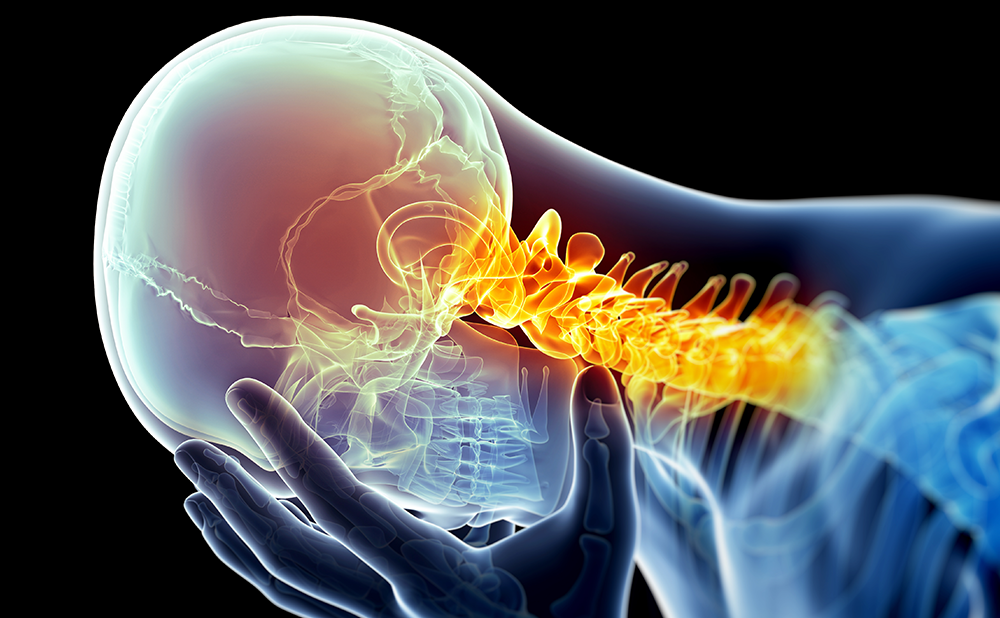
Chronic pain is a widespread, debilitating condition shared by millions worldwide. In 2015, more than 25 million Americans reported suffering from consistent daily pain.1 The Center for Disease Control (CDC) reported 15.6% of American adults experience consistent headaches or migraines, 29% have consistent low back pain, and 14.9% suffer consistent neck pain. With pain conditions accounting for approximately 80% of doctor visits, effective pain management and prevention methods are essential to use in order to effectively deal with issues such as emotional distress, loss of workproductivity, and quality of life in these patients.2 The US spends roughly $625 billion annually for medical treatment and lost productivity related to the pain conditions.2,3
The prevalence of chronic pain stimulated the US Congress to designate that the 2000s would be the decade of pain control and research,3 by passing “The 2010 Patient Protections and Affordable Care Act.” Moreover, the National Institutes of Health (NIH) supported the Department of Health and Human Services (HHS), in collaboration with the Institute of Medicine (IOM), highlighted the importance to examine pain as a public health issue.2 The IOM’s role was to assess the state of science regarding education, care, and research of pain, to make recommendations about how to proceed forward in the best interest of the public. The IOM presented their findings and recommendations in the US in a publication entitled “Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research”.4 The IOM recommendations were: to shift the view of pain from a patient perspective to one of a major public health issue; increase awareness of the problem of pain; focus on the prevention of pain; improve pain assessment techniques; address disparities among sufferers; and foster both treatment centers and cohesive research among scientists and healthcare providers. Interdisciplinary research is essential to better understanding complex, multifaceted issues of pain in order to address these recommendations.5
Individuals experience pain in a multitude of ways, often seeming subjective to the individual based on their perceptions and descriptions of their condition. The variations in how patients perceive and relay this information can influence physician interpretation and treatment strategies. Unfortunately, difficulties in assessing and treating pain have led to an enormous proportion of sufferers to be treated with opioid medications, which manage pain but do not resolve the condition. Opioids tend to be highly addictive, and are often misused. In 2014, The National Institute on Drug Abuse (NIDA) estimated 26–36 million people would abuse opioids globally in the next year.6 Opioid medications cause changes in brain chemistry that can lead to mood and behavioral issues and disrupt physiological functions.7 Treatment models focusing on prevention and early intervention may help decrease the number of patients who require long-term use of opioids. Of course, it is often difficult to establish effective generic pain management programs because every individual displays a unique combination of biopsychosocial factors.3 This is the major reason why the biopsychosocial model, out of which grew interdisciplinary pain management, has been so successful. Additionally, programs that emphasize early intervention and functional rehabilitation components have been shown to be highly effective and financially sensible.3 Reliable conceptual models to gauge individual differences, and then treat them accordingly, are vital to successful pain management.
Conceptualizing chronic pain — an overview
Chronic pain is characterized by persistent symptoms, often unrelenting and debilitating in nature. The definition of pain encompasses unpleasant experiences, both physical and emotional, with actual or potential tissue damage and the chronicity is implied that the pain persists over time.8,9 Where some conditions are acute, and the pain dissipates once the problem is addressed, chronic conditions require ongoing monitoring, treatment, and often require a variety of strategies to manage them. Pain management techniques have been evolving over the course of history; a few notable practices based on such techniques include the Ancient Greeks’ humoral theory, the religious and spiritual ideations of the Middle Ages, and scientific advancements occurring during the Renaissance.10 The resulting theories relied heavily on biological explanations of pain, and incorporated illness, disease, and eventually the individual circumstances and states of the patient.
The biomedical model
The biomedical model explains illness based on somatic processes within the body. This view often assumes that psychological and social processes are largely irrelevant to biological illnesses and focuses instead on mainly biochemical imbalances and neurophysiological abnormalities. However, over the years, even with the ever-increasing number of sophisticated diagnostic and therapeutic procedures (e.g., medical imaging, and interventional/surgical techniques), there has been no solid, objective validation of their effectiveness concerning chronic low back pain.11 Moreover, this promoted unrealistic “high expectations” on the part of patients that this new medical technology would “cure” their pain. Unfortunately, this is not always the case as many chronic conditions require lifelong maintenance (as explained by Gatchel 200512).
The rise of psychosomatic medicine somewhat curbed this strictly biological view and uncovered the important connections between biological and psychosocial factors. Landmark studies started to appear in the scientific literature, such as: Selye 1950,13 who examined the link between homeostasis breakdown and stress; Rosenman and colleagues,14 who examined the link between Type-A behavior and coronary heart disease; and Birk,15 who applied biofeedback techniques to conditions such as headaches. Such studies were crucial in amassing support to move from a strictly biomedical model. Psychodynamically oriented professionals also began to emphasize the role of psychological factors such as personality, attitude, and resilience in illness.16 However, this psychodynamic model remained limited in scope, due to the unstructured, subjective nature of it. The aforementioned shortcomings of methodology and limited range and scope of explanation, coupled with significant advances in neuroscience, and increased attention to eastern medicine practices, “opened the door” for a shift to a better model.
The biopsychosocial model
The biopsychosocial model evaluates the integrated “whole person,” with both the mind and the body together as interconnected entities, recognizing biological, psychological, and social components of pain and illness. Prior to the major research of the biopsychosocial model in the 70s and 80s, pain was generally viewed as an organic process. If pain was not organic, patients were referred for psychiatric care to treat the pain, which was deemed “psychogenic” in nature. The biopsychosocial model also emphasizes illness and how you live with, or respond to, symptoms or a disease, in contrast to the biomedical disease model, which primarily focuses on disruption of bodily systems by underlying physiological, anatomical, or pathological processes. Basically, the biopsychosocial model takes into account the dynamic interactions among bio, psycho and social factors in the pain-experience process.5,8 However, in order to continue to provide effective pain management approaches, the model must adapt as our knowledge and technology advances. Some criticize the biopsychosocial model pointing out that we now expect behavior to be rooted in biological and psychological components, realizing a systemic approach as opposed to the interactions made among these three factors the model historically suggests.17 Expanding the basis for a holistic approach to pain management is necessary, particularly when discussing the need for interdisciplinary assessment and treatment of chronic conditions. There are also often individual differences in the nature of these interactions, which account for the unique symptom patterns presented by specific patients. This creates the need to tailor interdisciplinary pain management programs for each specific patient during the assessment-treatment process.
George Engel’s conceptual model of illness suggested a progression of pain stemming from a physical problem, to distress, then illness behavior, and finally adoption of a sick role (Figure 1) thus incorporating bio, psycho, and social components.18 Engel studied patients with medical disorders, finding that biological measures alone did not provide a comprehensive view of the patients’ pain and treatment, and needed to consider psychological, social, and cultural factors to accurately assess and manage illness conditions.3 Engel felt previous pain theory had overlooked the critical interaction of multiple factors and sought to develop his own to address the gaps not addressed by biomedical models.18 Loeser proposed a direct model of pain in which a physiological component (nociceptors), as the beginning of the pain progression, as seen in Figure 1.19 According to Loeser’s theory, nociceptors are sensory nerve cells that respond to damage within the body through a process called nociception. The stimulation of the nociceptors leads to a sensory component (i.e., experiencing physical pain). This process results in affective components, suffering, and exhibition of pain behaviors. Pain behaviors are acts used to communicate feelings associated with the pain experience. Suffering refers mainly to the emotional distress caused by pain. These emotions typically manifest internally, and are often highly unpleasant. Though central components of Loeser’s model are no longer accepted, his model is often discussed as an important historical concept that helped develop our current understanding of pain conditions.
Melzack and Wall’s Gate Control Theory of Pain was the initial basis for our current modern understanding of pain physiology.20 This theory aimed at a more comprehensive explanation of pain by melding

specificity theories with affective views and pattern-response theories.5 The Gate Control Theory, presented in a series of stages, proposed the dorsal horn of the spinal cord acted as a gate that modulated sensory transmissions controlled by pain and touch fibers before reaching higherlevel brain areas for perception.16 Building from the Gate Control Theory, the Neuromatrix Theory of Pain (originally proposed by Melzack and Casey21), describes a network involving motivational-affective, cognitiveevaluative, and sensory-discriminative functions. The combinations of these components gauge bodily responses to stress. This neural network, called the body-self neuromatrix, suggests that processing of pain is widely distributed throughout the neuromatrix, and the experience of pain results from such output.22
Though the strictly biopsychosocial model may not be the most exhaustive tool available today, these theories have been critical in the advancement of tailored pain management approaches. Additionally, arguments of reliability around the model, specifically to make the perspective more scientific while still allowing a great level of customization, propose ideas like patient-centered interviewing in which the process can repeat a reliable methodology and systematic questioning process that centers around the individual, focusing on their specific answers to the same set of inquiries.23 Criticisms such as these are necessary to help push our understanding toward the most holistic views available, and in doing so allow for effective interdisciplinary treatment strategies and patient centered care. Building on our knowledge of how the bio, psycho, and social factors interact and working in issues of genetic predispositions, cultural ideologies, stress, deconditioning variables, and available tools could continue to expand the tailoring of effective pain management and allow for the best possible outcomes for sufferers.
In general, the Diathesis-Stress Model examines gene-environment interactions and the resulting behavior, and suggested that a genetic predisposition (diathesis) interacts with environmental factors (stress) to produce a set of behavioral outcomes.24 In the context of pain, our behavioral outcomes represent pain behaviors and the predisposition of developing a chronic pain condition.25 Genetic vulnerabilities to develop a specific illness or injury, exacerbated by stress (particularly stress resulting from the injury), combine to produce a chronic pain condition with physical, psychological, and social suffering.25 The Biopsychosocial Model accounts for the resulting effects of pain conditions, but the addition of a diatheses-stress component (to be reviewed next) may be especially helpful in the determination of why some people develop a chronic pain condition while others do not.
Biopsychosocial-diathesis stress model of chronic pain
In order to even better treat and manage chronic pain conditions, it may be important to expand the biopsychosocial model to incorporate a diathesis-stress component. This would allow for a deeper understanding of how the biological, psychological, and social factors are acting together, while also considering the predispositional vulnerabilities of the patient.12 Chronic pain conditions produce stress, and Levi proposed such stressors likely exacerbate the pain disorder.24 Together with genetic factors, known stressors (such as physical and sociocultural vulnerabilities) can have a profound effect on chronic pain sufferers, making the condition even more excruciating and difficult to manage. These are reviewed next.
Genetic vulnerabilities
Epigenetic research has begun to illuminate how the expression of candidate genes that contain certain predispositions for illness, and their resulting behavioral phenotypes, are displayed.26,27 Candidate polymorphisms associated with chronic pain include HTR2C; Catechol-OMethyltrans- Ferase (COMT); Interleukin 6 (IL6); Interleukin 1 β (IL1B); and μ-opioid receptors (OPRM1).28,29 In addition to these genetic predispositions, variables such as stress can alter their phenotypic behavioral expression, and have lasting effects both behaviorallyand psychosocially.2,29,30
Biological vulnerabilities and physical deconditioning
Individuals may have biological predispositions to injury and physical deconditioning problems. The breakdown in normal physical functioning due to pain, from fear-avoidance, kinesiophobia, pain catastrophizing, etc., can be mild to severe and have lasting repercussions on healthy functioning in biological, psychological, and social areas. In the longterm, disruption of homeostatic states can lead to increased stress levels and have harsh consequences to the body.5 Indeed, chronic pain is a stressor with a wide range of biopsychosocial effects.5 Cortisol release is an important and necessary function for stress adaption, but extended secretions can be detrimental. Increased and continuous activation of the hypothalamic-pituitary-adrenal (HPA) axis can lead to breakdowns of muscles, bone, and tissue which results in more pain and the continuation of a vicious cycle.31 Furthermore, serotonin and norepinephrine are involved in the pain cascade, but also implicated as pathogenic mechanisms for mood disorders.5 Modulation of these biochemical components through the endocrine system is required for proper function and processes to maintain homeostasis.12
Moreover, concepts such as neuroplasticity and central sensitization are central to physical deconditioning. Neuroplasticity is the brain’s ability to change based on personal experience, modifications in behavior, environment, or injury. Central sensitization occurs when the nervous system is consistently in a highly reactive state, and is associated with development and maintenance of chronic pain conditions.32 Pain sensations can become distorted as a result, meaning the receptor thresholds are decreased, or more sensitive to, noxious stimuli.33 Distortions of pain resulting from central sensitization clearly affect the individual pain experience through pain hypersensitivity, hyperalgesia, aftersensations, and allodynia.32 Both concepts canlead to avoidance behaviors and fear, resulting in further physical and mental deconditioning.
Psychological vulnerabilities and mental deconditioning
The development or exacerbation of psychological issues resulting from initial distress following injury can lead to physical deconditioning, as well as mental deconditioning as reflected in indices such as learned helplessness, anxiety disorders, personality disorders, substance abuse, and depression, as seen in Figure 2.31 Evaluating psychosocial factors, as pain conditions worsen or become chronic, becomes increasingly important when considering the crucial role these factors play in the acceptance, maintenance, and suffering of the individual.34
Emotional effects of pain can include behaviors such as catastrophizing, fear-avoidance, re-evaluation of beliefs, issues of efficacy and control, vulnerability, and resilience. While these behaviors can be present independent of pain, the process often exacerbates them. Catastrophizing and avoidance behaviors tend to be a result of anticipated pain when patients feel that a wrong movement or activity could result in, or worsen, their pain.5 There may be individual differences regarding patients’ selfcontrol and self-efficacy. It may be that those who feel they have more control over the pain duration or intensity would display decreased levels of learned helplessness and similar behaviors, relative to those who feel they are without control concerning their pain condition. However, this aspect has not been unequivocally determined in the extant research literature. Overall, individual experiences, temperament, and personality all have influences on these behaviors.5
Social vulnerabilities
There are inequalities in socioeconomic status (SES) and cultural beliefs concerning pain management. Often, low SES Americans do not have access to quality healthcare, and are unable to afford health insurance, prescriptions, or care without coverage, nor can they travel away from home to gain access to quality care in areas that are underserved and/ or overpriced.35 In addition to the financial difficulties, cultural traditions may hinder some from seeking or accepting care. For instance, some Asian cultures foster a stoicism in the presence of pain that can make it difficult for medical providers to evaluate.36 Stoicism and fear often transcend cultural boundaries, as males may be less likely to seek treatment in some cultures due to their respective gender norms. Furthermore, minority groups may face prejudice and a decreased level of care in certain areas, or from particular providers, based on the medical professionals’ own beliefs, cultural expectations, or prejudices.
Summary
Thus, to summarize, the Biopsychosocial-Diathesis Stress Model of Chronic Pain takes into account how certain diatheses or predispositions can affect the resultant configuration of the biopsychosocial components of chronic pain that will need to be comprehensively assessed and treated. Figure 3 provides a brief overview of the various constructs we have discussed, as well as the number of feedback loops involved in the final configuration of the biopsychosocial assessment-intervention model that will need to be individually tailored for each patient with chronic pain. In a sense, this is in keeping with the new goals of Precision Medicine, which focuses on better treatment of patients by developing a large biobank of patient genomic profiles, as well as data on diet, lifestyle, and occupational variables.37 One important outcome will be to advance pharmacogenetics in order to evaluate the “right drug for the right patient at the right dose.” This “precision” is what drives the interdisciplinary assessment and pain management process.

Clinical risk assessment and intervention study findings
The assessment before treatment is clinically relevant to treatment outcomes, identifying patients who may benefit from a primary care or multidisciplinary approach and those who would be better served by an interdisciplinary approach. Rothman and colleagues (2013) found that patients with chronic muscular pain who received a multimodal pretreatment assessment had significant improvements in quality of life and working ability and higher satisfaction than those who received a routine multidisciplinary assessment.38
An interdisciplinary approach integrates disciplines into a cohesive team responsible for all aspects of treatment rather than each discipline separately approaching treatment from their own perspective (i.e., a multidisciplinary approach). Functional restoration (FR) is an interdisciplinary management approach based on the biopsychosocial model that is applied to the treatment of chronic musculoskeletal disorders. The treatment team usually consists of a physician, specialized nurse, physical therapist, and clinical psychologist. Other providers, such as an occupational therapist, may also be included in the treatment team. The entire treatment team meets with the patient at the same time, providing consistent advice and directives. While traditional treatment planning is focused on subjective physician observation and patient self-report, FR emphasizes objective assessment of all aspects of functioning. A central tenet of FR is the quantification of function, that is, the systematic assessment of function to determine improvement. This makes treatment monitoring of otherwise unobservable variables more possible.39
We will now turn to another important area of biopsychosocial assessment and treatment with two examples of a series of studies. Chronic low back pain and temporomandibular joint and muscle disorder (TMJMD) are two of the most prevalent chronic musculoskeletal pain conditions.40

We will review early risk-assessment and intervention for these two conditions below. Acutely, low back pain affects one in four adults, with 10–15% developing chronic conditions.3 As mentioned previously, the costs associated with chronic pain conditions are estimated to be in the billions of dollars annually.
Low back pain
A preliminary study by Gatchel, Polatin and Mayer sought to develop reliable early detection techniques for “high risk” acute low back pain (ALBP) patients.9 This NIH-supported study examined over 500 ALBP patients from an occupational medicine clinic who were administered a comprehensive biopsychosocial evaluation within 6 weeks of injury. Participants were followed for 1 year, at the end of which approximately 20% did not return-to-work. Using a statistical algorithm developed from a receiver-operator curve (ROC) analysis and estimated probabilities from a logistic regression model; they were able to differentiate “low-risk” versus “high-risk” patients for developing chronicity, with an accuracy rate of 89.2%.9
Subsequently, another NIH-funded study screened a large cohort of ALBP patients to determine their risk status, using the algorithm developed in the above preliminary project.41 High-risk patients were randomly assigned to receive a usual course of treatment of their choice, or an early intervention FR program. Follow-up evaluations were conducted at 3-month intervals over the next year in order to assess socioeconomic factors such as healthcare utilization, medication use, whether patients had returned to work, as well as self-reported pain and disability. Results revealed that patients who received the early FR intervention displayed significant reductions in medication use, pain and disability reports, healthcare utilization, and were 4.55 times more likely to have returned to work. Those in the usual treatment condition displayed more symptoms of chronic pain and disability, relative to the low-risk patients. In addition to the obvious physical benefits of the FR intervention, there were significant financial advantages at the 1-year period: the FR program cost was one-half of the usual treatment cost.41
Finally, a third NIH-supported effectiveness study was conducted to compare an early FR intervention program; a workplace-transition program; and a combined approach of both FR and workplace transition. Results indicated that both approaches containing the FR intervention were most effective in positive patient treatment outcomes. Once again, the cost effectiveness of the FR intervention was also noted among patients.42
Temporomandibular joint and muscle disorder
TMJMD ranks second among all musculoskeletal disorders in the United States in prevalence, with an estimated $4 billion dollars in annual costs.40 Again, similar to the above reviewed research on low back pain, a series of NIH-supported studies for early identification and intervention for patients at high-risk of developing TMJMD were conducted. Initially, Epker, Gatchel, and Ellis used a logistic regression model to formulate a statistical algorithm to identify high-risk patients.43 The algorithm used components of the Diagnostic Criteria for Temporomandibular Disorder, and successfully identified patients (at a 91% accuracy rate) into high-risk versus low-risk groups for developing chronic TMJMD problems. Subsequently, Gatchel, Stowell, and Buschang conducted an investigation to determine if an early biobehavioral intervention for high-risk patients would result in decreased levels of pain 1 year post-treatment, as compared to those not receiving early intervention.44 Significant differences were found between the groups, supporting the premise that early intervention is critical in TMJMD pain management, and the prevention of more costly chronic problems. Additionally, significantly larger overall costs were connected with the non-intervention group, relative to the intervention group, when examined throughout the duration of the study.45
Finally, a third study sought to examine TMJMD patients in chronic and acute stages, in addition to high-risk and low-risk categories. High-risk patients were randomly assigned to a self-care group or an early biopsychosocial intervention. The self-care group focused on education to understand prevention and pain reduction strategies. The intervention group included cognitive behavioral coping skills, progressive muscle relaxation, riskreduction, and biofeedback training. Patients were evaluated at baseline, 6 months, 12 months, and 24 months. Results demonstrated significant decreases in pain and disability, in the early intervention group.46 Both high-risk groups improved significantly from baseline through the 2-year follow up. The intervention group also reported significantly faster recovery compared to the self-care group.
Summary and conclusions
The advent of the biopsychosocial model has been responsible for developing the most comprehensive basis for treating chronic pain – an interdisciplinary multifaceted pain management strategy.5,47 Pain is a distinctive experience, with a wide range of influential factors in its progression. Predispositions for injury and illness, social influences, economic difficulties, psychological factors, and physiology all play important roles in the development and management of chronic pain.5 In addition to pain, patients often experience functional deficits including physical difficulties, psychological and emotional distress, poor coping skills, and kinesiophobia. Interdisciplinary pain management programs have shown to be highly effective in management and cost.5,47 FR or other similar programs require careful assessment of individuals to provide better pain management outcomes.34 Incorporation of early interventions, based on the biopsychosocial model, appear to be the most effective pain management strategies available, allowing for further customization for individual needs.
Further, it is important to consider and develop reliable risk prediction for patients who experience acute pain and may transition to a chronic pain condition. A strategy that is highly effective in prediction could help alleviate pain, suffering, and costs to pain patients, potentially saving treatment and resources the patient doesn’t need.48 The Prognosis Research Strategy group (PROGRESS) proposes that risk models must be clinically useful (e.g. easy to use), reliable, and customizable to individual needs and circumstances.48 Early intervention programs have reduced costs and suffering but more research is needed to develop tools to effectively target those at risk for developing chronic pain conditions and providing a solid base for their identification while still allowing the flexibility of tailored assessment.46 Excessive treatment could result in unnecessary costs, potential suffering, depletion of resources, and distrust between patients and providers.49
Advancements in neuroscience, epigenetics, and pain research, including cognitive, biological, psychological, genetic perspectives, have now allowed for a better understanding of cellular and behavioral mechanisms.3 Still, more research is needed to address gaps in knowledge and continue to develop the most effective strategies possible to help address and alleviate pain. Challenges of translating research into practice, funding, regulatory processes, and ever-evolving patient needs necessitate the support of pain research moving forward.3