Neuropathic Pain Definition, Diagnosis and Clinical Presentation
Neuropathic Pain Definition, Diagnosis and Clinical Presentation
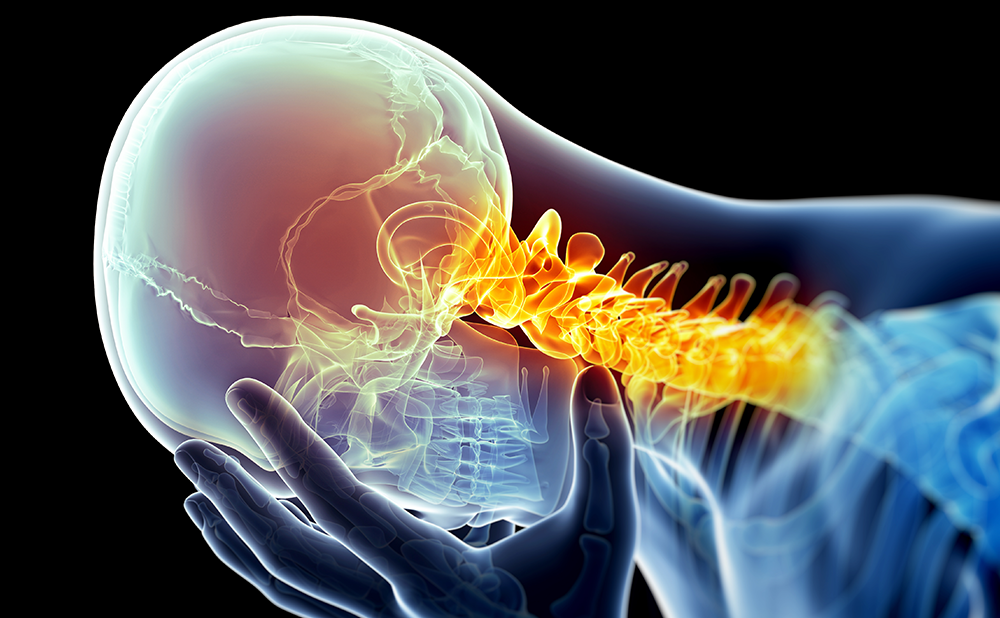
Neuropathic pain (NP) originates as a result of a lesion or disease (e.g., diabetes, herpes zoster, HIV infection, chemotherapy or surgery) pertaining to the somatosensory system.1 NP can be classified as peripheral or central depending on where the lesion/disease is located.2 The clinical presentation of NP includes both positive and negative sensory phenomena: e.g., pain and lack of sensation. The presence of NP can be categorised in three groups depending on the certainty of its existence: the ‘definite’ and ‘probable’ levels indicate that the presence of NP is established, and the ‘possible’ level does not confirm the existence of this condition.2 These levels are assigned by using the NP grading system, which consists of four criteria:
- pain with a distinct neuroanatomically plausible distribution;
- a history suggestive of a relevant lesion or disease affecting the peripheral or central somatosensory system;
- demonstration of the distinct neuroanatomically plausible distribution by at least one confirmatory test; and
- demonstration of the relevant lesion or disease by at least one confirmatory test.
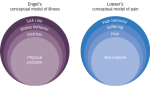
If all of the four criteria stated above are met, the diagnosis of definite NP is made. Probable NP is present if the first, second and either the third or fourth criteria are met. The diagnosis of possible NP requires the first two criteria without the third or fourth. If the patient fails to exhibit the criteria for these three levels, the NP is considered as absent.2 Commonly used recent screening tools to identify NP include Leeds assessment of neuropathic symptoms and signs, Douleur neuropathique 4 questions, Neuropathic questionnaire, painDETECT and ID Pain. Bennett et al. conducted research in 2007 investigating these five screening tools and noted that three symptomatic items (‘prickling, tingling, pins and needles’, ‘electric shocks or shooting’ and ‘hot or burning’) were found in all tools. Also ‘numbness’ and ‘pain evoked by light touching’ were present in 80 % of the tools investigated in Bennett et al.’s research.3 Quantitative sensory testing (QST) is one of the tools useful in evaluating sensation, focusing on the definition of the stimulus properties, the quantity of sensory intensity and the quality of sensation. QST, skin biopsies, imaging electrodiagnostic studies, pertinent ancillary data and the symptoms exhibited by the patient should be studied while treating the NP. The clinician should consider a ‘rational polypharmacotherapy’ for the case if a single agent is not enough to relieve the NP.4 The illness or injury preceding NP may present itself with both medical and psychiatric co-morbidities, disturbing the diagnosis and assessment of NP. Backonja and Argoff5 suggested an outline of multidimensional pain assessment (MDPA) to establish the complete clinical diagnosis of individual patients. Multiple dimensions of NP include medical aetiology, pain management, psychiatric co-morbidities and quality of life/ability to function. Ranking each dimension as ‘none’, ‘mild’, ‘moderate’ or ‘severe’ helps assess multidimensional pain.
Treatment of Neuropathic Pain
The treatment of NP is difficult because less than half of patients receive satisfactory pain relief (>30 % reduction) while side effects are common. Although being treated with multiple medications, studies have shown that NP patients continue to have pain of moderate severity.6 O’Connor states that this inefficacy may result in part from inappropriate medication prescription or use of insufficient dosage in treating these patients. The Neuropathic Pain Special Interest Group (NeuPSIG) outlined three lines of medications to treat NP.7 Combinations of medications appear to provide greater pain relief compared with monotherapy, although there is not a great deal of evidence surrounding combination therapy. There are also non-pharmacological approaches to the treatment of NP which include: physical medicine approaches, behavioural approaches, interventional approaches, surgical approaches and neuromodulation approaches.
Medication Management of Neuropathic Pain – Current Recommendations
The International Association for the Study of Pain (IASP) NeuPSIG, an international consensus process that included a diverse group of pain experts, was convened to develop evidence-based guidelines for the pharmacological treatment of NP. These guidelines were endorsed by the American Pain Society, the Canadian Pain Society (CPS), the Finnish Pain Society, the Latin American Federation of IASP Chapters and the Mexican Pain Society.7 Additional consensus guidelines for the pharmacological treatment of NP were created simultaneously by the European Federation of Neurological Societies (EFNS)8 and the CPS.9 The first-line agents for NP recommended by the IASP NeuPSIG included: tricyclic antidepressants (TCAs), calcium channel α2-δ ligands, selective serotonin/norepinephrine re-uptake inhibitors (SNRIs) and topical lidocaine (for localised peripheral NP).7 Opioids and tramadol were recommended as second-line agents except in selected circumstances, such as the treatment of acute NP, episodic exacerbations of severe NP and neuropathic cancer pain and during the titration of a first-line agent in patients with severe pain.7 The CPS guidelines recommended TCAs and calcium channel α2-δ ligands as first-line medications.9 SNRIs and topical lidocaine (for localised peripheral NP) were recommended as second-line medications and opioid analgesics and tramadol were recommended as third-line analgesic agents for the treatment of NP.9 In 2010, the EFNS updated its guidelines.10 Recommendations for first-line agents for diabetic NP included: duloxetine, gabapentin, pregabalin, TCAs and venlafaxine extended-release. Opioids and tramadol were recommended as second-line agents for diabetic NP. Recommendations for first-line agents for postherpetic neuralgia (PHN) were gabapentin, pregabalin, TCAs and lidocaine plasters with opioids and topical capsaicin (topical 0.075 and 8 % capsaicin patch [Qutenza®]). Recommendations for first-line agents for central pain were gabapentin, pregabalin and TCAs.10
Antidepressants
Antidepressants are a heterogeneous group of drugs which have all demonstrated beneficial activity for patients with major depressive disorder. Antidepressants can be classified in multiple ways; however, a simplistic yet clinically useful categorisation divides them into TCAs, SNRIs, selective serotonin re-uptake inhibitors (SSRIs) and selective norepinephrine (noradrenalin) re-uptake inhibitors (NRIs or NARIs).
Tricyclic Antidepressants
The TCAs can be divided into amines and their demethylated secondary amine derivatives. The tertiary amine TCAs include the following:
- amitriptyline (Elavil®);
- imipramine (Tofranil®);
- trimipramine (Surmontil®);
- clomipramine (Anafranil®); and
- doxepin (Sinequan®).
The secondary amine TCAs include the following:
- nortriptyline (Pamelor®);
- desipramine (Norpramin®);
- protriptyline (Vivactil®); and
- amoxapine (Asendin®).
In 1987, Max et al. demonstrated that TCAs possess analgesic effects independent of their effects on moods.11 Furthermore, as a generalisation it was found later on that the analgesic effects from TCAs tend to occur more rapidly (at roughly a week or less after initiating TCA therapy) and at lower doses than those used for antidepressant effects. TCAs have been extensively used in the treatment of different types of NP and multiple randomised controlled trials (RCTs) have demonstrated their efficacy for various types of NP, excluding pain in HIV and chemotherapy-induced peripheral neuropathies.12–14 The mechanism of action of TCAs includes both norepinephrine and serotonin re-uptake inhibition. Certain TCAs, such as amitriptyline and doxepin, have demonstrated sodium channel blocking ability as well. Among the most commonly used TCAs are nortriptyline and desipramine, not only because of their analgesic properties but because of their fewer side effects in comparison with other TCAs (tertiary amines) such as amitriptyline.15,16 TCAs may exhibit a wide range of adverse effects and differ significantly as regards which TCAs have which effects. Adverse effects include: anticholinergic effects (desipramine has the least anticholinergic effects), antihistaminergic effects (doxepin has the most potent antihistaminergic effects), α-1 adrenergic receptor blockade (e.g., orthostatic hypotension) and cardiac effects (increasing intraventricular conduction, prolonged QT interval, prolonged through the atrioventricular node). Other side effects of TCAs include orthostatic hypotension as well as those related to their anticholinergic activity including urinary retention, dry mouth and constipation. Cardiac toxicity has been described as a possible side effect of TCAs; sinus and ventricular arrhythmias were noted in patients with a history of coronary artery disease (CAD) and depression who were on nortriptyline.17 A large review study has shown some cardiac complications, including myocardial infarction, with doses more than 100 mg/day, but did not demonstrate adverse cardiac outcomes in patients who were on a regimen of less than 100 mg/day.18 One of the advantages of TCAs is that they are taken once daily and are not expensive. When committing a patient with NP to treatment with TCAs, the lowest effective dose should be used. In patients with a history of arrhythmias and CAD, TCAs should be avoided and obtaining an electrocardiogram prior to starting treatment in patients over 40 years old is recommended.19
Multiple reviews have evaluated that placebo-controlled RCTs found TCAs to be efficacious for several different types of NP.7,12,14,20–22 In older persons, TCAs, especially tertiary amines such as amitriptyline, may exhibit too many adverse effects to be used. In fact, over time, amitriptyline consistently appears on the Beers list23,24 of medications that are suggested to be inappropriate when treating older persons. Thus, in frail older patients, duloxetine may be a reasonable choice and clinicians may trial an initial dose of half a tablet for a week to assess how well they tolerate this medication. Duloxetine is also available in 20 mg tablets for old and frail patients.
Although the role of SSRIs in providing effective analgesia is uncertain, it appears limited at best.22
Selective Serotonin/Norepinephrine Re-uptake Inhibitors
Duloxetine and venlafaxine are antidepressants with both serotonergic and noradrenergic re-uptake inhibiting properties (SNRIs). The former has been extensively studied and used in the treatment of diabetic neuropathy and has been demonstrated to be efficacious over placebo in multiple RCTs that showed doses of 60 and 120 mg/day to be both safe and effective.25–27 The side effect profile of duloxetine seems to be more favourable than TCAs, especially with respect to anticholinergic and cardiac side effects. Nausea has been reported as one of the common side effects and is reduced by lowering the dose.28 For many patients, nausea is self-limited and resolves within the first several weeks of usage. Duloxetine has been extensively studied in patients with diabetic peripheral neuropathy, fibromyalgia, musculoskeletal back pain and osteoarthritis, and is US Food and Drug Administration (FDA)-approved for all four indications. Venlafaxine has been effective in the treatment of diabetic painful neuropathy (DPN) and other polyneuropathies, except PHN.7 A small subset of patients demonstrated cardiac conduction abnormalities; thus precautions should be taken in patients with a history of cardiac pathologies. Venlafaxine should be tapered rather than abruptly discontinued because of a withdrawal syndrome that has been reported.29 At doses less than 150 mg/day, venlafaxine behaves more like a serotonergic-specific re-uptake inhibitor or SSRI; at doses above 150 mg, it behaves more like an SNRI agent and pain relief is more likely to occur with doses of 150 mg/day or greater. Venlafaxine is not FDA-approved for any pain indication.
Calcium Channel Alpha-2 Delta Ligands
Gabapentin and pregabalin are calcium channel α2-δ ligands. The mechanism of action of each of these is through their ability, in an excited neuron, to reduce calcium influx into the neuron with subsequent reduction of neurotransmitter release such as substance P, glutamate and norepinephrine.30–36 Although calcium channel ligands can lead to dose-dependent somnolence and dizziness, as well as weight gain and peripheral oedema, they have few drug–drug interactions. Their dose must be lowered in patients with renal insufficiency.7 Another advantage of pregabalin is that it has some anxiolytic effects, which is frequently helpful with concurrent anxiety seen in patients with NP.37 Gabapentin is FDA-approved for PHN. Pregabalin is FDA-approved for PHN as well as DPN and fibromyalgia.
Gabapentin exhibits non-linear pharmacokinetics. That is, as doses are increased, less of the drug is absorbed and therefore much of it is excreted in the urine rather than being clinically effective. It should be introduced to a patient in a low-dose fashion and increased until analgesia has been achieved or side effects are experienced. The maximum recommended dosage of gabapentin is 3,600 mg/day for DPN and 1,800 mg/day for PHN and its effect can be seen as soon as two weeks, although an adequate therapeutic trial can take up to several months.1 Gabapentin is now available in extended-release formulations. Although pregabalin and gabapentin have identical mechanisms of action, pregabalin has improved pharmacokinetics and linear bioavailability, both of which are significant advantages. Its onset of analgesia is faster than gabapentin, secondary to its shorter titration period. The current recommendations are titration up to 300 mg/day divided into three doses for DPN and up to 600 mg/day divided into three doses for PHN.1 For maintenance treatment it is generally dosed twice a day (bid). However, some elderly patients or those patients more sensitive to medication may prefer taking a lower dose three times a day (tid). The doses for both gabapentin and pregabalin should be reduced in patients with chronic kidney disease.
Topical Lidocaine
The lidocaine patch 5 % is FDA-approved for the treatment of PHN and may be used as a part of multimodal therapy. Several RCTs have established its efficacy over placebo. The mechanism of action is a result of sodium channel blocking of hyperactive sodium ions in damaged peripheral nerves and interference with ectopic impulses ascending to the dorsal horn. This interferes with peripheral and central sensitisation and decreases the likelihood of maladaptive neuroplasticity. In addition, the patch itself is a buffer which decreases mechanical allodynia.38,39 The most common side effect of the patch is mild skin irritation. The patch should not be used in patients sensitive to lidocaine or type 1 antiarrhythmics such as tocainide or mexiletine. It should not be used in patients with hepatic insufficiency since lidocaine is metabolised by the liver. Lidocaine crosses the placental barrier and therefore should not be used in pregnancy or by nursing mothers. The 5 % lidocaine patch and 5 % lidocaine-medicated plaster are safe and appear to be effective and well-tolerated by patients with PHN and allodynia.13,40–46 Patients with a small focal area of well-localised NP may benefit from topical lidocaine the most.47 Since the drug is not absorbed systemically, there are no systemic adverse effects. Mild local reactions are the most common side effects.
Opioids
Opioids and tramadol may provide analgesia in multiple NP conditions and multiple RCTs have supported their use.1,7 Because of their side effects, which occur more frequently than with the first-line medications and the risk of misuse, opioids are not recommended as a substitute for the first-line medications.48 They should be reserved for patients who have failed the first-line regimen, for pain relief during the titration of the first-line medication, for treatment of episodic severe NP and for neuropathic cancer pain. The most commonly reported side effects of opioids are constipation, nausea, vomiting and sedation. It is recommended to start patients on a bowel regimen to prevent the gastrointestinal symptoms. Moreover, chronic use of opioids may be associated with immunological changes, endocrine changes (e.g., hypogonadism) and the possible development of hyperalgesia. Opioids are not FDA-approved for specific NP conditions. Eisenberg et al. performed a systematic review and meta-analysis and found 22 articles that met inclusion criteria (14 were short-term and eight were intermediate-term).49 Short-term studies provided equivocal evidence of opioid efficacy for providing analgesia in NP, but all eight intermediate-term studies demonstrated significant efficacy of opioids over placebo for reducing NP.49
Tramadol
Tramadol is a racemate, with the (+) enantiomer having weak opioid properties and binding to the μ opioid receptor which accounts for about 30 % of its analgesic activity. The (+) enantiomer also inhibits the re-uptake of serotonin and the (-) enantiomer inhibits the re-uptake of norepinephrine. Tramadol is available in short- and extended-release preparations and the recommended starting dose for the immediate-release tramadol is 50 mg every 6–8 hours. Because of the risk of seizures at higher doses, there is a maximum recommended dose of 400 mg/day. This regimen should be adjusted for patients with kidney or liver pathology.1 Tramadol is not FDA-approved for any NP indications.
N-Methyl D-Aspartate Receptor Antagonists
Inconsistent outcomes for the use of memantine and dextromethorphan have been observed; however, they have been occasionally tried with patients who failed other therapies.7,12 Dextromethorphan is effective in a dose-related fashion in selected patients with DPN but not in PHN.50
Alpha-2 Adrenoceptor Agonists
There are three α-2 adrenoceptor agonists FDA-approved for use (not analgesic use) in the US. The agents all have antinociceptive properties and may be especially useful when used in conjunction with muscular spasticity/spasms or concomitantly with opioids. Clonidine is primarily used as an antihypertensive agent. It is available in various formulations for multiple routes of administration including oral, sublingual, transdermal, intravenous and epidural. Tizanidine is primarily used as a muscle relaxant/antispasticity agent in an oral tablet form.
Topical Capsaicin
A high-potency (8 %) capsaicin patch (Qutenza) is FDA-approved for the treatment of PHN pain. It is thought to diminish pain sensation by reducing transient receptor potential vanilloid-1 (TRPV1) expression and decreasing the density of epidermal nerve fibres in the application area. A single 60-minute application may provide up to 12 weeks of analgesia. Derry et al. performed a Cochrane Review in 2009 which included six studies (389 participants) comparing 0.075 % capsaicin cream with placebo cream and two studies comparing 8 % capsaicin patch with placebo patch.51 They concluded that capsaicin, either as repeated application of a low-dose (0.075 %) cream or a single application of an 8 % patch may provide a clinically significant degree of pain relief to some patients with NP.51
Combination Therapy
The use of ‘rational polypharmacy’ in pain management has not been particularly well studied. Gilron et al. have shown that the combination of gabapentin and morphine achieved better analgesia at lower doses of each drug than either as a single agent for NP48 and that the combination of gabapentin and nortriptyline seems more efficacious than either drug administered as monotherapy for NP.52
Potential Future Agents
Conventional available agents for the treatment of NP remain suboptimal for providing adequate analgesia for all patients with NP. Novel analgesic agents are needed in efforts to improve pharmacological approaches to combating NP. Potential therapeutic options in the future may include: purinergic receptor modulators, cannabinoid receptor modulators, neurokinin-1 (NK-1) receptor modulators, glial modulators, rostral ventral medulla on-cell modulators (e.g., improgan), chemokine receptor modulators, toll-like receptor modulators, modulators of tetrahydrobiopterin synthesis and/or chemically re-engineered conotoxins.
Summary
NP is an extremely complex and challenging problem. Despite the availability and employment of multiple treatment guidelines/algorithms, a significant subpopulation of patients with NP still do not achieve adequate analgesia. At least from the standpoint of pharmacological approaches to the treatment of NP, this is probably due in part to available agents not significantly affecting important potential therapeutic targets. It is hoped that the development of novel therapeutic agents may expand the achievement of satisfactory analgesia to a larger population of patients currently suffering with NP.