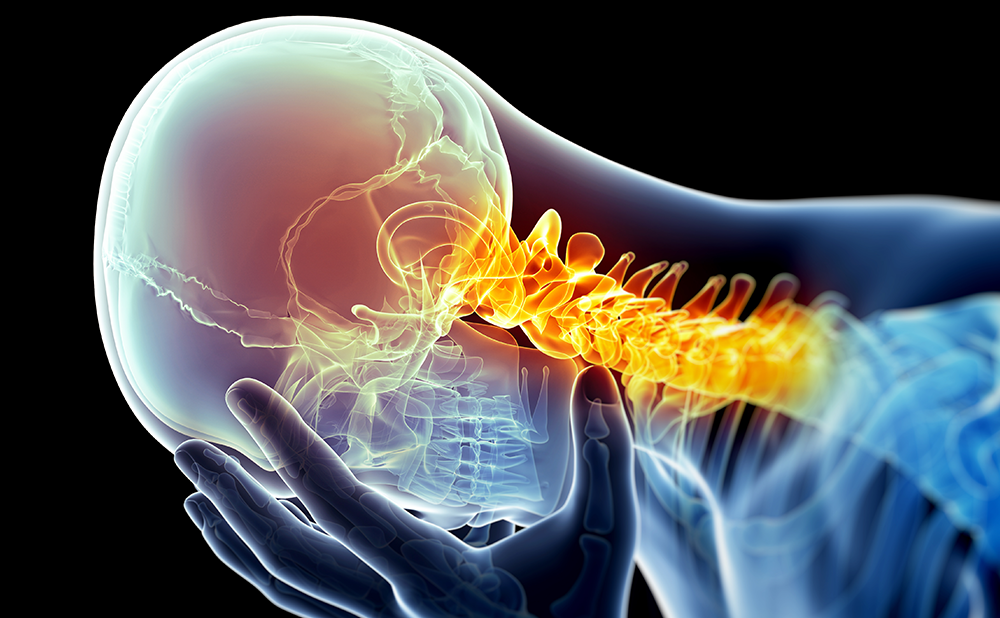
Cervical dystonia (CD), or spasmodic torticollis, affects the muscles of the neck and often the shoulders. It is the most common form of adult-onset focal dystonia, with an estimated prevalence of 5.7/100,000 in Europe.6 CD usually presents in the fifth decade of life, although it can affect individuals at any age.6 Although CD is classically described as being slightly more prevalent in females, both genders seem to be equally affected according to a European epidemiological study.8 Clinically, the predominant direction of the muscle twisting allows the identification of four core patterns of CD: rotation or torticollis (horizontal turning of the head), which is the most common; laterocollis (lateral flexion or tilt of the head); retrocollis (posterior extension of the head); and anterocollis (forward flexion of the head).9 In a series of 300 CD patients, Jankovic et al. identified torticollis in 82%, laterocollis in 42%, retrocollis in 29% and anterocollis in 25%.9 In a limited number of cases, the head may be shifted forward (forward shift) or off the midline (lateral shift). Nevertheless, Jankovic et al. found that the majority of patients (66%) had a combination of these patterns (complex CD).9 Head tremor (dystonic tremor) was found in 62% of patients, whereas hand tremor was present in 23%.3
Stress or fatigue may exacerbate CD, while factors such as relaxation, sleep and sensory manoeuvres usually improve it.10–12 The use of a sensory trick, or geste antagoniste, to temporarily alleviate the dystonia is used by up to 90% of patients.10–12 In a series of 50 patients, sensory tricks were found to induce a greater than 30% reduction in dystonia in 82%.13 Touching the chin, face or the back of the head are classic examples of sensory tricks in CD. In contrast to the temporary relief induced by sensory tricks, a long-lasting and spontaneous remission of CD is less frequent, with reported rates ranging between 10 and 20%.14,15 In fact, in 20–32% of patients CD may progress to segmental or generalised dystonia.14,15
Most cases of CD are idiopathic. Nevertheless, the finding of a family history of dystonia (12% of cases)3 or of any movement disorder (44% of cases)16 suggests a genetic susceptibility. Secondary causes of CD include tardive and acute dystonia due to dopamine receptor blocking agents, neck trauma (central and peripheral trauma are less frequent), metabolic disorders such as Wilson’s disease and pantothenate-kinase- associated neurodegeneration or Parkinson’s disease.
Pain and Quality of Life in Cervical Dystonia
Pain
The presence of pain in CD is frequent and constitutes a distinctive feature not usually present in other focal dystonias. Patients tend to report a diffuse pain over the neck and shoulders that usually irradiates to the side of head deviation.17
In one study of 266 patients with idiopathic CD, pain occurred in 75% of the patients and had a significant impact on disability,3 while it was reported by 68% in another series of 300 patients.9 Pain was associated with more prolonged and/or severe head turning along with the presence of transient spasms of the head.3
The mechanism of pain in CD remains mostly unknown. A small study has suggested a decreased threshold of pain perception in CD patients,18 which could point to the involvement of central processes in addition to local muscle involvement.17,19 Other potential causes of pain in CD are orthopaedic complications including cervical spine degeneration, spondylosis, disc herniation, vertebral subluxations and fractures, radiculopathies and myelopathies.19–22 The association of these orthopaedic lesions with pain is not clear, despite their prevalence in CD ranging between 18 and 41% and patients with CD having an increased risk of secondary lesions of the upper cervical spine.19,20 Studies have also failed to find a correlation between the presence or severity of pain and the presence or degree of spinal changes.17,19 Nevertheless, the presence of spinal lesions was identified as a predictor of less improvement in pain and dystonia after selective peripheral denervation surgery.19 One study did not find a conclusive association between the presence of pain and muscle tenderness; the results were significant when tenderness was assessed by muscle palpation, but not when measured by pressure algometry.17 In cases of CD treated with botulinum toxin, pain was also associated with decreased muscle strength of the neck.23
Quality of Life
Dystonias have a negative impact on quality of life (QoL).24–28 A study on focal, segmental and generalised dystonias found that the QoL of dystonic patients was worse in all domains, but mainly in those related to physical and social functioning, compared with the norms for the general UK population.28 Poor QoL is observed even when using different assessment tools, comprising both generic and disease-specific instruments.24–28 The results regarding gender effect on QoL differ, but they suggest either no difference between males and females28,29 or a worse QoL for females.24,30
CD has a negative impact on QoL compared with age- and gender-matched healthy control subjects.24,25–29,31 Several studies have tried to identify the most affected domains and the major determinants of QoL in patients with CD.24,25,27–34 Many studies have reported a major impact of CD on pain25,28,29,32 and in domains of role limitation (physical and emotional), mental health and social and physical functioning,24,25,28,32 as measured by the Medical Outcomes Study Short-Form 36 (SF-36), a generic QoL measure (see Table 1). Depression and anxiety are consistently reported as the main determinants of QoL in people with CD, in addition to pain27–29,30,32,33 (see Table 2). Additional variables reported as contributing to poor QoL were older age, low education level, unemployment, being separated/divorced and severity of dystonia; on the other hand, longer duration of disease, physical activity and treatment satisfaction were associated with a better QoL.24,25,27–30,34 Two studies have also identified self-perceived disfigurement and self-esteem as contributors to QoL, although with weaker effect estimates in multivariable analysis.28,30
The QoL of CD patients is comparable to that seen in patients with multiple sclerosis or Parkinson’s disease, or long-term survivors of stroke;24 however, it is better than the QoL reported by patients with generalised forms of dystonia.28,31 Compared with other focal dystonias, such as blepharospasm or limb dystonia, CD patients score poorer in the domain of pain, but perform similarly otherwise.25,29
How to Evaluate Pain and Quality of Life in Cervical Dystonia
Several scales have been used to evaluate CD, incorporating both objective and subjective measures (see Table 3). The most widely used is the Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS),35 along with the Burke-Fahn-Marsden Dystonia Scale36 and the Tsui Scale.37 The TWSTRS (range 0–87 points) consists of three subscales – severity (range 0–35), disability (range 0–23) and pain (range 0–20)35 – while the Burke-Fahn-Marsden Dystonia Scale36 consists of two subscores (movement and disability) and the Tsui Scale37 is composed of four subscores (movement, duration, shoulder elevation and tremor). Only the TWSTRS covers pain, and none assesses QoL, although both the TWSTRS and the Burke-Fahn- Marsden Dystonia Scale evaluate disability.35,36 Recently, two new disease-specific rating scales have been developed and validated: The Craniocervical Dystonia Questionnaire (CDQ-24)26 and The Cervical Dystonia Impact Profile (CDIP-58).38 The CDQ-24 was designed as a QoL instrument and includes five domains with a total of 24 items: stigma, emotional wellbeing, pain, activities of daily living and social/family life.26 The CDIP-58 is a patient-based scale of the health impact of CD, consisting of eight subscales (head and neck symptoms, pain and discomfort, upper limb activities, walking, sleep, annoyance, mood and psychosocial functioning).38
Pain in people with CD has mostly been evaluated using self-assessment analogue scales and the TWSTRS pain subscale.39–41 By contrast, QoL in CD has been evaluated by global health-related QoL instruments, such as the SF-36 and the EuroQol (EQ-5D) questionnaires, which provide overall assessment of QoL.24,25,27–29,31,32,42,43 The SF-36 is a self-report questionnaire consisting of eight domains: four physical (role limitations physical, bodily pain, physical functioning and general health perception) and four emotional (role limitations emotional, vitality, social functioning and mental health). Higher scores indicate a better QoL, ranging from 0 to 100.43 The EQ-5D is also a self-report questionnaire, composed of two parts: first, patients rate their health status within five dimensions (mobility, self-care, usual activities, pain and discomfort and anxiety and depression); and second, patients rate their health status using a visual analogue scale (VAS), with high scores corresponding to the best possible health.42
Pain and Quality of Life in the Treatment of Cervical Dystonia
Currently, CD is an incurable disease. Available symptomatic interventions should aim not only at the relief of dystonia and the associated symptoms, but also to decrease functional disability and improve QoL. Ideally, the prevention of long-term complications should also be one of the therapeutic goals.44
Therapeutic interventions for CD are broadly divided into botulinum toxin (BoNT), oral drugs, surgical interventions and physical therapy.1
Botulinum Toxin
BoNT is well-established as an effective and safe treatment for CD, as supported by seven class I studies.45 Available data suggest a superior efficacy and better tolerability compared with trihexyphenidyl, an anticholinergic oral drug.45,46 Currently, there are two serotypes of BoNT (BoNT type A [BoNTA] and BoNT type B [BoNTB]), and four brands are now approved for the treatment of CD: three BoNTA preparations – Botox® (Allergan, US), Dysport® (Ipsen, UK) and Xeomin® (Merz, Germany) – and one BoNTB preparation – Myobloc®/ Neurobloc® (Solstice Neurosciences, US). Placebo-controlled trials using different brands of BoNTA have shown that this serotype is effective and safe for the treatment of CD.39,40,45,47 The weighted mean difference for the change in TWSTRS total score between BoNTA and placebo was -6.9 (95% confidence interval [CI] -11.25 to -2.55), according to a Cochrane Collaboration systematic review.47 There is weak evidence suggesting significant differences in efficacy and safety between Botox and Dysport and between Botox and Xeomin.39,47 The results of the trials comparing BoNTB with placebo also showed its efficacy and safety for the treatment of CD.48 The weighted mean difference for the reduction in the TWSTRS total score between BoNTB and placebo was -5.92 (95% CI -9.61 to -2.23).48 Two head-to-head trials comparing BoNTA with BoNTB showed similar efficacy; however, BoNTB was associated with more adverse events, mostly dry mouth. The occurrence of dysphagia diverged between trials, and only in one was it more common with BoNTB.41,49
Regarding the control of pain in CD, a systematic review found that in five trials in which patients were assessed for pain relief using an analogue scale, the injection of BoNTA markedly improved pain (odds ratio [OR] 11.9, 95% CI 6.3–22.5).47 Pain relief was not associated with dose, suggesting that mechanisms other than muscle weakening contribute to pain improvement after BoNT injection.47 However, the majority of the randomised controlled trials (RCTs) evaluating the efficacy and safety of BoNTA used the Tsui scale as the primary outcome measure,47 which poses a limitation because this scale does not incorporate a pain item.47
A recent RCT testing Dysport against placebo using the TWSTRS and a VAS as outcomes for pain assessment also found a marked improvement in pain after BoNT injection.40 Similar to the antidystonic effect, there seems to be no significant difference in the improvement of pain between the different brands of BoNTA.39,47 Contrary to trials of BoNTA, the primary outcome in the RCTs of BoNTB was the TWSTRS, including the pain subscale. The three RCTs of BoNTB also showed a marked improvement in pain favouring BoNT over placebo in both objective and subjective measures, with a weighted mean difference in the TWSTRS pain score of -3.70 (95% CI -5.64 to -1.76) and a weighted mean difference in the VAS of 18 (95% CI 5.69–30.31) for 5,000U of BoNTB and 19.63 (95% CI 11.69–27.56) for 10,000U of BoNTB.48 The two RCTs comparing BoNTA and BoNTB showed no significant difference in the effect size of both treatments in reducing pain.41,49 Additionally, one case series suggested that multiple points of injection per muscle of BoNTA were more effective than one in reducing pain.50
Although CD has a marked impact on quality of life, no RCT has assessed QoL as a primary outcome.39–41,46–49 Data on the effect of BoNT in the QoL of patients with CD are derived solely from five case series using BoNTA.25,27,29,51,52 They all consistently report a moderate to marked improvement in QoL, a benefit that does not correlate with the change in objective clinical severity scales, suggesting that the effectiveness of BoNT is better captured by subjective than objective scales. Hilker et al. assessed QoL in 50 patients using the EQ-5D and the SF-36.25 They found a moderate to marked improvement in QoL, mostly in the mental health and pain domains; the effect size using the EQ-5D was 0.6 for both the Utility Index (UI) (standard deviation 0.9) and the VAS (standard deviation 1.1), while the larger effect sizes using the SF-36 were found in the mental health (0.7) and pain (0.8) domains. Interestingly, no improvement occurred in the general health, emotional limitation of role and physical functioning domains. Employment predicted better improvement in QoL, whereas no correlation was found with disease duration, dosage or duration of BoNT treatment. Muller et al. recruited 131 patients and found that not only did pain have a significant impact on all domains of SF-36, it was also the main determinant of depression in patients with CD.29 Although BoNTA injections resulted in a significant improvement in dystonia, only two of the eight domains of SF-36 improved significantly, again suggesting a dissociation between improvement in dystonia and QoL. This idea is supported by another series of 101 patients with CD and 84 healthy controls: BoNTA treatment improved both scores of SF-36 (all domains) and TWSTRS, but without a correlation between each other.51 Depression was the main predictor of poor QoL, along with female gender, poor finance and living alone. In contrast to the Hilker et al. study, a longer duration of BoNT therapy predicted better QoL score.25,51
Oral Drugs
Several oral drugs have been reported to be efficacious for the treatment of CD, such as anticholinergics, antidopaminergics, dopaminergics, GABAergics, benzodiazepines and antiepileptics.53,54 Anticholinergics have prevailed as the most prescribed in clinical practice, mainly before the advent of BoNT, although the evidence supporting their use is scarce.55 There are no specific controlled trials of anticholinergics for CD; however, one RCT compared BoNTA versus trihexyphenidyl in 66 patients with CD. In this small trial, BoNTA was found to be superior to trihexyphenidyl, and also was better tolerated.56 More patients in the BoNTA arm had pain relief (TWSTRS pain subscale) compared with those in the trihexyphenidyl arm, in addition to having better scores in the QoL scale (General Health Perception Subscale of the Dutch MOS-Quality of Life Scale).
Surgical Interventions
Peripheral Surgery
Peripheral surgical techniques, either selective peripheral denervation or myectomy, have been reported to be efficacious for the treatment of patients with CD refractory to BoNT.54 Although controlled trials are not available, large case series supported the approval of selective peripheral denervation in patients with CD by the UK National Institute for Health and Clinical Excellence (NICE). These patients should be refractory to other pharmacological treatments, and the procedure should be carried out in a specialist neurosurgical centre.57–59 Only two of the three case series available evaluated pain or QoL.58,59 Munchau et al. prospectively included 62 patients, and pain was assessed by the TWSTRS pain subscale; this subscore for pain was reduced by 40 and 30%, respectively, at six and 12 months after surgery, although it increased afterwards as a possible consequence of muscle re-innervation.59 In the study by Cohen-Gadol et al., 168 patients with medically intractable CD were evaluated retrospectively.58 Pain was measured by a patient self-assessment analogue scale, and 131 patients (81%) reported a moderate to marked benefit after surgery, which was long-lasting (mean follow-up of 3.4 years) in 70 patients.58 Munchau et al. assessed changes in psychosocial function, including the EuroQol Measure of Quality of Life, in which the score significantly improved after surgery.59 The study by Cohen-Gadol et al. did not measure QoL.58
Deep Brain Stimulation
Deep brain stimulation (DBS) is largely replacing ablative surgery for dystonia, particularly DBS of the globus pallidus internus (DBS-GPi). In 2003, the US Food and Drug Administration (FDA) approved the Activa® Dystonia Therapy System under the Humanitarian Devices Exemption process for unilateral or bilateral stimulation of the GPi or the subthalamic nucleus for the treatment of chronic and intractable (i.e. drug-refractory) primary dystonia (generalised, segmental, hemi- and cervical dystonia). Controlled studies of DBS in CD are not available, and most case series report on small-sized samples with heterogeneous dystonic conditions. The Canadian multicentre, single-blind study prospectively evaluated 10 patients with disabling CD, and reported significant improvement in the TWSTRS pain subscore 12 months after bilateral DBS-GPi.60 After a mean follow-up of 32 months, Hung et al. found a 50% decrease in the TWSTRS pain subscore in 10 patients who underwent bilateral DBS-GPi for refractory CD.61 Similar results were reported by Krauss et al.62 Only the Canadian study evaluated QoL, and it found a significant improvement in SF-36 scores after surgery.60
Physical Therapy
Several rehabilitation techniques for the treatment of CD have been reported, but the data are generally of poor methodological quality.63 In the single RCT available, neither pain nor QoL was evaluated.64
Conclusions
CD is a chronic disorder that has a severe impact on the QoL of patients,24,25,27–29,31 comparable to that found in other chronic neurological disorders such as multiple sclerosis.24 Pain is present in almost two-thirds of patients with CD and represents one of the QoL domains that is most affected in CD.3,9 The main determinants for a poor QoL are depression, anxiety and pain.27–29,30,32,33
Although there are no specific trials that have evaluated the effect of pharmacological, surgical or physical treatments on pain or QoL as primary outcomes, the best data available suggest that all interventions that have improved dystonia have also alleviated pain and improved QoL domains.25,27,29,40,47,48,51,52,58,59,60,61
The relevance of pain for the management of CD suggests that treatments for CD that strictly target dystonic movements may not be sufficient to have a major impact on QoL.25,27,29,51,52 The therapeutic strategy to manage CD likely requires multiple pharmacological/ surgical interventions to target dystonia, pain, depression and anxiety in order to achieve a major decrease in the burden of disease. ■