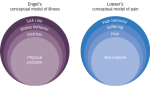
Specifying the previous definition given by the International Association for the Study of Pain (IASP), neuropathic pain has recently been re-defined by the Neuropathic Pain Special Interest Group (NeuPSIG) as “pain arising as a direct consequence of a lesion or disease affecting the somatosensory system”.1 This re-definition eliminates the term ‘dysfunction’ from the IASP definition and introduces ‘disease’ instead, and replaces ‘nervous system’ with ‘somatosensory system’ to distinguish neuropathic pain from secondary pain syndromes (e.g. spasticity-induced pain). Neuropathic pain can be caused by a variety of factors leading to a lesion or a disease of the somatosensory system. These include inflammation, ischaemia, haemorrhage or trauma of the peripheral and central nervous system. Neuropathic pain is frequent: the estimated prevalence of neuropathic pain in the general population ranges from 3.3 to 8.2 %.2 This wide range is mainly due to methodological differences between studies, which use different assessment tools and questionnaires.
Guidelines for the Assessment of Neuropathic Pain
Currently, three major guidelines are available with recommendations for the assessment of neuropathic pain: the guidelines of the German Neurological Society (Deutsche Gesellschaft für Neurologie, DGN),3 of the European Federation of Neurological Societies (EFNS)4 and of NeuPSIG.2 All three guidelines assess the methods that are currently available for the investigation of neuropathic pain. The new proposed definition of neuropathic pain1 is applied in all of these guidelines. In this article, the main recommendations of the three guidelines are summarised. Table 1 provides a synopsis of the examinations and questionnaires recommended and not recommended in each guideline. Table 2 summarises the currently available questionnaires for pain chronification, screening for neuropathic pain and assessment of neuropathic pain symptoms and signs.
Guidelines of the German Neurological Society
The 2008 guidelines of the DGN include one chapter on the diagnosis of neuropathic pain, giving the following recommendations.3 A detailed patient history with information not only about possible reasons for neuropathic pain but also about the characteristics of neuropathic pain and a thorough neurological examination are strongly recommended. The neurological examination should determine a somatosensory profile and delineate possible neurological deficits. It is also helpful to assess the degree and extent of plus and minus symptoms associated with neuropathic pain. Plus symptoms include spontaneous or evoked pain, itching, static or dynamic allodynia (i.e. pain on application of normally non-painful stimuli such as a light touch) or hyperalgesia (i.e. increased pain on application of painful stimuli such as pinprick); minus symptoms include hypesthesia or hypalgesia. For the assessment of pain intensity (including current intensity, maximum intensity and average intensity over a defined period), the application of visual or numerical rating scales (VRS and NRS, respectively) is recommended. The degree of possible pain chronicity should also be investigated by pain chronification scales. For this purpose the Graded Chronic Pain Scale (GCPS)5 or the German Mainzer-Chronifizierungsbogen6 can be used. Self-employed pain diaries are recommended for tracking the temporal course of neuropathic pain in patients and for documentation of the consumption and effect of analgesic drugs over time. The DGN guideline also recommends the use of self-employed pain drawings to record the exact location of pain. A number of pain questionnaires have been designed to assess neuropathic pain components. The DGN emphasises painDETECT as one of these questionnaires that has been validated in German for the assessment of neuropathic pain components in back pain.7
Besides these methods (patient history, neurological examination, pain questionnaires, pain drawings, pain rating), it is recommended to use further methods to identify the lesion in the somatosensory system that is leading to neuropathic pain. These methods mainly include neurophysiological studies and imaging techniques. It is important to note that routine neurophysiological studies assess the thickly myelinated large fibres, while the thinly myelinated and unmyelinated small fibres (A-delta and C fibres) cannot be studied with these techniques. For the examination of small fibres, specific tools are recommended such as quantitative sensory testing (QST) for function and skin-punch biopsy for morphology. QST is a psychophysical measure of sensory perception on application of defined thermal and mechanical stimuli. The examination will provide a sensory profile of the patient, investigating the different fibre classes. Laser-evoked potentials (LEPs) are recommended as an objective method to investigate A-delta fibres. In some cases with focal neuropathic pain, imaging techniques such as magnetic resonance tomography (MRT) can be helpful. In specific cases such as post-herpetic neuralgia, the investigation of the spinal cord with MRT and the examination of cerebrospinal fluid (CSF) via lumbar puncture are recommended. In central neuropathic pain syndromes, additional evoked potentials (sensory and motor) are necessary. Further laboratory measurements are recommended only in the presence of specific diseases, since as yet there is no biomarker available for the diagnosis or follow-up of neuropathic pain.
Guidelines of the European Federation of Neurological Societies
The 2010 guidelines of the EFNS have revised the previous EFNS guidelines of 2004.4 A detailed patient history is recommended followed by a thorough neurological examination to confirm the presence of a neuropathic syndrome and to reach an aetiological diagnosis. Additionally, the application of screening tools and pain assessment questionnaires is recommended. Suggested screening tools are the Leeds Assessment of Neuropathic Symptoms and Signs (LANSS)8 and the S-LANSS (for self-report).9 Patient assessment with LANSS is based on analysis of the sensory description of pain and on bedside examination of sensory dysfunction such as allodynia or hyperalgesia. The Neuropathic Pain Questionnaire (NPQ)10 investigates pain quality based on the description of the patient; sensory, affective and sensitivity items are examined. The Douleur Neuropathique en 4 Questions (Neuropathic Pain in 4 Questions, DN4)11 was designed to distinguish patients with chronic pain associated with neurological or somatic tissue injuries using pain descriptors and a simple bedside examination. The painDETECT questionnaire was developed and validated in Germany7 to identify neuropathic pain components in back pain. The Standardised Evaluation of Pain (StEP)12 is a recently validated questionnaire for patients with low-back pain and neuropathic pain. One of the recommended main assessment questionnaires is the Neuropathic Pain Scale (NPS),13 which however is said to lack some pain qualities frequently found in neuropathic pain. Therefore, the Pain Quality Assessment Scale (PQAS)14 has been developed, but this questionnaire has not yet been used in blinded neuropathic pain trials. An alternative questionnaire is the Neuropathic Pain Symptom Inventory (NPSI),15 which has been submitted for validation in 50 languages. The EFNS recommends the use of these screening tools to identify potential patients with neuropathic pain. However, since 10–20% of patients with neuropathic pain will not be detected by these screening tools alone, they do not replace the clinical evaluation of the patient. The NPS or the NPSI are recommended to evaluate the effects of treatment on neuropathic pain symptoms.
The EFNS guideline recommends that QST can be used in the clinic along with bedside tests to document the sensory profile of the patient. However, QST is not considered sufficient to distinguish non-neuropathic from neuropathic pain. QST is considered helpful to quantify treatment effects on allodynia and hyperalgesia. For the assessment of mechanical allodynia or hyperalgesia, the use of a brush and a high-intensity pinprick or von Frey filament is recommended. The systematic investigation of thermal stimuli is recommended only for pathophysiological research or treatment trials. Skin-punch biopsy is a minimally invasive method for the visualisation of intraepidermal A-delta and C fibres. It is recommended in patients with burning feet and clinically suspected small-fibre neuropathy.
The EFNS guidelines recommend standard neurophysiology for the assessment of large fibres and for the documentation of peripheral neuropathies. Microneurography is assumed to be a useful and safe tool for the neurophysiological examination of small fibres.16 Microneurography allows single-axon recordings from peripheral nerves; however, the technique is time-consuming, is available in only a few centres and so far has been applied only in a small number of patients; also, normative values are not available. Microneurography is therefore not yet recommended for the assessment of patients with peripheral neuropathies and neuropathic pain. Pain-related reflexes may be diagnostically useful for symptomatic forms of trigeminal neuralgia.17 Among pain-related evoked potentials, LEPs elicited via A-delta fibres are currently the most reliable potentials to assess the nociceptive pathway. For the other pain-related evoked potentials (e.g. those elicited by electric current or heat), the available evidence is not yet considered sufficient to recommend these techniques in clinical practice.
The most extensively investigated methods of functional neuroimaging in the assessment of neuropathic pain are functional MRT (fMRT) and positron-emission tomography (PET). The data so far support the notion that spontaneous neuropathic pain is associated with a decrease in contralateral thalamic blood flow, whereas provoked neuropathic pain is associated with an increase in contralateral thalamic blood flow. Functional imaging techniques are not yet recommended by the EFNS guidelines for routine investigation of patients with neuropathic pain.
Guidelines of the Neuropathic Pain Special Interest Group on Neuropathic Pain Assessment
The recently published 2010 NeuPSIG guidelines2 on neuropathic pain assessment had several aims: to assess the incidence and prevalence of neuropathic pain; to evaluate the sensitivity of the methods available to investigate neuropathic pain; to evaluate the methods available for assessing neuropathic pain treatment and to propose future studies on unsolved topics in neuropathic pain.
Of the screening tools for neuropathic pain, the NeuPSIG guideline recommends the LANSS and S-LANSS, the NPQ, the DN4, painDETECT and ID-Pain18 as tools to identify patients with neuropathic pain, especially when used by non-specialists. A questionnaire validated in the patient’s native language is preferred. Ten to 20% of patients with neuropathic pain will not be detected by these questionnaires; therefore, these questionnaires cannot replace clinical examination and judgement. Clinical examination is recommended as a crucial part of the diagnostic process in neuropathic pain, with sensory testing being the most important factor (including tests for touch, vibration, pinprick, cold and warmth detection). QST assessing the complete somatosensory profile of the patient in a blinded manner is recommended together with bedside testing. The NeuPSIG guideline recommends NRS and VRS for the assessment of pain intensity, and the NPS and the NPSA for the assessment of treatment response. The short version of the McGill pain questionnaire (SF-MPQ) has been used in a number of treatment trials, although it has not been formally validated for neuropathic pain. For the assessment of overall change of neuropathic pain under treatment, the use of the Global Impression of Change reported by the patient (PGIC) or reported by the physician (CGIC) and pain relief scales is recommended.
Regarding the available laboratory tests to investigate neuropathic pain, the NeuPSIG guideline focuses on reflexes, evoked potentials, microneurography, functional brain imaging and skin biopsy. The A-beta-fibre-mediated trigeminal reflexes are considered useful for the differentiation of symptomatic and idiopathic trigeminal neuralgia. In patients with structural damage leading to symptomatic trigeminal pain (e.g. trigeminal neuropathy), the trigeminal reflex is abnormal. Regarding the methods available to induce and record evoked potentials in neuropathic pain, the NeuPSIG guidelines recommend LEP for the investigation of A-delta fibres to subcortical pathways. Microneurography is considered a useful technique for the investigation of different peripheral nerve fibre types. This method is not currently recommended by the NeuPSIG guidelines for the routine assessment of neuropathic pain because only selected and small patient groups have been investigated to date. Similarly, functional brain imaging with fMRT and PET is not yet recommended for routine neuropathic pain assessment. However, the converging evidence for decreased activity in the contralateral thalamus is mentioned in the NeuPSIG guidelines. The minimally invasive technique of skin-punch biopsy is recommended in patients with clinical signs of small-fibre impairment to determine the intraepidermal nerve fibre density (IENFD). The investigation of IENFD can also be used as a follow-up tool to examine treatment response in patients with diabetic small-fibre neuropathy. Owing to a lack of appropriate data, the use of peripheral nerve blocks and intravenous drug infusion tests is not recommended by the NeuPSIG guidelines.
Conclusions and Future Challenges
Although the equipment for the assessment of neuropathic pain has been substantially replenished in recent years, further improvement is still needed. There is a lack of adequate tools for the assessment of mixed pain (nociceptive and neuropathic pain) and for the distinction of mixed pain from other pain states. Further studies are necessary to evaluate the specificity and sensitivity of tools such as microneurography and evoked potentials (e.g. contact/heat-evoked potentials and pain-related evoked potentials) in assessing neuropathic pain. These methods have the potential to allow the investigation of possible structural and functional changes in distinct fibre types and may thus allow a better subclassification of neuropathic pain. In addition, the search for suitable biomarkers of neuropathic pain has not yet yielded reliable and routinely usable results. Further studies are warranted to investigate local or systemic markers that may be used as diagnostic tools and in follow-up. Functional brain imaging is a very promising tool in attempts to visualise pain. However, more data are needed in controlled and precisely defined patient groups.
Independent of the method used, strictly defined and well characterised patient groups should be investigated in comparison with adequately matched healthy controls. These groups need to be large enough to allow reliable and reproducible results. All measurements should be performed by well trained investigators to minimise technical or methodological bias. The measurements and data assessment should be performed in a blinded manner. A method should be assessed in at least two different laboratories before being recommended for the assessment of neuropathic pain. Improving the methods will also give further insights into the pathophysiology of neuropathic pain. This in turn will help to improve the classification of pain syndromes that are not covered by the new definition of neuropathic pain, such as complex regional pain syndrome or fibromyalgia syndrome. ■