Post-herpetic neuralgia (PHN), a neuropathic pain disorder resulting from nerve fiber damage following herpes zoster (HZ) infection, is caused by reactivation of the varicella zoster virus (VZV).1–3 VZV reactivation leads to the symptom complex commonly known as shingles.4 PHN is defined as VZV-associated pain persisting for more than 3 months after resolution of a VZV infection.5 PHN symptoms often include allodynia, whereby normally innocuous stimuli, such as the light brushing of the skin, can elicit pain, paresthesia, and dysesthesia.6
The incidence of PHN increases with age.7,8 In population-based data from 1996 to 2005, out of 1,669 adult residents (≥22 years) of Olmsted County, MN, US, the proportion of individuals who developed PHN increased from 5 % in those aged <60 years to 10 % in those aged between 60 and 69 years, 17 % in those aged 70 to 79 years, and 20 % in individuals aged ≥80 years.8 Apart from age, other risk factors for PHN include severe acute pain related to the VZV infection, rash severity (>50 lesions), and the presence of a prodrome.9,10
Pharmacologic Treatments and Unmet Needs
Guidelines issued by the American Academy of Neurology,11 the International Association for the Study of Pain,12 and the European Federation of Neurological Societies13 categorize tricyclic antidepressants (TCAs), anticonvulsants such as gabapentin and pregabalin, and the lidocaine 5 % topical patch as first-line treatments for PHN. TCAs,14–16 gabapentin,17 pregabalin,18 and topical lidocaine19–21 have demonstrated efficacy in reducing the pain of PHN and have mostly acceptable tolerability profiles. In a recent systematic review and meta-analysis of 229 studies,22 the use of TCAs, serotonin-noradrenaline reuptake inhibitors, pregabalin, and gabapentin were strongly recommended.
The use of TCAs in treating PHN, however, is hampered by a slow onset of action and systemic adverse events such as urinary retention, weight gain, constipation, and sedation.23 TCAs have also been associated with cardiotoxic events, including myocardial infarction and cardiac dysthymias.23–26 Elderly patients appear particularly susceptible to these events.23 Adverse events associated with anticonvulsants likewise limit their use in some patients. The most common adverse events with gabapentin or pregabalin reported in clinical studies included somnolence, weight gain, and dizziness.27,28
Pathophysiologic Mechanisms Underlying Postherpetic Neuralgia
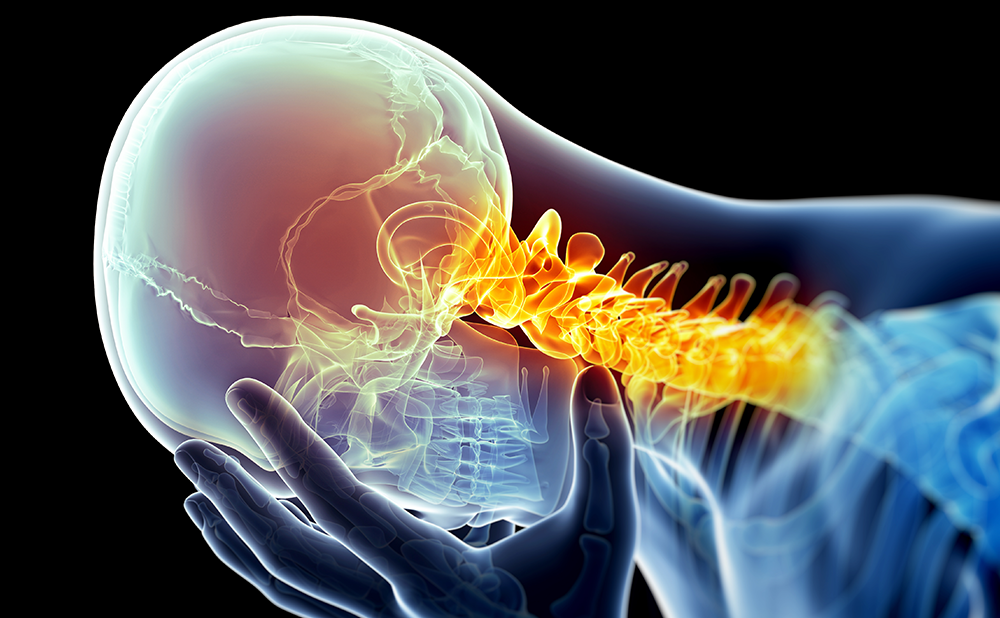
The pathophysiology of PHN, although not fully understood, is believed to be rooted in neuronal injury affecting both the peripheral and central nervous system (CNS).29 This injury leads to peripheral and central neurons generating spontaneous discharges while also lowering the activation threshold to cause pain with nonpainful stimuli (allodynia). At the cellular level, there is evidence to indicate that nerve fiber membrane receptors associated with pain, such as the transient receptor potential vanilloid 1 (TRPV1), are upregulated.30
Unique Mechanism of Action
The transient receptor potential (TRP) family of ion channels are selective for calcium and magnesium over sodium ions.31 TRPV1 channels are expressed in the CNS in areas that process pain signals.32 TRPV1, a member of the TRP family of ion channels, is a calcium-permeable channel, which is modulated by a diverse range of exogenous noxious stimuli including pH changes, high temperatures, and irritant and pungent compounds.33
The capsaicin 8 % w/w; 640 μg/cm2 patch (Qutenza®) is indicated in the US for the management of neuropathic pain associated with PHN.34 Capsaicin, 8-methy-N-vanillyl-6-nonenamide (see Figure 1),35 is the active ingredient in chili peppers that evokes burning and “flare and weal” responses and is a highly selective agonist for the TRPV1 receptor.31,36 TRPV1 receptors are found on a portion of primary sensory neurons with cell bodies in the dorsal root ganglion and are selectively expressed in the epidermis cutaneous nociceptors making them accessible to local treatment.36,37 In general, the TRPV1-expressing neurons are peptidergic, small diameter, and give rise to thin, unmyelinated C fibers,37–39 which may play an essential role in the chronic pain-induced plastic changes in the CNS.38 Natural stimuli such as tissue burns, noxious heat, and spider toxins can activate TRPV1 expressing C-fibers.31
Inactivation of voltage-gated sodium ion channels and direct pharmacologic desensitization of plasma membrane TRPV1 receptors may contribute to an immediate reduction in neuronal excitability and pain, while more persistent effects may be due to sustained increased levels of intracellular calcium.39 Such raised levels can activate calcium-dependent enzymes, such as proteases,40 which can induce depolymerisation of cytoskeletal components, including microtubules.41,42 Thus, multiple mechanisms are believed to be important for capsaicin-induced analgesia (see Figure 2). Capsaicin-induced local depletion of substance P is not thought to be crucial for capsaicin’s mechanism of action.43 Intra-epidermal nerve fibers degenerate following high-dose capsaicin application;44 these nerve fiber endings have been shown to recover after 24 weeks in healthy volunteers.45
Pharmacokinetic Profile
The capsaicin 8 % dermal patch measures 280 cm2 and contains 179 mg of capsaicin (640 μg/cm2).34 Capsaicin is extremely lipophilic, having little affinity for the aqueous blood phase and is readily absorbed into the epidermal and dermal layers. To determine systemic capsaicin exposure after single 60 or 90 minute applications, plasma samples were collected in 173 patients with PHN at varying intervals after patch removal (0, 1, 3, 6, and 24 hours).46 Overall, the majority of plasma concentrations of capsaicin were lower than 10 ng/ml; capsaicin plasma levels were found to decline rapidly, with a mean elimination half-life after patch removal of 1.64 hours. After a 60-minute application, the mean area under the plasma concentration time curve was 7.42 ng.h/ml and the maximum plasma concentration (Cmax) value was 1.86 ng/ml. The primary metabolites of capsaicin,47,48 hydroxycapsaicin, 17-hydroxycapsaicin, and 16,17-dehydrocapsaicin, as observed in in vitro hepatic and skin metabolism studies, were not detected in patients in this study.
Capsaicin is metabolized readily in the liver by various cytochrome P450 enzymes.49 During in vitro incubation with human skin, [14C]capsaicin was metabolized slowly over 20 hours.47 As only small quantities of drug reach the systemic circulation, there are no recommendations for dose adjustments in cases of hepatic or renal failure.50
Clinical Experience
The capsaicin 8 % patch clinical development program comprised phase I, II, and III studies and is summarized in Tables 1, 2, and 3,45,51–-59 respectively. For treatment of PHN, the capsaicin 8 % patch is applied for 60 minutes and then removed. In order to more fully blind patients in the trials, a lowconcentration capsaicin 0.04% patch was used as an active control; this dose was selected because it induced erythema and a sensation of heat. In one multicenter, randomized controlled trial (RCT), 42 % of PHN patients treated with the capsaicin 8 % patch reported a ≥30 % reduction in pain intensity compared with 32 % in the active control group (odds ratio [OR] 1.56, 95 % confidence interval [CI] 1.03 to 2.37; p=0.03; see Table 2).56 In this same study, the mean percent change in numerical pain rating scale (NPRS) score between baseline and weeks 2–12 was –29.9 % in the capsaicin 8 % patch group versus –20.4 % in the active control group. In another multicenter RCT in PHN, the mean percent change in NPRS score between baseline and weeks 2–8 was –32.0 % in the capsaicin 8 % patch group versus –24.4 % in the active control group (p=0.011).58 In the same study, a ≥30 % reduction in NPRS score was achieved in 46 % of capsaicin 8 % patch-treated patients compared with 34% of active controls (p=0.02; see Table 3).58
A meta-analysis that included seven RCTs of similar design investigated the capsaicin 8 % patch (1,120 with PHN; 338 with HIV-associated neuropathy [AN]).60 This meta-analysis was based on pooled individual patient data, for identical end-points, as if all patients were part of one large study. The percent change from baseline to weeks 2–12 was –30.7 % in the capsaicin 8 % patch and –22.7 % in the control group, which yielded a group difference of 8.0 % (95 % CI 4.6, 11.5) (p<0.001); the proportion of patients achieving a 30 % reduction in pain intensity was 44 % for the capsaicin 8 % patch-treated patients compared with 34 % for control-treated patients.60 In a separate meta-analysis of combined individual patient data (1,313 participants with PHN) from seven doubleblind RCTs,61 44 % of patients had a ≥ 30 % reduction in pain intensity, and 11 % of patients achieved complete pain relief 2–12 weeks after capsaicin 8 % patch treatment. In those responding to treatment, analgesia started within a few days of treatment and was sustained for an average of 5 months. In a Cochrane review62 of six studies involving 1,272 participants with PHN and 801 with HIV-AN, it was concluded that capsaicin 8 % patch treatment generated greater levels of pain relief than the active control in both PHN and HIV-AN. Point estimates of the numbers needed to treat were 8.8 (95 % CI 5.3–26) at 8 weeks and 7.0 (95 % CI 4.6–15) at 12 weeks.
The Qutenza Safety and Effectiveness in Peripheral neuropathic Pain (QUEPP) study evaluated 1,044 patients without diabetes with peripheral neuropathic pain, who received a single application of the capsaicin 8 % patch.63, 64 PHN was the most frequent diagnosis (31.9 %) followed by postsurgical neuralgia (22.8 %), post-traumatic neuropathy (12.4 %), polyneuropathy (14.3 %), and mixed pain syndromes (16.6 %). Mean relative pain intensity during weeks 1–12 decreased by 24.7 % (1.1 standard error of the mean [SEM]) and significant improvements in pain attacks (p≤0.001), sleep duration (p≤0.001), and sleep quality (p≤0.001) were reported in the peripheral neuropathic pain patients. The ≥30 % responder rate was 42.7 % and the ≥50 % responder rate was 23.7 %. The use of opioids and anti-convulsants decreased significantly (p<0.001) in capsaicin 8 % patchtreated patients. In the QUEPP study, 146 adverse drug reactions were reported in 106 of 1,063 patients of the safety population (10.0 %); the most common among these were application site reactions, such as erythema and pain.63 In total, 27 serious adverse event (SAE) drug reactions were reported in 17 patients (1.6 %) and five SAEs resulted in death, none of which were treatment-related.64 The highest treatment response, relative change of numeric pain rating score on days 7–14 to week 12 compared with baseline, was seen in patients with a history of pre-existing peripheral neuropathic pain of <6 months, suggesting that early initiation of treatment may be advantageous.62 In patients with pre-existing peripheral neuropathic pain for <6 months, the mean relative change of the NPRS score on days 7–14 to week 12 versus baseline was −36.6 % (4.6 SEM; n=105).
Longitudinal analysis from four double-blind RCTs of the topical capsaicin 8 % patch has suggested that there are different response groups to treatment, which may be related to different pain mechanisms despite a presumed common underlying disease process.65 In this analysis, five distinct response subgroups were detected from data of 1,248 patients treated with the capsaicin 8 % patch, including a group of nonresponders, a group with partial response, and a group exhibiting full analgesic effect.
Overall, the clinical studies showed the capsaicin 8 % patch to be generally safe and well-tolerated (see Tables 1–3). The most commonly reported side effects were dermal irritation, erythema, and pain at the site of application. These effects were transient and mild to moderate in severity. This was emphasized by an integrated analysis of tolerability data from the capsaicin 8 % patch clinical program, including 1,696 patients with peripheral neuropathic pain related to PHN, HIV-AN, and painful diabetic neuropathy. Almost all (≥98 %) of the patients completed ≥90 % of the full treatment duration, regardless of the number of treatments given.66 NPRS score increases returned, on average, to baseline within 85 minutes following treatment.60 Transient patch application-related pain with the capsaicin 8 % patch was managed with local cooling or oral analgesics in nearly all cases. This indicated that patch application-related pain was not a barrier to use.
Role of Lidocaine Pre-treatment
To mitigate any discomfort, prior to treatment with the capsaicin 8 % patch, the product prescribing information states that patients should be pretreated with topical anesthetic cream, such as lidocaine, for 60 minutes.35 Lidocaine reduces pain transmission through inhibition of sodium ion channels; sodium channels act independently of the TRPV1 receptors.67 Capsaicin can induce axonal depolarization and dysfunction even in the presence of sodium channel blockade.68 There are potential advantages in avoiding pre-treating patients with topical lidocaine including a reduction in total treatment time and a potential cost benefit. This was supported by a comparison of 32 pre-treated patients with 26 non-pre-treated patients receiving capsaicin 8 % patch treatment in which there was no significant difference in mean NPRS at any time during or after capsaicin patch treatment.67 Furthermore, the same proportions (57 %) of pre-treated and non-pre-treated patients were willing to receive capsaicin re-treatment. Topical lidocaine-induced analgesia itself is transient (lasting 1–2 hours); statistically significant pain relief compared with the vehicle patch was not achieved in clinical trials until 4 hours post-application.69 This suggests that 60-minute pre-treatment does not allow sufficient time for topical lidocaine to act on the nerve endings. Further study is therefore warranted to explore whether lidocaine pre-treatment confers any overall benefit in the application of the capsaicin 8 % patch.
Repeat Application of the 8 % Capsaicin Patch
The effects of repeated 8 % capsaicin patch treatment were shown in an open label extension of a PHN trial.52 Fifteen patients who received at least two treatments had similar reductions in their pain score from baseline, 28.4 % after the first treatment; 29.7 % after the second treatment. Nine patients who received three treatments achieved a mean reduction from baseline in NPRS score of 34.1 ± 24.2 (95 % CI 52.7–15.6). These results demonstrated that a mean decrease of approximately 30 % was maintained during each treatment cycle of the capsaicin 8 % patch regardless of the number of treatments received.
Cost-effectiveness
A review of high-concentration topical capsaicin for the treatment of chronic neuropathic pain highlighted that although the treatment is similar to other available therapies in terms of efficacy, it is likely to be used when other available therapies have failed owing to reasons of cost.62 However, in a cost-effectiveness analysis using a 1-year Markov model that compared the 8% capsaicin patch to existing PHN therapies, measures showed that 8% capsaicin and topical lidocaine patches had significantly higher rates of effectiveness than oral agents.70 The analysis also found that the 8 % capsaicin patch was comparable to the topical lidocaine patch and within an accepted cost per quality-adjusted life-year gained threshold compared with the oral treatments.
Concluding Remarks
Initially the topical administration of capsaicin, a highly selective agonist for TRPV1, resulted in localized burning sensations, hyperalgesia, allodynia, and erythema.36 Over time, TRPV1-expressing cutaneous nociceptors become less sensitive to a variety of stimuli, including capsaicin itself, and exhibit a protracted decrease in spontaneous and evoked firing known as defunctionalization.36,43 Capsaicin-induced defunctionalization of cutaneous nociceptors results in a reversible retraction of epidermal nerve fibers while leaving the majority of the neuron and cell body in the dorsal root ganglion unaffected.71–73
At present, it is unclear why only a proportion of patients respond to capsaicin treatment and how response to treatment may be predicted. Questions also persist as to whether lidocaine pre-treatment is beneficial, how deep the capsaicin from the capsaicin 8 % patch penetrates the skin layers, and how much capsaicin reaches the nociceptors.
Overall, the clinical evidence indicates that the capsaicin 8 % patch has a good safety and tolerability profile and offers effective topical therapy in PHN. The episodic treatment application of every 3 months or longer makes the capsaicin 8 % patch a convenient option for patients. The capsaicin 8 % patch is therefore a valuable addition to the armamentarium of analgesic options for PHN.