Opioid therapy has become a mainstay for the treatment of chronic pain, despite evidence that these medications may be ineffective and even unsafe in this patient population.1,2 In patients with chronic back pain, the use of first-line medications (non-steroidal anti-inflammatory drugs and acetaminophen) declined by 48% from 1999 to 2010; simultaneously, there was a 53% rise in narcotic prescriptions.3 This dramatic increase in opioid prescription is often attributed in part to the standards for pain treatment introduced by the Joint Commission in 2000.4 These standards, coupled with intense pharmaceutical marketing and unsupported claims that the risk of addiction from opioids is low, led to the increasingly aggressive use of opioid analgesics to manage chronic pain.5,6
Concurrent with the increased rates of opioid prescription, deaths related to opioid overdose have increased as well, tripling in the period from 2000 to 2014.7 Importantly, long-term opioid therapy may be associated with other significant adverse effects, such as respiratory depression, cognitive impairment, sexual dysfunction and constipation.8 In addition, chronic opioid use has also been linked to tolerance and opioid-induced hyperalgesia, limiting the efficacy of use in patients with chronic pain.9
In 2016, the Centers for Disease Control and Prevention (CDC) published a guideline on opioid prescription for chronic pain with recommendations on several issues, including opioid selection and dosage.10 The 2016 CDC recommendation on opioid dosage generated controversy and was not uniformly embraced by physicians caring for patients on chronic opioids.11 Nonetheless, the national call for more responsible opioid prescribing led many physicians to strongly consider alternative forms of effective pain relief.12 In 2019, the Department of Human and Health Services convened a task force on ‘Pain Management Best Practices’, and in late 2022, the CDC published an updated guideline for prescribing opioids for pain.13,14 Current guidelines support the use of chronic opioid therapy in a multimodal approach that addresses the biological, psychological and environmental factors that contribute to the chronic pain landscape.13–17 Recent recommendations on the best practice for pain management place emphasis on individualized and patient-centred care, which uses state-of-the-art pain management strategies. Other recommendations include improving patient access to care and the education of providers, patients and the general public.13,15
The complex nature of pain poses a challenge to providing effective treatment to many patients. Multidisciplinary and multimodal therapeutic approaches based on a biopsychosocial model may help improve the care of these patients.13,15 Multimodal treatment strategies include behavioural approaches (e.g. cognitive behavioural therapy), physical therapy and interventions such as anaesthetic and steroid injections, nerve blocks and neuromodulation using implanted devices.17,18 Use of non-pharmacological methods and/or interventional modalities may reduce the need for long-term opioid use in patients with chronic pain. For example, implantation of a spinal cord stimulator was associated with a lower rate of opioid use (13% versus 42%) in a study of 45 patients with persistent radicular pain after lumbosacral spine surgery.19
Despite these guidelines, patients continue to request opioids more than any other medication for chronic pain.20 There is little information in the literature on how patients’ beliefs regarding optimal pain management influence care. Hence, we sought to better understand the beliefs about optimal pain management strategies among patients with chronic pain. This information may be helpful in guiding public health education on opioid use and may improve how we educate and counsel patients on their options for chronic pain management.
Methods
We were interested in examining how patients perceived and compared various treatment options for pain. We did not find a previously published survey of this kind, although patient surveys have been conducted in an attempt to individualize pain medications based on the patient’s report of the effectiveness of the medication.21 In our study, we sought to find out whether 1) patients were aware of options beyond medication management and, if so, 2) how receptive they were to therapies for chronic pain beyond medication management. In addition, we noticed variable pushback from third-party insurers to cover or pay for therapies (other than medication management) that interfered with access to care for some patients. Along those lines, we thought that information about how patients felt about their treatment choices and what ‘worked’ for them may be useful when addressing the inconsistent medical coverage among the third-party payers.
Since we found no comparable data on this topic, we designed a pilot study to survey 200 patients in our pain clinic. The study design was predicated on a questionnaire assessing patients’ perceived susceptibility, barriers and benefits related to pain management. With the Institutional Review Board’s approval, patients with chronic pain were randomly surveyed at the GW Spine and Pain Center between May 2019 and February 2020. Inclusion criteria were adult patients with chronic pain aged 18 years or over and who received on-going treatment at the centre. Patients were not selected based on the type or severity of the disease. The exclusion criterion was patient refusal to participate in the survey.
The study used a seven-item Likert scale questionnaire that asked patients to identify perceived barriers and facilitators in accessing treatment for pain (Figure 1). The questionnaire was derived from previously validated questionnaires that used the Health Belief Model to evaluate patient beliefs about obtaining general medical care.22 Themes of the questionnaire included time taken for treatment, access to other treatment modalities, ambivalence, patients’ knowledge of treatment options and patient’s beliefs.
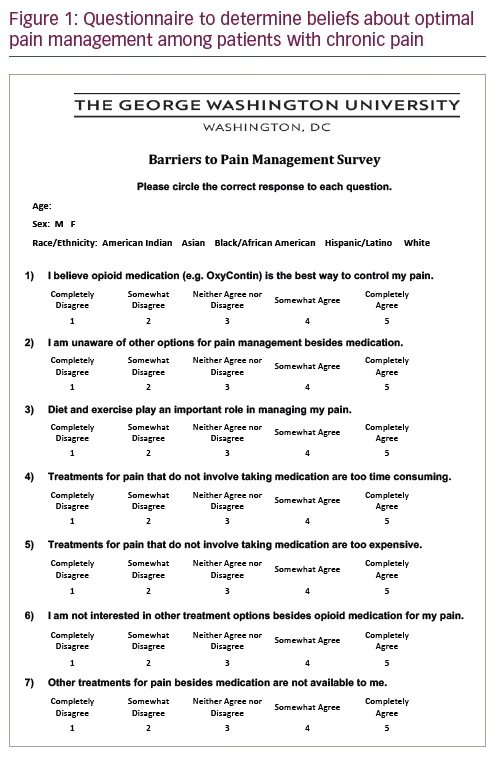
Research participants were given the questionnaire at the beginning of the visit and asked to complete the questionnaire before leaving the clinic. Each participant gave written informed consent. In addition to answering each question, participants self-reported basic demographic information, including sex, race, age, insurance status and pain treatment status (e.g. taking opioids, receiving injections). The survey was anonymous. At the time patients were given the survey, it was clarified that the term ‘treatments’ on the survey included all the different types of treatments, if any, that they may have had for their chronic pain. In an attempt to limit bias, all patients who met the inclusion criteria were invited to participate in the study. The participant responses were then statistically analysed using the chi-squared test. Correlations between responses were also studied where appropriate using Pearson’s correlation coefficient. Responses were grouped by “completely disagree”, “somewhat disagree”, “neither agree nor disagree”, “somewhat agree” and “completely agree”. A p-value of 0.05 was chosen to determine statistical significance. Answer choices of “neither agree or disagree” were not included in the analyses.
Results
In this pilot study, the vast majority of participants surveyed were returning patients. The duration of pain varied from several months to several years. In our clinic, the most common complaint was back pain, followed by neuropathic pain in either the upper or lower extremities. A few patients presented with generalized pain, which, in our clinic, was most commonly associated with the diagnoses of fibromyalgia or post-laminectomy syndrome. During each clinic visit, the patient was assessed for the efficacy of pain control, including the risks and benefits of the current regimen. If there was room for improvement, other pain management strategies in line with best practice recommendations were discussed.15 These options included but were not limited to various pharmacotherapies, including complementary and integrative modalities; non-pharmacological options, such as physical therapy, and interventional procedures; and behavioural health therapies, including mindfulness meditation and stress-reduction techniques. On arrival at each visit, the patient routinely completed a questionnaire that included basic psychological and psychiatric screening questions. Psychological distress was rarely encountered; however, some patients might report stress from the impact of chronic pain on day-to-day functioning and quality of life. For each patient seen in the clinic, an attempt was made to tailor pain management and individualize care as much as possible.
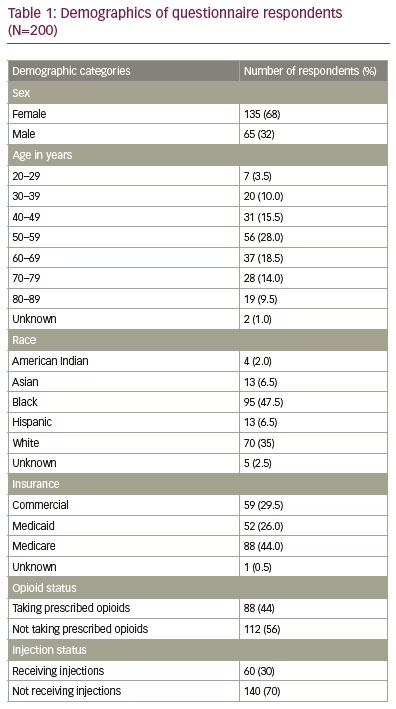
Once responses from 200 unique participants had been obtained, the study closed for recruitment and the responses were analysed. Our study yielded a diverse group of respondents according to sex, age, race and insurance status. More than half of the respondents had chronic back pain. Notable demographics were as follows: 70% of respondents had either Medicaid or Medicare as their primary insurance; 44% of respondents were on prescription opioids; and 30% had received injections. The remaining demographic details of the respondents are reported in Table 1.
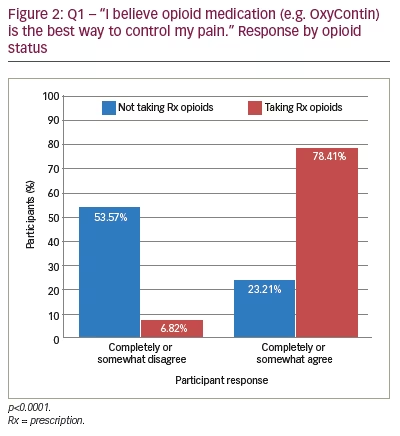
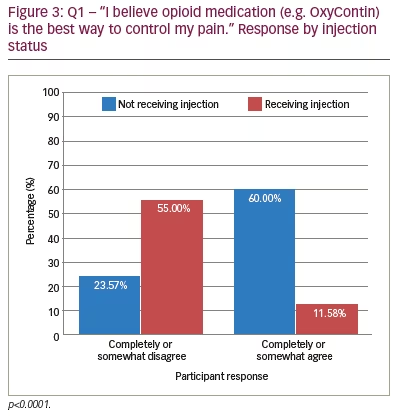
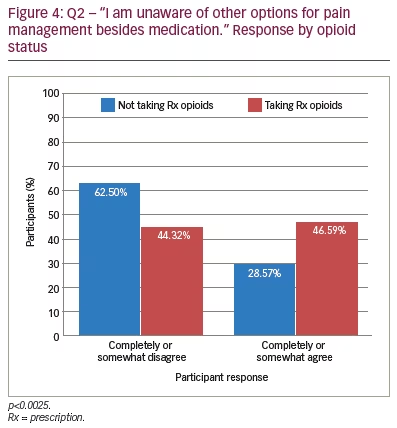
In responding to the first questionnaire item, most participants (47.50%) agreed that opioid medication was the best way to control pain (p<0.05), especially those taking prescribed opioids (78.41%; p<0.0001) (Figure 2). However, more than half (55.00%) of those who received injections for pain disagreed that opioids were the best way to control pain (p<0.0001) (Figure 3). With the second questionnaire item, most participants (54.5%) were aware of other options to control pain (p<0.05), but patients on opioids were significantly less aware of other options for pain control (p<0.05) (Figure 4). This trend continued in questionnaire item five, which addressed whether pain treatments other than medication cost too much. While the majority of participants agreed that non-prescription treatments for pain cost too much (54.27%), the majority of participants who received injections disagreed (p<0.0395).
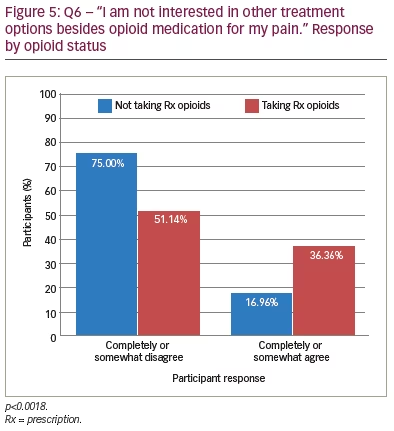
Questionnaire item six asked whether participants were interested in other treatment options besides opioids. The majority of participants reported they were interested in other treatments. However, participants taking opioids (36.7%) were significantly less likely to be interested in other treatment options besides opioids compared with non-opioid users (17%) (p<0.0018) (Figure 5). Finally, questionnaire item seven asked participants whether they believed treatments for pain, aside from opioid medication, were available to them. The majority of participants believed that treatments other than opioids were available to them; however, a significant percentage of male participants (54.00%) did not believe other treatments were available to them (p<0.0014). More than half of the patients with Medicaid as their primary insurance reported that other treatments besides opioids were unavailable (p<0.0437). Other potential barriers, including accessibility and time restraints to non-opioid treatments, were assessed, but these were not statistically significant.
Discussion
Increased awareness of the harmful effects of chronic opioid use has gradually led to more responsible opioid prescribing in the United States.1,4 Current guidelines support the use of chronic opioid therapy as part of a multimodal approach that addresses the biological, psychological and environmental factors that may contribute to chronic pain.14,15 Although research shows that long-term opioid therapy is largely ineffective for chronic non-cancer pain,1,2 it was unclear whether the patient population understood this to be true. We wondered whether certain subsets of our patient population differed in their beliefs on what they considered to be the optimal treatment for chronic pain. At our urban academic pain centre, more than half of our participating patients presented with chronic back pain. We found that most patients on chronic opioid treatment believed that opioids were the best option for the treatment of chronic pain. Interestingly, this opinion differed from that of patients receiving interventional pain procedures, such as injections for their back pain. In fact, patients who received injections were more likely to view interventional procedures as the best treatment for their chronic pain. We noted that accessibility or availability to multimodal treatments for chronic pain migth vary according to insurance carriers, and this may influence a patient’s exposure to other modalities for the treatment of chronic pain. We found that patients taking long-term prescribed opioids were significantly less aware of, or interested in, other non-opioid treatments and may view opioids as a superior treatment modality. Our preliminary research also shows that there may be a need for better patient education. Formal patient education programmes have been successful in improving outcomes in other chronic conditions such as diabetes and asthma.23 Despite considerable effort being made through public health campaigns to combat the opioid epidemic, there appears to be a continuing and concerning gap in knowledge on the use of opioids for chronic pain in some patients and providers.
Limitations
We recognize several limitations to this pilot study. First, this was a small prospective study conducted on 200 participants in a single institution; therefore, its findings may not have external validity and may not be generalizable to other institutions or clinic settings. Having said that, the patient population surveyed was not unlike many urban populations, as 1) patients come from varying psychosocial backgrounds and have varying third-party coverage, 2) most of the patients surveyed had chronic pain attributed to back pain or joint pain, and 3) many present with medical comorbidities such as obesity, diabetes and hypertension. Second, the patients’ responses to the questionnaire may be biased; patients in our clinic came from varying educational backgrounds, and this may potentially contribute to a bias in how patients respond to the questionnaire. Third, the fact that we did not limit the survey to a specific diagnosis may have confounded the results. Even though many patients surveyed suffered from chronic back pain, not all patients surveyed did, and there may be some patients for whom injections may not have been indicated (for instance, those suffering primarily from generalized pain).
Conclusions
Our findings suggest that exposure to alternative pain control modalities, as well as patient education, may play a significant role in patients’ beliefs and perceptions of what constitutes optimal pain control for their chronic pain. Inconsistencies in patient access to multimodal treatments for chronic pain with different insurance carriers may impact exposure to some of the multimodal interventions, such as injections.
We understand that pain itself is complex, let alone the issues surrounding the treatment of pain, and do not claim to have all the answers. We hope our findings will encourage further research to identify whether 1) standardized educational efforts, with a focus on the various strategies available for treating chronic pain, and 2) the use of these strategies, including non-pharmacological, interventional and behavioural therapies, may improve treatment goals and outcomes for the patient with chronic pain. If so, these efforts may potentially encourage some insurance carriers to provide better accessibility to multimodal treatments and, importantly, help reshape patients’ beliefs in the optimal treatment of chronic pain.