Treatment guidelines recommend preventive therapy for migraine, based primarily on the frequency of migraine attacks.1 Migraine-related burden of disease increases with the number of headache days; however, even fewer than 4 headache days per month can result in severe disability in addition to impairment during individual episodes.2,3 The needs of patients with migraine go beyond simply reducing migraine frequency; healthcare practitioners should also consider duration, severity and resulting disability of attacks as crucial factors.2,4 Additionally, treatment needs may also fluctuate within the same patient, as they cycle between episodic and chronic migraine during the reproductive versus non-reproductive years, and in more stressful environments.4–6 Personalizing treatment decisions on a case-by-case and temporal basis provides a patient-centred model of care. This article summarizes three symposium presentations on current and emerging preventive treatments for migraine with additional case studies.
Overview of migraine and the preventive treatment landscape
Burden of migraine
Migraine affects approximately 37–39 million Americans,7,8 approximately 28 million of whom are women.9 It is a leading cause of disability,10,11 accounting for an estimated 157 million lost work days and up to $36 billion annually in lost productivity and healthcare costs in the USA.7 Furthermore, migraine has a profound impact on daily living and is a cause of social stigma.12,13
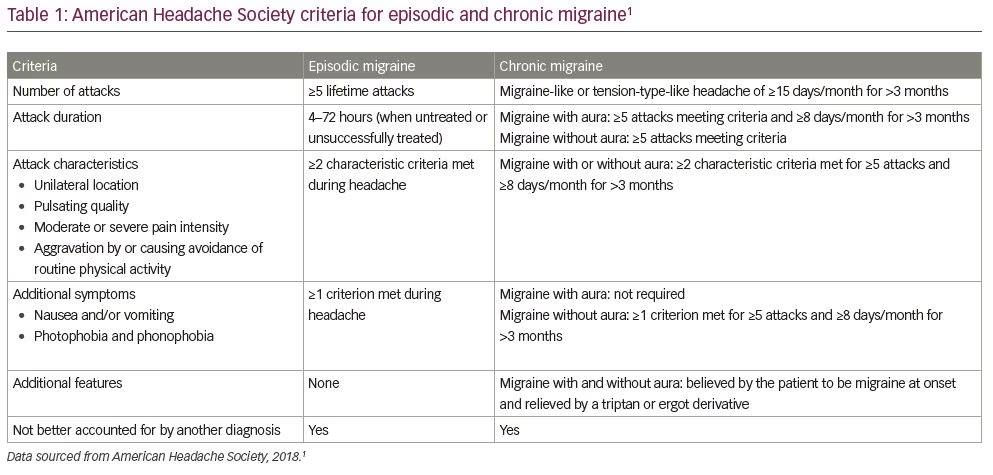
Migraine can be classified as either episodic or chronic, based on the frequency of headache and migraine days experienced per month.1,14 Episodic migraine is delineated as ≤14 headache or migraine days per month, whereas chronic migraine is defined by the International Classification of Headache Disorders (ICHD)-3 as ≥15 headache days per month for a period longer than 3 months, with ≥8 of these being migraine days.1,14 For all diagnoses of migraine, ≥5 lifetime attacks are needed to fulfil the ICHD-3 diagnostic criteria for migraine without aura, including a duration of headache of 4–72 hours if untreated or unsuccessfully treated, and further criteria as listed in Table 1.1,14 Over a lifetime many patients fluctuate between episodic and chronic migraine, and an estimated 2–3% of patients with episodic migraine progress to chronic migraine annually, with a higher proportion (14%) reported for patients in specialist clinics.15–17 Additionally, acute treatment overuse may lead to the development of chronic migraine.15
Current preventive therapeutics
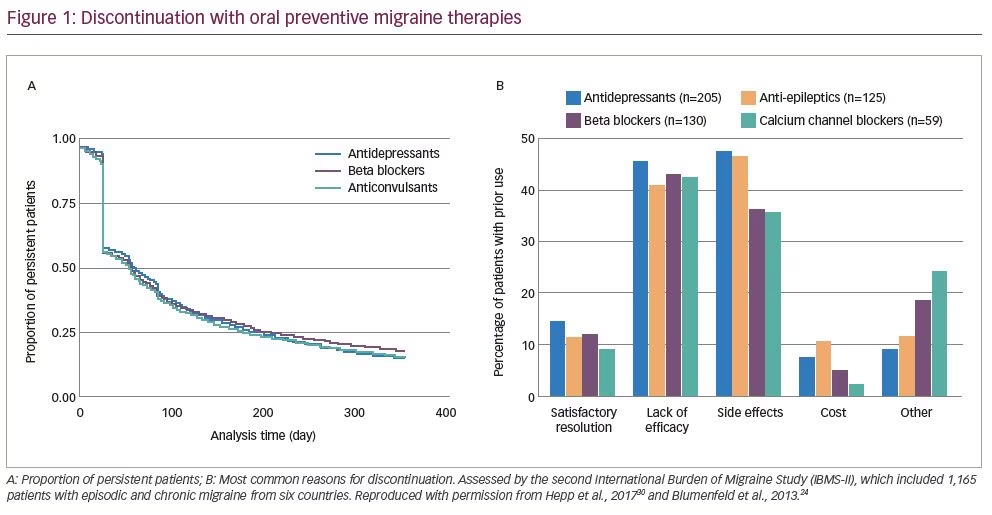
Migraine preventive treatments that are currently recommended by the American Headache Society (AHS) for chronic migraine include oral antiepileptic drugs, β-blockers and antidepressants, and injectable therapies such as onabotulinumtoxinA and subcutaneously injected calcitonin gene-related peptide (CGRP) inhibitor monoclonal antibodies (mAbs) including erenumab, fremanezumab and galcanezumab.1 The development of mAbs targeting the CGRP pathway was stimulated by research identifying CGRP receptors at proposed sites of migraine pathogenesis and that CGRP levels are increased during migraine attacks and normalized after treatment.18,19 More recently, the CGRP inhibitor mAb, eptinezumab, administered intravenously, has been approved in the USA and offers 100% bioavailability with a rapid onset of action and sustained benefit over 3 months.20–23 Despite this range of therapies, it is estimated that only 28–52% and 45–96% of eligible patients with episodic and chronic migraine, respectively, are currently receiving preventive therapy.24–26 The slow onset of efficacy (taking weeks to months) of preventive medications and side effects contribute to high discontinuation rates, particularly with oral therapies.25,27–30 Consequently, 40% of patients receiving preventive treatment still experience at least one migraine-related issue and 14% have two or more issues – the most common being disability and dissatisfaction with treatment.31 This highlights the poor efficacy of current treatments and the substantial unmet need for improved migraine prevention.
The impact of preventive treatment
Establishing and managing patient expectations
It is important to set realistic efficacy expectations with preventive migraine treatment. The patient’s treatment goal may be to become ‘pain free’ or to be able to function uninterrupted in a setting of known and consistent triggers. Appropriate headache education can make a significant difference in managing patient expectations for treatment and ultimately migraine control. The AHS suggests that evidence of treatment benefit may be provided by at least one of these criteria:1
- a reduction in mean monthly headache days of ≥50% compared with pre-treatment baseline, although some patients may experience benefits with smaller reductions
- a clinically meaningful improvement in a validated migraine-specific patient-reported outcome measure, including, but not limited to:
– a reduction from baseline of ≥5 points in the Migraine Disability Assessment (MIDAS; baseline score 11 to ≤20, moderate disability),32 Migraine Physical Function Impact Diary (MPFID) or 6-item Headache Impact Test (HIT-6) score– a ≥30% reduction from baseline in MIDAS score for patients with baseline scores of >20 points (severe disability)
– Other documented benefits reported by clinicians and patients
- latency in the onset of treatment action, which is an important aspect of most preventive agents that should be conveyed to patients who are understandably eager for prompt results.
Important considerations for setting expectations based on experts’ advice
The importance of each individual specific symptom to patients is variable, so a clear understanding of patient goals should be determined when creating a treatment plan. Symptoms beyond the headaches themselves can have a significant impact on patients and may underlie a lack of perceived improvement in health-related quality of life (HRQoL) after treatment, despite reductions in monthly migraine days.33 It is also important that patients are aware that the onset of action for most current preventive therapy can take weeks to months to reach steady state. Additionally, a 50% reduction in migraine days from baseline may be clinically meaningful;1 some patients may expect greater reductions or complete cessation of migraine days. Finally, to reduce potential misunderstanding or stigma, it should be emphasized that the preventive treatments are commonly prescribed for conditions such as depression or seizures, but they are also prescribed for patients with migraine.
Patient satisfaction with current preventive therapies
A retrospective database study by Hepp et al. suggested that many patients discontinue preventive oral migraine medication within 30 days, or do not collect their initial medication at all, and approximately half of patients discontinue after approximately 60 days (Figure 1A).30 In a separate retrospective cohort study, Woolley et al. found that 81% of patients (n=107,122) had a gap of >90 days in their migraine preventive treatment, and only 10% of the 86,329 patients with treatment gaps restarted preventive treatment within 1 year of the gap.29 The most common reasons for therapy discontinuation were lack of efficacy and side effects (Figure 1B).24 Discontinuation of one or more preventive medications was reported by 24% of the 672 respondents who experienced <15 headache days per month and by 41% of the 493 who experienced ≥15 headache days per month.24
Important considerations for patient satisfaction based on experts’ opinions
In patients who have treatment failure with several migraine drug classes and waited 3–6 months each time before knowing if a treatment was effective, feelings of frustration can be minimized by carefully explaining why a specific drug is being prescribed and why it is the best choice at a given time. Patients should also be made aware that treatments are not a cure; they will need to continue to seek medical care for migraine, and a pause or delay in treatment may lead to the return of symptoms. There are also considerations relevant to dosing and administration that are important. Patients may view treatments that require titration and multiple daily doses to reach steady state (as is required for some preventive migraine treatments) with concern, so the purpose of titration should be clearly explained. Patients may also be uncomfortable self-administering treatments at home, thereby contributing to non-adherence. Consequently, preferences concerning methods of treatment administration should be considered and support provided where necessary. Finally, physicians should be aware that chronic treatment with preventive medication can drive changes in patient behaviour as they recognize they have a chronic disorder.
Should we expect better?
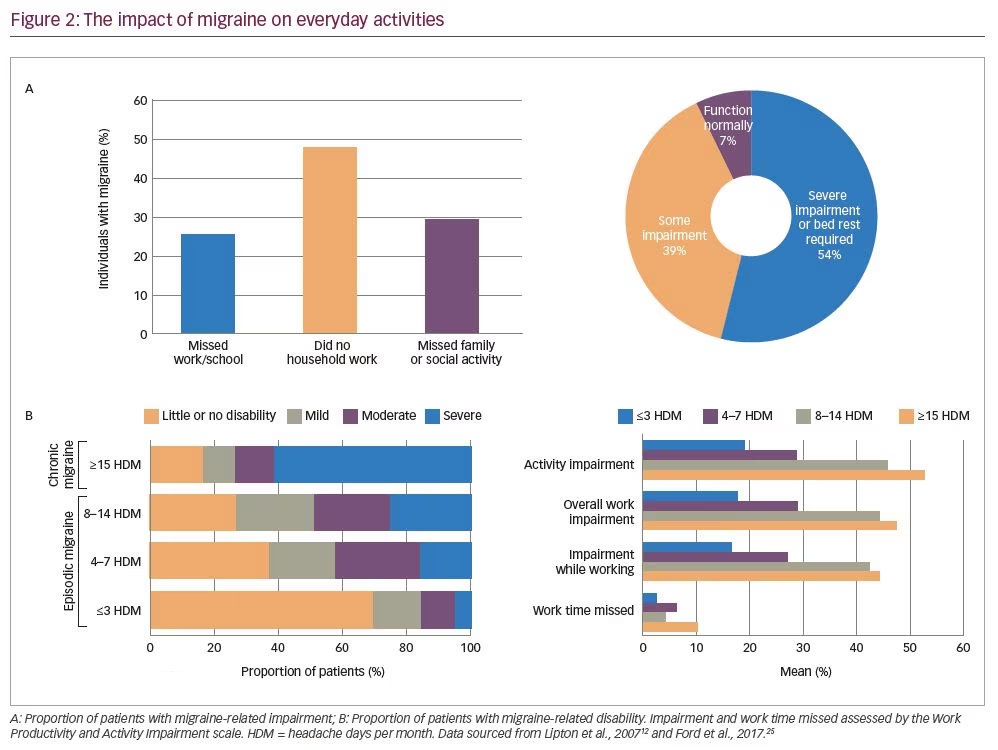
Despite the availability of preventive medications, the American Migraine Prevalence and Prevention (AMPP) study demonstrated that migraine-related impairment is common (Figure 2A): survey respondents reported missing work or school (25%), household work (48%) and family or social activities (29%) on one or more days in the previous 3 months.12 When asked how they are usually affected by severe headache, the majority of respondents experienced at least some impairment during a migraine, and 54% reported severe impairment or the need for bed rest.12 In the decade since the AMPP study was conducted, there has been little improvement in migraine-related disability, with over 60% of patients with chronic migraine reporting severe disability and over 40% of their work and activity time impaired (Figure 2B).25
Case study 1
A 32-year-old female chief surgical resident was experiencing 4–6 migraine days per month. The migraine attacks were accompanied by extreme pain, aura and other visual disturbances, and were completely disabling when they occurred during surgery. The attacks and related symptoms were managed reactively with acute therapies, including nonsteroidal anti-inflammatory drugs, triptans and antiemetics/dopamine receptor blockers administered in the emergency room. The patient was not amenable to anti-epileptic drugs due to possible cognitive impairment, and was not interested in other oral preventive treatments due to possible weight gain side effects. The patient was also showing signs of depression and anxiety, as she believed her condition may never improve and would interfere with her career. Following initiation of treatment with a CGRP inhibitor mAb preventive therapy, a reduction of approximately 50% in the number of migraine days per month was observed after 8 weeks, from 4–6 migraine days down to 2–3 days per month.
Treatment considerations for case study 1
The patient in case study 1 demonstrates several of the challenges and considerations in the treatment of migraine with currently available preventive treatments. Although the reduction in migraine days is beneficial, an unmet need for further reductions remains as the patient continued to experience significant headache burden and growing concern about her ability to function, especially at work. After careful consultation it was agreed that due to the nature of the patient’s surgical role, along with her anxiety and aversion to the possibility of cognitive impairment, she should consider CGRP inhibitor mAb treatments, over daily oral medications, as a means of improving efficacy and compliance with her treatment plan.
Patient candidates for preventive treatment
Goals of preventive treatment and candidacy
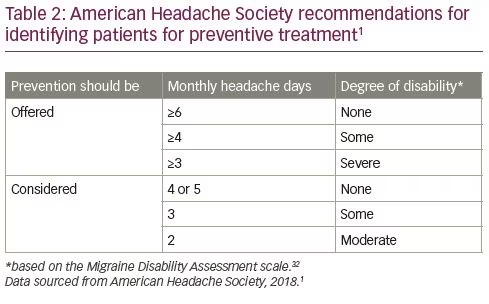
The goals of migraine prevention are to reduce the frequency and impact of attacks, improve function and treatment responsiveness, reduce treatment costs, enable patient management and improve HRQoL.1 The current AHS position paper on migraine treatment suggests that patients experiencing frequent migraine attacks (≥4 monthly migraine days and no disability, or ≥3 monthly migraine days and some disability) and some degree of disability are candidates for preventive treatment (Table 2).1
Impact of migraine days and degree of disability
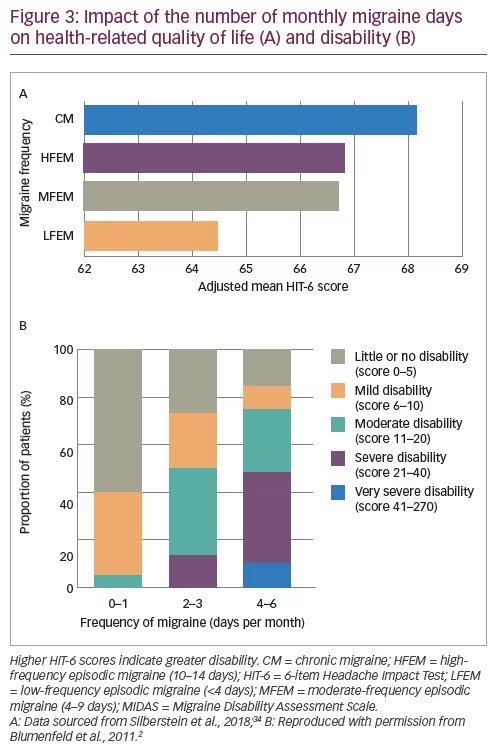
Migraine frequency often fluctuates between the definitions for episodic and chronic migraine, and is not always the best measure of migraine impact.15–17 For some patients, even a limited number of monthly migraine days is associated with a high degree of disability and impact on HRQoL (Figure 3A).2,34 The longitudinal Chronic Migraine Epidemiology and Outcomes (CaMEO) study, which surveyed adults with episodic and chronic migraine in the USA using an online questionnaire, showed that nearly three-quarters of patients with chronic migraine drop below the clinical threshold for chronic migraine at least once a year.4 Additionally, data from a cross-sectional survey of 1,347 respondents recruited from the US National Health and Wellness Survey demonstrated that although patients with chronic migraine have the highest disability, patients with episodic migraine also have substantial disability.34 Finally, the International Burden of Migraine Study (IBMS) investigated the relationship between the number of headache days per month and migraine-related disability and found that disability increased progressively with the number of headache days.2 Other studies have also found that even fewer than 4 headache days per month can result in severe disability (Figure 3B) in addition to the impairment during individual episodes.2,34 These study findings indicate that preventive treatment should be considered on a case-by-case basis.
Acute medication overuse can be an indication for preventive therapy
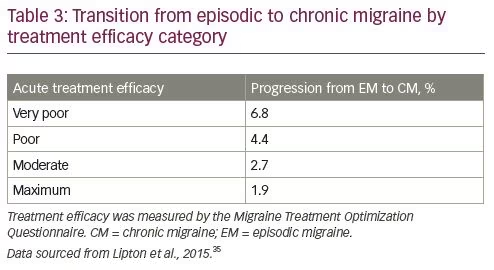
Preventive treatment initiation is also recommended for patients overusing acute migraine therapies, including the use of ergot derivatives, triptans, opioids, simple or combination analgesics, or a combination thereof for ≥10 days per month.1 Furthermore, the overuse of acute treatments could result in the development of chronic migraine, which could further reduce patient HRQoL.15 The longitudinal, population-based AMPP study included 28,261 participants who reported experiencing ‘severe headache’ in the preceding year.35 The study demonstrated that consistent failure of acute treatment to achieve complete and lasting relief, as measured by the Migraine Treatment Optimization Questionnaire, was significantly associated with the development of chronic migraine 1 year later (after adjustment for covariates, Table 3).35 Therefore, repeated acute treatment failure can result in more frequent attacks and greater disability.35 Together, this suggests that the appropriate treatment of episodic migraine might prevent or delay progression to chronic migraine.
Case study 2
A 55-year-old female law professor was experiencing 15–18 migraine days per month. Her headache days were accompanied by photophobia, phonophobia, nausea and dizziness, forcing her to frequently miss work. The patient’s primary care physician prescribed various acute therapies for over a decade to manage her condition when she was experiencing 3–5 migraine days per month. Her condition progressed such that she was experiencing headaches more days than not, and was using acute therapies for most episodes of migraine, averaging >10 days of acute treatment per month. She had a complex family/social background, including a mother with dementia who insisted on living alone, and a husband who was also a busy academic professor. She had considered applying for permanent disability but was distraught over the loss of her professional identity and the financial consequences from that decision. After 10 years of suffering from increasing monthly migraine attacks and lack of control with acute therapies, the patient decided to consult with a new healthcare practitioner, who suggested adding a preventive therapy to her treatment plan.
Treatment considerations for case study 2
The patient in case study 2 highlights several challenges in considering a suitable candidate for preventive treatments. The case history illustrates progression from 3–5 migraine days per month 10 years ago, when she was under the threshold for preventive therapy, to >15 migraine days per month while using only acute therapies. It also highlights how the impact of migraine on HRQoL is a more relevant factor in considering preventive therapy than simply the number of migraine days per month. The case indicates why the escalation of acute therapy should be considered a trigger for preventive medicine. Initially, the patient responded well to acute treatments, and did not consistently exceed 10 days per month of acute therapy use, so her physician recommended that she continue her existing treatments. However, even before reaching the 10 days per month acute therapy threshold, the patient’s use of acute medication had continued to escalate over time, indicating a lack of migraine control. As migraine attacks increase in frequency, they cause increasing interpersonal stress, impairment in activities of daily living and can contribute to medication overuse due to anticipatory anxiety;12,17,36 therefore, escalating acute therapy use could be a surrogate or ‘red flag’ for considering preventive treatments.
Discussion and conclusions
Significant advances in migraine prevention have made it possible to reduce the burden of migraine attacks and improve HRQoL in some patients. However, current oral preventive treatments have varying levels of effectiveness and side effects, and may take weeks or even months before providing meaningful improvements in HRQoL. These features are linked to high discontinuation rates,25,27–30 although newer injectable preventive therapies may mitigate these features, facilitating the achievement of patient goals. Preventive migraine treatments are recommended in the USA for patients who have at least 4 headache days per month, but the number of headache days per month is clearly not the only factor indicating a need to initiate or change preventive therapy. This is emphasized by patients having a poor HRQoL even with only a few monthly headache or migraine days.2 Taken together, these points illustrate a variety of unmet clinical needs in reducing disease burden among people with migraine. Existing preventive treatments have some efficacy but patients require education in their usage, and their expectations should be managed. Treatment choices should be made on an individual basis to align with the patient’s context, needs and goals.