Recently, certain aspects of trigeminal neuralgia (TN) and its management have been clarified. After a reminder of the general concepts of TN, this article describes these recent developments with regard to new views about the criteria for diagnosing symptomatic forms, clarification about medical treatment and a proposal about the choice of surgical procedures.
Recently, certain aspects of trigeminal neuralgia (TN) and its management have been clarified. After a reminder of the general concepts of TN, this article describes these recent developments with regard to new views about the criteria for diagnosing symptomatic forms, clarification about medical treatment and a proposal about the choice of surgical procedures.
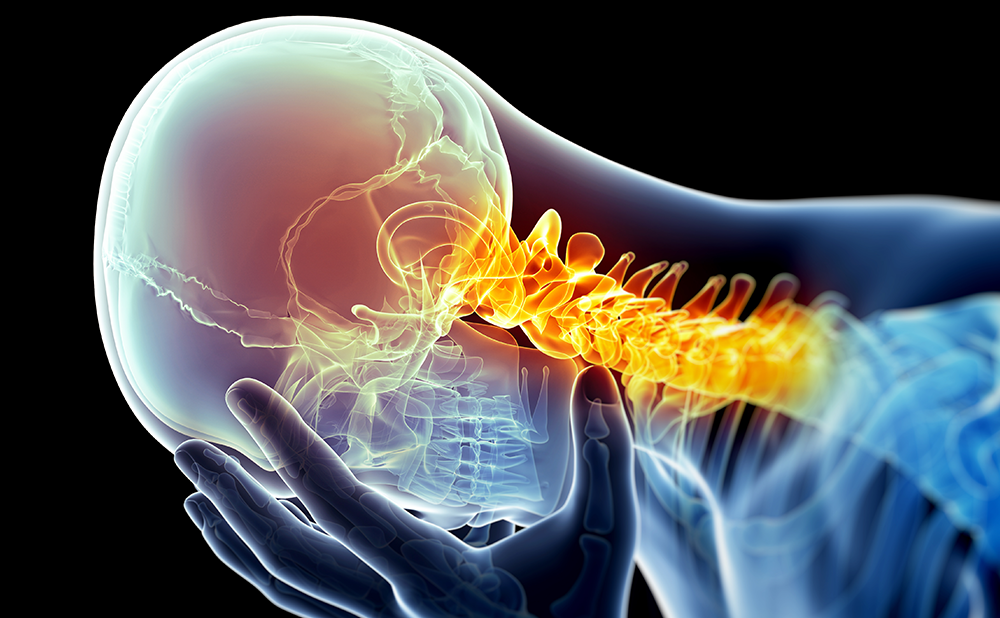
TN, or ‘tic douloureux’, is most easily recognised in medical practice as “a sudden, usually unilateral, brief stabbing recurrent pain in the distribution of one or more branches of the fifth cranial nerve”.1 TN may have no apparent cause (idiopathic, essential or classic TN) or be secondary to major neurological disease (symptomatic TN). Symptomatic TN can be related to slowly growing tumours, such as cholesteatomas, meningiomas or neurinomas of the VIII nerve that compress the trigeminal nerve root near the dorsal root entry zone, or multiple sclerosis (MS), which is typically associated with TN.2–4 Many investigators refute the term ‘idiopathic TN’ because they support the view that, when no lesion affecting the trigeminal system can be demonstrated, TN is due to a vascular compression of the trigeminal nerve root by tortuous or aberrant vessels. Microsurgical interventions in the posterior fossa always find a compressing vessel, most often the superior cerebellar artery. Further support for this view comes from magnetic resonance imaging (MRI) studies reporting a frequent contact between vessels and the trigeminal root.5 Microvascular decompression consistently relieves TN pain.6 Nevertheless, other investigators do not support the view that a vascular compression is the main factor, as compression of the trigeminal nerve root near the root entry zone is often found (in 7–12% of cases) during standard autopsy of patients with no history of TN, and on MRI TN patients may have bilateral compressions but no bilateral symptoms.7,8 Several factors possibly contribute to the development of TN. The hypothesis of a multifactorial origin is favoured by several investigators.
As the debate about the possible causes of idiopathic TN is still open, we believe that the terminology and definitions proposed by the International Headache Society (IHS)9 are the most appropriate. Classic TN has no apparent cause other than vascular compressions, and symptomatic TN is pain indistinguishable from that of classic TN but is caused by a demonstrable structural lesion other than vascular compressions.9 The categorisation of TN into typical and atypical forms is based on symptom constellation and not aetiology, thus typical TN must not be confused with classic TN.7
Although trigeminal neuralgia is classified as neuropathic pain because it is a direct consequence of somatosensory system lesion, it has unique features that make it different from other neuropathic pain. TN symptoms are unmistakable, and TN is usually recognisable by patient history alone. Pain distribution is unilateral (bilateral TN sometimes occurs in multiple sclerosis) and follows the sensory distribution of the trigeminal divisions, typically radiating to the maxillary (V2) or mandibular (V3) territories. Ophthalmic (V1) pain is less common and was previously considered indicative of symptomatic TN (see below).
Strongly indicative of a symptomatic form, a focal neuropathy is often a pain in the tongue, which is very rarely affected in classic TN. The pain is never felt in the teeth.10 The right side of the face is involved more frequently than the left, and the disorder is more common in women than in men (3:2). Pain, usually referred to as stabbing or electric-shock-like, is brief and paroxysmal, lasting a few seconds, with no pain between paroxysms. However, there is sometimes an after-pain described as slowly fading away. Pain may be provoked by stimulating cutaneous or mucous trigeminal territories (trigger zones). Gently touching the face, washing, shaving, talking, brushing the teeth, chewing, swallowing or even a slight breeze can trigger the paroxysms. Pain provokes brief muscle spasms of the facial muscles, thus producing the ‘tic’. Especially in the early years of the condition, there can be long pain-free periods; however, these remission periods gradually become shorter and shorter. Classic TN occurs more often in the sixth or seventh decade of life and is stereotyped in each individual.
Differential Diagnosis Between Classic and Symptomatic Forms
About 15% of cases are secondary to major neurological disease such as tumours or MS.7 How does one identify these patients? Traditionally, the clinical features that were considered indicators of probable symptomatic TN were bilateral pain, finding of sensory deficits, involvement of the ophthalmic division, unresponsiveness to medical treatment and onset age below 50 years.
In a recent systematic review of the evidence-based literature, a joint European–American task force arrived at conclusions that differ from the above notion in several respects.7 Bilateral pain has a 100% specificity, but its occurrence is too rare even in symptomatic TN (sensitivity 0–7%). The finding of sensory deficits is highly specific (98%), but the sensitivity is only 37%. In other words, the finding of sensory deficits or bilateral pain is an excellent indicator of symptomatic TN, but their absence does not indicate classic TN. The involvement of the ophthalmic division is equally rare in the two forms (21 and 23%, respectively). Similarly, there was no significant difference in response to treatment. The mean onset age was significantly lower in symptomatic (48 years) than in classic TN (57 years), but a histogram of onset age distribution showed that there was considerable overlap in the age ranges of the two populations. Thus, although younger age increases the risk of finding symptomatic TN, the diagnostic accuracy of age as a predictor of symptomatic TN is too low to be clinically useful. Hence, this task force concluded that it is impossible to exclude a symptomatic form on clinical grounds only, and recommended performing neuroimaging or neurophysiological investigations (see below) at least once in all patients.7 Figure 1 shows clinical and neurophysiological results in a personal series of 178 patients with classic or symptomatic TN.
Neurophysiological Investigations
According to the European Federation of Neurological Societies (EFNS) guidelines on neuropathic pain assessment and the American Academy of Neurology (AAN)–EFNS guidelines on trigeminal neuralgia management,7,11 the neurophysiological recording of trigeminal reflexes represents the most useful and reliable test for the neurophysiological diagnosis of trigeminal pains. The trigeminal reflexes (see Figure 2) consist of a series of reflex responses (R1 and R2 components of the blink reflex after electrical stimulation of the ophthalmic division; SP1 and SP2 components of the masseter inhibitory reflex after electrical stimulation of the maxillary or mandibular division) that assess function of trigeminal afferents from the three trigeminal divisions, as well as trigeminal central circuits in the brainstem.
In patients reporting pain in the trigeminal territory, trigeminal reflexes offer the clinician useful information. Abnormalities are often discovered in divisions that appear clinically unaffected. An objective demonstration of dysfunction is provided in all patients with pain secondary to a documented disease, such as symptomatic trigeminal neuralgia, post-herpetic neuralgia, vascular malformations, benign tumours of the cerebellopontine angle and MS. As a tool for disclosing symptomatic TN, neurophysiological testing of trigeminal reflexes provides the same sensitivity (95%) and specificity (93%) as MRI.12
Although more advanced techniques assessing brain responses after selective nociceptive stimulation did provide important pathophysiological information,13,14 a diagnostic protocol for patients with trigeminal pain should rely primarily on trigeminal reflexes: the technique is easy and completely harmless and the finding of any abnormality implies an underlying structural lesion. Many readers may not be aware of the electrophysiological testing of the trigeminal reflexes and, admittedly, it is easier to find an MRI scanner. However, any health unit provided with electromyography can easily perform the trigeminal reflex testing. It requires the same equipment used for a nerve conduction study and is quickly managed by a neurophysiologist. It also has the advantage of being far less expensive than MRI. Furthermore, it will probably disclose the few cases that MRI fails to detect.12 Naturally, only patients with normal repsonses can be spared MRI. Those with any abnormality must undergo MRI to ascertain the nature of the lesion.
Medical Treatment
As the mechanism leading to paroxysmal pain begins in demyelinated fibres that become hyperexcitable and generate high-frequency discharges, the ideal drugs are those that reduce neuronal excitability and, in particular, those able to limit the discharge frequency, i.e. sodium-channel blockers. Some local anaesthetics (lidocaine) and antiepileptic drugs (phenytoin, carbamazepine, oxcarbazepine, lamotrigine) belong to this category. It is worth emphasising that the drugs most commonly used in neuropathic pain, i.e. amitriptyline and gabapentin, although efficacious in many neuropathic pain conditions, have never been adequately tested in the treatment of TN, probably because they are less effective in paroxysmal pain.
According to recent guidelines,7,15 the two first-line drugs for trigeminal neuralgia are carbamazepine (CBZ) 400–1,000mg and oxcarbazepine (OXC) 900–1,800mg daily. Both drugs are very efficacious, reducing the number of attacks by more than 50% in more than 80% of patients, a proportion far higher than the 30–40% of responders achieved by any drug in other neuropathic pain conditions.15,16 The problems may come with the side effects on the central nervous system, such as drowsiness and unsteadiness. Besides these relatively common side effects, CBZ can occasionally induce leukopoenia and thrombocytopoenia. A blood count should be performed before the first administration of CBZ and thereafter three or four times a year. Numerous drug interactions can occur; this is especially important as the majority of patients are elderly and already taking medication. Oxcarbazepine was developed in order to minimise the side effects of CBZ on the CNS. OXC may induce hyponatraemia in 6–8% of elderly patients, thus it is necessary to measure electrolyte concentration during the first month of treatment.7,15,17
Although there are uncontrolled case series reporting the efficacy of several new drugs, only baclofen and lamotrigine are the second-line drugs. Baclofen18 has the advantage of a synergistic action with CBZ, but probably due to its frequent – and sometimes severe – side effects it is rarely prescribed. One randomised controlled trial19 demonstrated the efficacy of lamotrigine as add-on therapy. Oral phenytoin (historically the first antiepileptic drug used for the treatment of TN) is effective in only 25% of patients and its chronic administration has serious adverse effects.15 However, phenytoin can be administrated intravenously (IV), and thus it is useful in an emergency, when extremely frequent TN paroxysms preclude taking anything orally.20
According to the aforementioned guidelines,7,15 patients who cannot reach effective doses of CBZ and OXC due to contraindications or adverse events should try second-line drugs. Patients who do reach effective doses of CBZ or OXC but who do not experience enough pain releif become candidates for surgical interventions.
Surgical Treatment
Several surgical procedures proved to be efficacious in TN. Percutaneous procedures on the Gasserian ganglion, microvascular decompression and gamma-knife radiosurgery have proved effective. The percutaneous procedures on the Gasserian ganglion (which are also called percutaneous rhizotomies) involve penetration of the foramen ovale with a cannula and then controlled lesion of the trigeminal ganglion or root by various means: thermal (radiofrequency thermocoagulation), chemical (injection of glycerol) or mechanical (compression by a balloon inflated into Meckel’s cave). Ninety per cent of patients attain pain relief from these procedures. At four years, around 50% of patients are still painfree. Sensory loss after these percutanous procedures is present in about 50% of patients. Fewer than 6% develop troublesome dysesthesias, and 4% develop anaesthesia dolorosa. Corneal numbness, with the risk of keratitis, occurs in 4% of patients. Up to 50% of patients undergoing balloon compression experience transitory masticatory weakness. Mortality is extremely low.21–24
Gamma-knife surgery is the only non-invasive technique. It aims a focused beam of radiation at the trigeminal root in the posterior fossa. At one year after gamma-knife therapy, complete pain relief with no medication occurs in almost 70% of patients. This falls to 50% at three years. Pain relief can be delayed for a mean of one month. Sensory complications average 6%, while anaesthesia dolorosa is practically absent. No complications outside the trigeminal nerve have been reported. Quality of life improves and 88% are satisfied with outcome.25–28
Microvascular decompression is a major neurosurgical procedure that entails craniotomy to reach the trigeminal nerve in the posterior fossa. Vessels compressing the nerve are identified and moved out of contact. The procedure aims to preserve trigeminal nerve function. Ninety per cent of patients obtain pain relief. Over 80% will still be pain-free at one year and 73% at five years. The average mortality associated with the operation is 0.2%, although this may raise to 0.5% in some reports. Post-operative morbidity is lower in high-volume units.29 Up to 4% of patients incur major problems such as CSF leaks, infarcts or haematomas. Aseptic meningitis and ipsilateral hearing loss are the most common complications (about 10%). Diplopia is usually transient and facial palsy is rare. Sensory loss occurs in 7% of patients.6,30–32
Hence, all the surgical procedures yield excellent results. As mentioned in the section about medical treatment, patients resistant to the main drugs should be quickly offered the surgical option. In a study of 245 post-operative patients, over 70% would have preferred to have received surgical treatment earlier.32
The question remains: which surgical procedure? Although there are no adequately controlled studies that directly compare the different procedures, some reasoning may be of help. Microvascular decompression yields the longest duration of pain freedom and should be preferred, at least in patients with MRI-documented neurovascular compression and an age that allows general anaesthesia and craniotomy without major concern. Gamma-knife radiosurgery is the least invasive of all the procedures, but has the disadvantage that the onset of pain relief is delayed and patients with very strong pain may not be willing to wait. Furthermore, patients must be able to lie very still within the MRI machine for the duration of the treatment. The pain-relieving effects of the percutaneous procedures are of shorter duration, but these techniques are comparatively easier and quicker and many patients are not worried about repeating the intervention. The hercutaneous procedures entail some degree of sensory disturbance, and radiofrequency thermocoagulation is by no means indicated in patients with involvement of ophthalmic division because it damages the smallest fibres and thus may produce corneal numbness and keratitis. ■