Multiple sclerosis (MS) is an immune-mediated neurodegenerative disease affecting approximately 2.5 million individuals worldwide.1,2 Pathologically, MS is mostly characterized by inflammation, demyelination, axonal degeneration and gliosis. Clinically, a wide range of symptoms can occur, including cognitive, motor and sensory impairments.3
The clinical disease course is often classified as relapsing-remitting MS, primary-progressive MS or secondary-progressive MS.4 Relapsing-remitting MS is defined as having stable neurological disability between acute episodes. These acute episodes involve monophasic clinical attacks with patient-reported symptoms and objective tests reflecting a focal or multifocal inflammatory demyelinating event in the central nervous system. In contrast, progressive MS is characterized by steadily heightened, objectively documented neurological disability independent of episodes. The primary-progressive type is diagnosed based on a progressive course from disease onset, whereas the secondary-progressive type is characterized by an initial relapsing-remitting course that develops into a progressive course.4 Most individuals are diagnosed at a young age, commonly between 20 and 50 years, and so far, no curative treatment exists.5 Thus, patients are confronted with a chronic, long-lasting, progressive disease,3 accompanied by worsening neurological deficits that limit daily activities and general societal participation.6 Therefore, optimal care is a fundamental issue for clinicians as well as researchers.
Despite this need, comprehensive care is challenging due to the disease’s complexity.1 First of all, its diagnosis is based on the presence of neurological symptoms and signs, alongside magnetic resonance imaging findings, cerebrospinal fluid examinations, neurophysiological testing, such as evoked potentials, and other laboratory investigations to rule out other conditions that mimic MS.7 After the diagnosis, the extensive range of symptoms – including spasticity, bladder, bowel and sexual disturbances, pain, fatigue and cognitive impairment – requires specific treatment. Consequently, a variety of clinical disciplines need to be involved in a patient’s care, such as neurology, speech therapy and neuropsychology.1
Disease-modifying treatments (DMTs) include a range of drugs with various mechanisms of action and adverse effects requiring intensive monitoring.8 Appropriate monitoring involves a large set of investigations, such as magnetic resonance imaging or immunological tests, which demand an advanced level of organization. Together, the disparate nature of MS manifestations creates challenges for clinical coordination and organization, emphasizing the need for efficient multidisciplinary patient care aimed at maintaining patients’ quality of life (QOL) and autonomy.
Recently, researchers and clinicians have promoted the establishment of specialized centres to meet these needs and offer a comprehensive approach to MS healthcare.1,9 Globally, several clinical centres intend to optimize their delivery of care for patients with MS by reorganizing existing resources and incorporating new resources into multidisciplinary MS care units.9–11 A multidisciplinary MS care unit approach involves different specialists – MS neurologists, nurses and therapists – working together. Such units have formalized protocols and procedures for the diagnostic workup, initiating and following up on DMT use, and managing complications.1
Restructuring existing care into a multidisciplinary MS care system would enable appropriate, timely and targeted diagnosis and better and more efficient management of treatment complexity, and a comprehensive intervention spectrum.1 These benefits may increase a patient’s safety when treated with DMTs.1 Moreover, the presence of multiple MS experts might facilitate timely discussions about diagnostic and therapeutic challenges.1 Additional benefits could include the availability of expert nurses or therapists to carry out tasks and offer a clear point of contact for providing information, support and advice. Thus, they might create individualized relationships offering higher levels of comfort.1 Ultimately, MS care units may offer a societal benefit by being more cost-effective, reducing disability claim benefits and the need for familiar caretakers by preserving the patients’ autonomy and work ability.1
Reliable and validated measures are needed to monitor, evaluate and improve the quality of multidisciplinary MS care units. In 2001, the US Institute of Medicine of the National Academy of Medicine emphasized the importance of systematic quality management in healthcare to enhance the likelihood of achieving the desired health outcomes.12 Specifically, prior work has established patient satisfaction as a major factor of interest for such quality assessment since higher satisfaction has led to increased therapy compliance and active disease management.9 Hence, it is particularly important to understand and integrate the patient’s opinion to improve the quality of their care.
The aim of this single-centre pilot study was to exemplify and evaluate the quality of a multidisciplinary MS care unit by assessing patient satisfaction before and after the reorganization of a Swiss clinical centre. Since the goal of MS care is to maintain or increase a patient’s QOL and autonomy, we included a recognized QOL scale as an efficacy measure.1
Methods
Participants and procedure
This research was a single-centre study involving patients with a confirmed clinical diagnosis of MS (either relapsing-remitting or progressive MS) and currently receiving infusion therapy at the clinical centre in Biel, Switzerland. Eligible participants had to be 18 or older. There were no other exclusion criteria.
Patients received an intravenous injection of either ocrelizumab or natalizumab between November 2019 and May 2020. Prior to this study, the infusion site was located at the internal medicine ambulatory care unit. Consequentially, the preparation of diagnostic procedures, such as lumbar punctures and blood tests, and the administration of intravenous DMTs had to be coordinated between the neurological and internal medicine departments. Notably, the nursing staff and the physicians at the site were not specialized in MS care. Moreover, the cross-coordination led to delays in diagnosis and treatment in the majority of cases.
Statistical analyses
All survey data are reported descriptively and expressed as means and standard deviations (SDs) or as a percentage of participants and percentage points. To test whether patient satisfaction and QOL changed from before to after the reorganization of the clinical centre, pre- and post-scores for total satisfaction and QOL scores were compared using Wilcoxon signed-rank test for non-parametric, dependent ordinal data. To investigate whether baseline QOL scores were positively associated with greater differences in satisfaction, a satisfaction change score was calculated (post-test score – pre-test score). A correlational analysis was done using Spearman’s rank order correlation for non-parametric and at least ordinal data. A p-value of ≤0.05 was considered significant. The statistical analysis was done with IBM SPSS Statistics 26 (IBM Corp., Armonk, NY, USA).
Results
Demographics
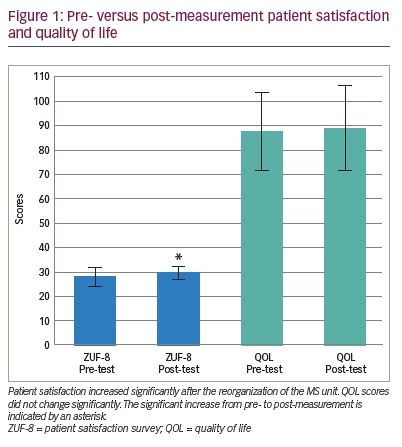
Of 24 patients who received the questionnaire, 19 returned the pre- and post-measurement surveys and were eligible for analysis. Demographics and sample characteristics are displayed in Table 1. The sample consisted of 11 female and 8 male patients. Eleven participants spoke German, and eight participants spoke French. The participants’ mean age was 38.89 years (SD: 9.89). Six patients received ocrelizumab, whereas 13 patients received natalizumab as infusion therapy. The mean duration of disease was 6.95 years (SD: 4.94).
Patient satisfaction and quality of life
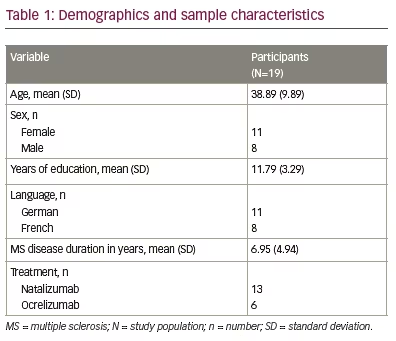
All the assumptions for using the Wilcoxon signed-rank test were met for patient satisfaction and QOL scores. Patient satisfaction scores increased significantly from pre- to post-measurement (z=-2.227; p=0.025; n=19). Based on Cohen (1992), the analysis of satisfaction scores has a strong effect size (r=0.51).13 Pre- and post-measurement mean (SD) satisfaction scores are shown in blue in Figure 1.
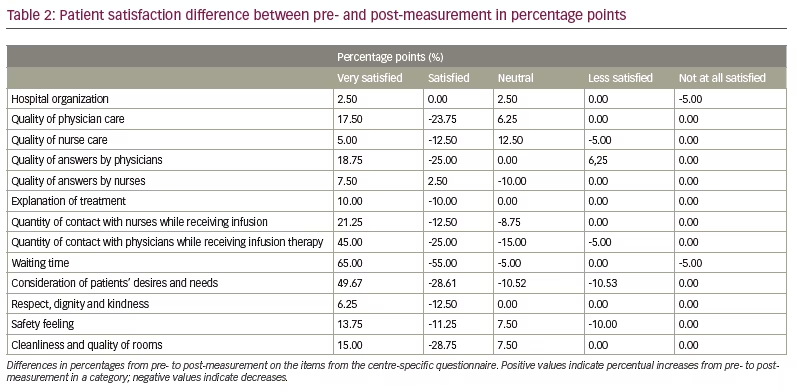
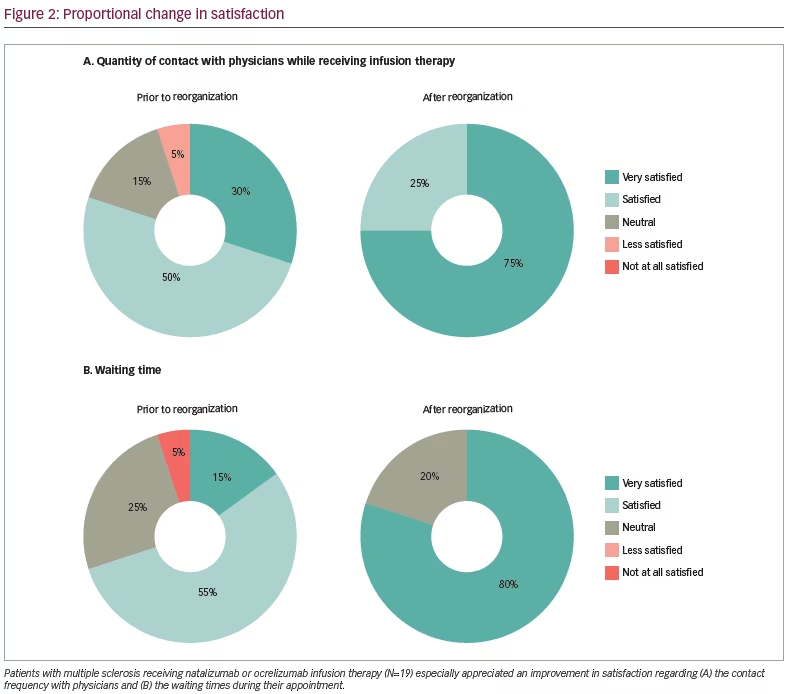
The questionnaire designed specifically for the clinic showed an overall increase in satisfaction by a percentage point improvement on several items. Satisfaction increase or decrease in percentage points for all items from pre- to post-reorganization is shown in Table 2. All items demonstrated an increment from pre- to post-measurement in the category of “Very satisfied”. For illustrative purposes, two of the items showing the highest proportional differences between pre- and post-measurement, namely “Quantity of contact with physicians while receiving infusion therapy” and “Waiting time”, are depicted in Figure 2.
In contrast, QOL did not change significantly (z=-1.379; p=0.18; n=19). Figure 1 displays the pre- and post-measurement mean (SD) QOL scores as green bars. Baseline QOL scores and satisfaction change scores showed no association, as analysed using Spearman’s correlational coefficient (r=0.163; p=0.504; n=19). The test assumptions were met.
Discussion
This single-centre pilot study investigated whether a multidisciplinary care unit approach improved the satisfaction and QOL of patients with MS who were receiving infusion therapy at a Swiss clinical centre. At the centre, former MS care structures were reorganized to offer a specialized MS care team including neurologists, nurses, speech therapists and neuropsychologists working together and individualizing each patient’s care. Patients’ satisfaction increased after the reorganization, while QOL scores remained the same. Baseline QOL scores did not predict changes in patient satisfaction.
These findings support the recently promoted specialized multidisciplinary approach for MS.1,9 Using patient satisfaction as the primary measure of quality, these findings indicate an overall improvement in the perceived clinic quality and the care it is offering since patient satisfaction has repeatedly been shown to be a validated proxy for quality of care.14–16 Prior work suggests that more satisfied patients are more likely to comply with treatment, to actively participate,15 and to be more optimistic about their future.16 These aspects are especially relevant for patients with a chronically impairing disease such as MS. Thus, the current findings exemplify that patients with MS might benefit from the reorganization of current MS care structures into more comprehensive and thoroughly coordinated multidisciplinary units. Future multicentre examinations of this issue are needed to validate the findings.
Since the topic of MS specialized multidisciplinary care is a relatively new clinical research topic, the current findings provide some of the first empirical evidence that such care increases patients’ satisfaction. Emphasizing the specific aspect of care providers, a pilot study by Thotam and Buhse (2020) evaluated patient satisfaction with nurses and physicians in specialized MS centres.15 In accordance with our findings, they showed that patients were highly satisfied with both groups within these settings, assessing satisfaction attributes such as general satisfaction, technical quality, interpersonal manner, communication, financial aspects, accessibility and convenience, and time spent with a provider. However, this study mainly compared nurses and physicians only and did not consider other non-specialized settings or longitudinal measurements. Another study by Becker et al. (2018) emphasized the importance of a specialized MS approach and reported that two-thirds of 2,791 patients were satisfied with their therapy in such MS centres.9 They focused their assessment of patient satisfaction mainly on the medical treatment, examining aspects such as advantages and disadvantages of current medication, the frequency with which information was obtained, and continuation of treatment. The pharmacological treatment might be an important aspect to consider in future analyses of patient satisfaction in this field; however, it may be too restrictive to only focus on the satisfaction related to patients’ medication. Additional attributes of satisfaction not directly concerning medication, such as organization, waiting times or interpersonal communication, might be missed. Therefore, future examinations are encouraged to include all these aspects to provide a comprehensive assessment of patient satisfaction.
Another aspect of the current findings is the importance of quality assurance measures, not only for the patient but also for clinics. These measures help to monitor and evaluate the quality progress and, therefore, help to build high-quality performance organizations.17 Our centre-specific quality survey emphasized that patients especially appreciated the contact frequency with physicians and a reduced waiting time and has highlighted areas with lower satisfaction, which need improvement, such as the overall organization and communication with patients.
Healthcare professionals have to be considered as one of the major contributing factors to ensuring high-quality healthcare,18 so future assessments ought to evaluate the opinions and suggestions of MS care professionals. It is possible, for example, that professionals’ and patients’ perspectives may differ on treatment comfort and patient status, as well as care goals and challenges.9 For example, a study by Tintoré et al. (2017) identified several deviating opinions between 982 patients and their neurologist concerning treatment selection, satisfaction, expectations, goals, and comfort discussing symptoms, treatment challenges and skipped doses.16 Hence, the study suggests the importance of systematically tracing these differences. On the other hand, considering and improving healthcare professionals’ work conditions has additionally been shown to increase care quality and patient safety.19,20 Therefore, further institutional quality assessments should incorporate professionals’ opinions on patients’ treatment and their valuable experiences concerning their own work environment.
The current analysis found no increase in QOL scores nor an association between baseline QOL scores and satisfaction change scores pre- and post-reorganization. This may be due to the short time interval between pre- and post-measurement and to our taking only one post-measurement. A longer time interval and more measurement time points could help identify possible changes in patients’ QOL. Notably, this study was done as a pilot study with the intention to continue patient satisfaction and QOL measurements half-yearly, so future investigations might show different results.
The present study has some limitations. Firstly, the sample size was small; however, the opinion of only a few patients is still of high importance for the improvement of the clinical service. This small-scale study was intended to exemplify the importance of this comprehensive practical approach for other clinical centres and pave the way for future large-scale research into MS treatment improvement. Secondly, the exceptional situation of the COVID-19 pandemic may have affected our findings. For example, patients’ feelings of safety may have been generally decreased and might have diminished the positive influence of the reorganization on patients’ perceived safety.
Conclusion
Multidisciplinary MS care units may offer improved care to patients with MS, a chronic neurodegenerative disease. The present small-scale study demonstrated that the reorganization of care into such a unit improved satisfaction among patients with MS being treated at a Swiss clinical centre. We hope these findings offer an example for other clinical centres and suggest that future studies should focus on longitudinal, large-scale data collection to further understand this important topic.