Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disorder of upper and lower motor neurons that results in progressive motor impairment. ALS is the most common disease of motor neurons with an annual incidence of approximately 1.7–2.5 per 100,000 people. It is a terminal condition with a typical life expectancy of 2–5 years from symptom onset. ALS remains invariably fatal despite extensive clinical research aimed at the development of effective disease-modifying therapeutic interventions. Presently, most of the approved therapeutics in clinical use for ALS have a modest impact on clinical progression and/or survival. While most patients with ALS will have no family history of the disease, approximately 15% of ALS cases are familial, with almost all having an autosomal dominant pattern of inheritance.1 In 1993, mutations in superoxide dismutase 1 (SOD1) were identified as the first genetic cause of familial ALS (fALS).2 Since the discovery of SOD1-associated ALS, numerous additional genes have been associated with ALS. Mutations in SOD1 remain the second most common cause of fALS behind pathogenic hexanucleotide repeat expansions in C9orf72 in European and North American populations, with C9orf72-ALS accounting for approximately 10–20% of fALS cases and 2% of all ALS cases.3
Natural history of SOD1-ALS variants
Similar to other forms of ALS, the natural history of SOD1-ALS is heterogeneous. SOD1-ALS predominantly follows an autosomal dominant inheritance pattern, with one exception being the p.D91A variant, common in Scandinavian populations, which is inherited in an autosomal recessive pattern.4 The association between p.D91A heterozygosity and SOD1-ALS remains somewhat controversial. Since 1993, more than 100 unique pathogenic or likely pathogenic mutations have been identified in SOD1. The ALS online database was established to collate information about genes and unique genetic variants that are causative or associated with ALS.5 Most identified pathogenic mutations are point mutations, resulting in single amino acid substitutions. The most common pathogenic SOD1 variant in North America is a mutation-substituting alanine for valine at codon 5, known as the p.A5V variant. The p.A5V variant has been recognized for its association with rapidly progressive fALS since 1994.6 In 1997, Cudkowicz et al. published an epidemiological study of 366 families with dominantly inherited fALS.7 This study detected SOD1 mutations in 68 families. The p.A5V variant was detected in 50% of SOD1-ALS families. The natural history of ALS, both forms associated with pathogenic mutations in ALS genes and in those without known genetic mutations, varies widely on an individual patient-to-patient basis with some patients surviving only a few months from symptom onset and others living for decades. In the SOD1-ALS population, patients with p.A5V SOD1-ALS have a markedly shortened disease duration (i.e. survival), while p.G38R, p.G42D, p.G94C and homozygous pD91A variants are associated with longer survival times. The average disease duration in patients with p.A5V SOD1-ALS is only 12–18 months.7 In 2017, Bali et al. published a retrospective cohort natural history study of 175 patients with SOD1-ALS from 15 centres of the Northeast ALS Consortium (NEALS) network collected over a 16-year period to improve understanding of the natural history of SOD1-ALS, guide therapeutic clinical trial design and provide historical control data for future studies.8 In this cohort, 63 participants (36.4%) had p.A5V mutations and 112 (63.6%) had non-p.A5V mutations. There were a total of 36 distinct SOD1 mutations. The four most common mutations representing two-thirds of the participants were p.A5V, p.I114T, p.G42D and p.E101K. The median survival was 1.2 years in the p.A5V group and 6.8 years in the non-p.A5V group. The mean age of onset for SOD1-ALS in this cohort was approximately 50 years and did not vary between p.A5V and non-p.A5V groups. The p.G42D mutation was again found to have a slower rate of progression with an average survival of 23.5 years from symptom onset, similar to findings reported by Cudkowicz et al. mentioned above.
Pathogenesis of SOD1-ALS
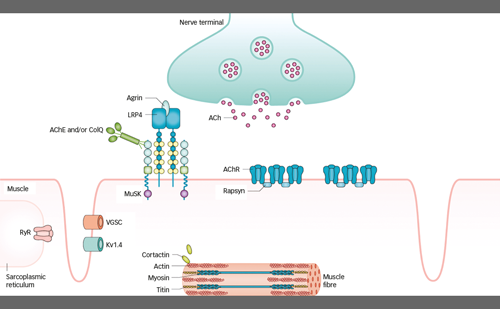
The pathogenesis of ALS is complex and likely multifactorial. The proposed pathophysiologic mechanisms include oxidative stress, mitochondrial dysfunction, glutamate excitotoxicity, prolonged activation of the intrinsic stress response, impaired axonal transport and accumulation of toxic intracellular aggregates. Genetic forms of ALS present a unique opportunity to investigate and better understand the pathogenesis of both familial and sporadic forms of this neurodegenerative disease. Genetic forms of ALS also provide prospective targets for the development of therapeutic interventions. SOD1 encodes for the Cu/Zn-binding superoxide dismutase metalloenzyme. This enzyme is ubiquitously expressed and converts toxic superoxide anions into oxygen and peroxide to reduce this toxic reactive oxygen species.9 Early studies of families with SOD1-ALS demonstrated that SOD1 activity was reduced in affected family members to less than half the activity level of controls and patients with sALS. This enzyme level abnormality is detectable years before the onset of clinical ALS in carriers of pathogenic SOD1 mutations.9 However, the toxicity of mutant SOD1 is not related to the loss of SOD1 activity. Transgenic mouse models with human SOD1 G93A develop motor neuron toxicity despite the little effect of this mutation on SOD1 enzyme activity.10 SOD1 mRNA levels are elevated in SOD1-ALS, as well as in non-SOD1-ALS, suggesting a potential toxic effect of mRNA accumulation and the possibility that oxidative stress plays a role in ALS pathogenesis.11 Patients with SOD1-ALS develop insoluble intracellular SOD1-containing aggregates in motor neurons. SOD1-containing aggregates form prior to clinical symptom onset and grow in number with disease progression.12
Preclinical studies
Pathologic studies of a variety of neurodegenerative diseases, including ALS, Alzheimer’s disease, Huntington’s disease, Parkinson’s disease and a variety of tauopathies, have identified aggregates of toxic proteins that contribute to neuronal death in these disorders.13 In SOD1-ALS, SOD1 mutations are believed to result in a toxic gain of function, and mutant SOD1 mRNA contributes to the formation of toxic aggregates.14 Therapeutic strategies have been investigated to target and reduce the toxic SOD1 mRNA as a means of disrupting the pathophysiology in SOD1-ALS. Prior studies have investigated viral vector delivery of siRNA molecules to accomplish this goal, but this strategy was limited by a lack of ability to discontinue therapy, adjust dosage or guarantee even penetration throughout the central nervous system (CNS).15–20 Antisense oligonucleotides (ASOs) are another approach that has gained traction in the treatment of several neurodegenerative disorders. ASOs are short, synthetic oligonucleotides designed to target specific mRNA sequences of interest. An ASO binding to a target mRNA sequence creates double-stranded RNA, and with the right modification, it can become a target for degradation by endogenous RNAse H.21 ASO therapies are unable to cross the blood–brain barrier, but intrathecal administration allows ASO therapies access to the CNS, and specifically, to motor neurons in the case of SOD1-ALS. This ‘mRNA knockdown’ strategy has demonstrated target engagement and effectively reduced levels of SOD1 mRNA in SOD1-ALS animal models and patients.22 In 2006, Smith et al. published animal data on rats and non-human primates exposed to continuous intrathecal infusion of an ASO-targeting SOD1 that demonstrated widespread tissue penetration throughout the brain and spinal cord, prominent uptake in the ventral horn and, at the cellular level, in motor neurons, as well as target engagement with a dose-dependent reduction in SOD1 mRNA levels to 25–40% of normal levels.22 Additionally, this study tested an ASO-targeting human SOD1 mRNA in a transfected rat model with a human G93A SOD1 mutation and found that it similarly dramatically reduced mutant SOD1 mRNA and SOD1 protein in the rat model throughout the brain and spinal cord as well as in fibroblasts from symptomatic patients with p.A5V SOD1 mutations. ASO treatment in the rat G93A SOD1 mutant model also resulted in extended survival compared with saline-infused rats.22 The results of this study suggested that mRNA knockdown ASO therapies may be an effective strategy for multiple neurodegenerative diseases involving toxic gain of function mechanisms and laid the promising groundwork to move forward with clinical trials adopting this strategy. Since this publication, ASOs have been developed to target a variety of other neurodegenerative disorders, including Huntington’s disease, spinal muscular atrophy and hereditary transthyretin amyloidosis.23–25 In 2013, Winer et al. established that SOD1 levels could be reliably measured in the cerebrospinal fluid (CSF) and used as a potential biomarker for the demonstration of target engagement for ASO and other mRNA knockdown treatment strategies using the human G93A SOD1 mutant rat model.26
Clinical studies
In 2013, Miller et al. published the first study of intrathecal ASO delivery in humans.27 This phase I, randomized, placebo-controlled, first-in-human study of intrathecal ASO delivery was tested on a cohort of 32 patients with SOD1-ALS. As the prior animal model studies were treated with continuous ASO infusions, this first-in-human study assessed the safety and tolerability of a single intrathecal infusion given for more than 11 hours. In the small phase I trial, intrathecal dosing was well tolerated with no dose-limiting toxicities or serious adverse events. Common side effects included post-lumbar puncture headache and local back pain at the procedure site judged to be procedure-related and not attributable to the ASO. Additionally, one patient with SOD1-ALS with a p.A5V mutation died shortly after participation in this study, and the autopsy of the brain and spinal cord tissue compared with untreated patients with SOD1-ALS and sALS demonstrated a lumbar-to-cervical ASO concentration gradient in the tissue at 12.5 weeks after dosing, which was consistent with its patterns and levels as seen in preclinical rhesus monkey studies.27 This proof-of-concept work laid the foundation for future clinical studies aimed at the utilization of intrathecally administered ASOs as a potential therapy for patients with SOD1-ALS. Simultaneously, studies assessing stable isotope labelling kinetics (SILK) demonstrated the ability to track protein production and clearance in the human CNS in vivo, including SOD1. Crisp et al. demonstrated that an orally administered SILK protocol could reproducibly measure SOD1 turnover in the CSF of human subjects and can distinguish between wild-type and mutant SOD1.28 The ability to track SOD1 protein kinetics provided a new biomarker opportunity to demonstrate target engagement for SOD1 mRNA-lowering therapies. Using this technology, the half-life of CSF SOD1 protein was determined to be approximately 25–30 days, which has been instrumental in clinical trial designs and dose schedules for SOD1-ASO clinical trials. Self et al. demonstrated that new production of human SOD1 protein in the CSF in mice could be lowered with an SOD1-targeting ASO and that this effect on new production of SOD1 could be seen at 10 and 30 days.29,30
A phase I–II, multicentre, international randomized, double-blind, placebo-controlled trial of an intrathecally delivered ASO (tofersen) for SOD1-ALS was published by Miller et al. in 2020.31 A total of 50 participants were assigned to placebo or one of four doses of tofersen (20, 40, 60 or 100 mg) to assess safety, tolerability, pharmacokinetics and pharmacodynamics of tofersen. Tofersen was delivered by intrathecal bolus injection on days 1, 15, 29, 57 and 85 of the study. CSF SOD1 protein concentrations were measured at baseline and day 85 to assess target engagement. Mild procedure-related adverse effects were common. Asymptomatic elevations of CSF white blood cell count and protein were seen in several participants. CSF SOD1 protein concentration was significantly reduced from baseline in the 40, 60 and 100 mg groups in a dose-dependent manner and was unchanged in the placebo group, confirming target engagement by tofersen. Exploratory outcomes investigating change in ALS Functional Rating Scale-Revised (ALSFRS-R) and slow vital capacity (SVC) suggested a slower decline in ALSFRS-R in faster-progressing p.A5V participants receiving the 100 mg dose compared with controls. The mean ALSFRS-R change from baseline to day 85 in participants receiving tofersen 100 mg was -1.19 (95% confidence interval [CI], -4.67 to 2.29) compared with -5.63 (95% CI, -8.90 to -2.36) in participants receiving placebo. In the p.A5V/faster-progressing subgroup, the mean ALSFRS-R change from baseline to day 85 was 0.84 (95% CI, -5.58 to 7.26) compared with -16.73 (95% CI, -23.28 to -10.18) in participants receiving placebo. The mean percentage decline in predicted SVC from baseline to day 85 was -7.08 (95% CI, -14.69 to 0.54) in the tofersen group compared with -14.46 (95% CI, -21.79 to -7.12) in the placebo group. In the p.A5V/faster-progressing subgroup, the mean percentage decline in predicted SVC was -8.62 (95% CI, -20.90 to 3.66) in the tofersen group compared with -30.31 (95% CI, -43.28 to -17.34) in the placebo group. As these measurements were exploratory outcomes and the study was not powered to establish efficacy, no statistical analysis or p-values were calculated. Neurofilament concentrations were also evaluated as an exploratory outcome, and there were notable decreases in CSF neurofilament heavy chain and plasma neurofilament light chain (NfL) at day 92 in the group treated with 100 mg of tofersen compared with no change in the placebo group, suggesting that this could be another useful marker of biological effects in clinical trials.31 Participants who completed the phase I/II studies were offered the opportunity to continue to receive tofersen through an open-label extension (OLE) study.
The phase III, multicentre, international, randomized, double-blind, placebo-controlled VALOR (ClinicalTrials.gov identifier: NCT02623699) trial evaluated the clinical efficacy and safety of intrathecally delivered tofersen (100 mg dose) in 108 participants with SOD1-ALS.32 There was a 28-week randomized portion of the trial (24 weeks of treatment plus 4 weeks of follow-up). The primary endpoint of the trial was a change in the ALSFRS-R score from baseline to week 28. The primary outcome was evaluated among the 60 participants predicted to have faster-progressing disease (based on pre-randomization delta ALSFRS-R). The secondary endpoints included measures of change in CSF SOD1 protein concentration, plasma NfL, SVC and handheld dynamometry (HHD). The VALOR trial participant size and duration of the study were determined based on 12 SOD1 mutation carriers with rapidly progressive disease in the placebo arm of the prior phase I–II tofersen study and a phase II trial of arimoclomol.33 The primary endpoint in the 60 prespecified fast-progressive participants showed no difference in change from baseline ALSFRS-R at 28 weeks (-6.98 points in the tofersen group, -8.14 points in the placebo group, p=0.97). The secondary endpoints were suggestive of clinical benefits, as detailed below; however, statistical analysis was not performed on these secondary endpoints because the primary endpoint did not show statistical significance. The secondary endpoint CSF SOD1 protein concentration data among the 60 fast progressors demonstrated a 29% reduction in the CSF SOD1 protein level in the tofersen group compared with a 16% increase in the placebo group, confirming target engagement. The slower progressing group showed a 40% reduction in the CSF SOD1 protein level. The neurofilament data for the fast-progressors demonstrated a 60% decline in plasma NfL in the tofersen-treated group compared with a 20% increase in the placebo group, demonstrating a biological effect on a validated ALS biomarker. SVC declined by 14.3 points from baseline to week 28 in the tofersen group and declined by 22.2 points in those who received placebo. HHD scores at week 28 were similar between the tofersen and placebo groups. Participants were also offered the opportunity to receive tofersen through the OLE after completing the VALOR study. Of the 108 participants in VALOR, 95 participated in the OLE. Analysis was performed at 52 weeks to compare results in participants who were randomized to the tofersen group at onset compared with those who switched from placebo to drug in the OLE portion of the study. Biomarker data from the OLE demonstrated sustained reductions in CSF SOD1 protein levels and plasma NfL in the early-start group, and the delayed-start group saw a comparable decline in CSF SOD1 protein and plasma NfL concentrations during the OLE. Clinical outcomes from the OLE measured at 52 weeks from enrolment in VALOR demonstrated a delta ALSFRS-R of -6.0 points in the early-start group compared with -9.5 points in the delayed-start group. A decline in SVC from VALOR baseline was -9.4% in the early-start group and -18.6% in the delayed-start group. A change in the HHD mega-score from the VALOR baseline was -0.17 in the early-start group and -0.45 in the delayed-start group. Overall, the VALOR study demonstrated clear evidence of target engagement and biomarker reduction with the reductions in CSF SOD1 protein and plasma NfL, but the study failed to meet the primary clinical endpoint at 28 weeks. The OLE data did suggest a benefit of tofersen treatment in clinical parameters, including ALSFRS-R score, SVC and HHD mega-score in the early-start over the delayed start group, leading many to advocate for US Food and Drug Administration (FDA) approval. Rare serious adverse neurological events occurred in approximately 7% of patients treated with tofersen during this larger trial. These serious adverse neurological events included myelitis, chemical or aseptic meningitis and papilledema/intracranial hypertension. Radiculitis and post-dose myalgias and/or radicular pain have also been described. An asymptomatic increase in CSF leukocytes and protein is common. A recently published manuscript provided extensive details on the CSF profiles observed in participants in symptomatic SOD1-ALS participants treated to date in the tofersen program and a more detailed account of the serious adverse events observed in this group of participants.34 Additional cases and case series have been published providing additional details on patients with complications of myelitis, headache and radiculitis.35–39
Aside from the objective results of the VALOR trial, this trial taught the field several valuable lessons that have changed the landscape for planning future ALS clinical trials. Most ALS clinical trials have used a change in ALSFRS-R as a way of determining fast and slow progressors in trial design, as well as using this as an outcome measure. In a post hoc analysis of the VALOR trial, plasma NfL concentrations were found to be a better predictor of the rate of progression than a pre-trial change in ALSFRS-R. Additionally, the OLE portion of the study showed a clear separation between the groups treated with tofersen versus placebo on multiple clinical endpoints at 52 weeks, suggesting that the commonly used ‘6-month’ study may be too short for ALS clinical trials and that longer duration trials are needed to confirm or refute the efficacy of new therapeutics. Specifically with regard to tofersen in SOD1-ALS, it is perhaps not surprising that the demonstration of clinical benefit/efficacy lagged behind the evidence of biological effects (i.e. lowering of SOD1 protein as well as mRNA and neurofilament reduction), particularly when one considers the half-life of SOD1 protein in the CNS from the SILK studies mentioned above as well as the known lag between the onset of therapeutic effects and clinical benefits in other neurologic disorders associated with neuronal and axonal degeneration (e.g. nerve regeneration in peripheral nervous system vasculitis and conditions such as Guillain–Barré syndrome). However, extending the duration of placebo-controlled trials to 12 months or longer may raise ethical dilemmas with regard to potentially enrolling rapidly progressing participants with a median survival of 12–18 months into a placebo arm. This debate has been a central discussion point in an ongoing phase III study of an ASO targeting fused in sarcoma RNA-binding protein (FUS), which is a longer duration trial in a form of ALS that is often characterized by a younger age of onset and rapid progression. Alternatively, the promising evidence of biomarker improvement seen in the NfL data in VALOR that preceded clinical benefits could be considered as an endpoint for future placebo-controlled trials to allow participants access to potentially beneficial trial agents at an earlier time point than would be allowed with an extended placebo-controlled period. Indeed, tofersen received accelerated approval from the FDA in April 2023 based on the NfL data as a readout of a biological effect, and this may provide a precedent for future therapeutics.
Since the publication of the VALOR trial, there has been a wealth of anecdotal experience with tofersen in SOD1-ALS among providers, particularly those who have been involved in the SOD1-ALS tofersen studies and the expanded access program.37–41 Patients, family members, clinicians and researchers have observed participants with SOD1-ALS clinically stabilize and even improve with apparently sustained responses to treatment. Following accelerated approval from the FDA in the spring of 2023, tofersen is now marketed under the trade name Qalsody® (Biogen MA Inc., Cambridge, MA, USA).
Future directions
A major challenge in the clinical care of ALS is that treatments are often initiated late in the course of the disease. By the time patients receive a diagnosis of ALS, they are often relatively late in the disease course, with average delays of ~1 year from symptom onset to diagnosis in most countries.42–44 Similar to hypotheses that have been explored for decades in other neurodegenerative disorders (e.g. Alzheimer’s disease), there is a strong belief among experts in the field, and likely demonstrated by the findings of the VALOR + OLE study, that earlier therapeutic intervention is likely to have a more profound impact on halting or slowing the natural progression of this disease. Genetic forms of ALS such as SOD1-ALS have presented a unique opportunity to identify pre-symptomatic carriers of variants with high clinical penetrance, thereby allowing investigators to identify early biologic markers of disease activity (i.e. biologic phenoconversion) that precede clinical signs/symptoms of disease, as well as trial therapeutic agents in this ‘pre-symptomatic’ stage of the disease. As alluded to above, pre-symptomatic biomarker changes have been established in several other neurodegenerative conditions, including Alzheimer’s disease, Parkinson’s disease and Huntington’s disease with evidence of biomarker changes years to decades prior to clinical manifestations.45–47 Benatar et al. first suggested that NfL might be a promising early biomarker of phenoconversion in pre-symptomatic ALS.48 In this study, 10 pre-symptomatic carriers of fALS gene mutations phenoconverted to symptomatic ALS (9/10 were SOD1, 8 of which were p.A5V carriers), allowing the study to assess changes in NfL around the time of phenoconversion in SOD1-ALS. Baseline plasma neurofilament levels were comparable between control and pre-symptomatic fALS mutation carriers and were expectedly higher in symptomatic ALS participants. The longitudinal plasma neurofilament data from this study indicated stable NfL levels in control and symptomatic ALS participants, but pre-symptomatic fALS mutation carriers who phenoconverted to symptomatic ALS during the study showed a consistent rise in plasma NfL well before clinical symptom onset, and values continued to rise for at least 6 months into the clinical course. All plasma NfL levels in phenoconverters >1 year prior to symptom onset were comparable to control participant levels. These results strongly suggested the utility of plasma NfL as a preclinical biomarker for the onset of neurodegeneration in SOD1-ALS, which is a finding suggestive of a potential pre-symptomatic window to initiate therapeutic interventions before clinically manifesting the disease.49 A follow-up study by Benatar et al. in 2019 demonstrated that the rise in plasma NfL in SOD1-ALS phenoconverters typically occurred 6–12 months prior to first clinical symptoms.50 Plasma NfL was validated as a prognostic biomarker for ALS by Benatar et al. in a prospective, blinded, multicentre, longitudinal observational study of patients with ALS, primary lateral sclerosis and progressive muscular atrophy that demonstrated baseline plasma NfL in patients with symptomatic ALS and predicted ALSFRS-R slope and survival, and the study suggested that this biomarker may have application as a pharmacodynamic marker of treatment effects.48 As mentioned above, these data lend additional support to the utility of NfL as a prognostic biomarker that more reliably predicts the rate of disease progression in ALS compared with delta ALSFRS-R, which is similar to the findings in the post hoc analysis of the VALOR trial. These studies by Benatar et al. laid the groundwork for an ongoing phase III, multicentre, international, double-blind, randomized, placebo-controlled trial called ATLAS (ClinicalTrials.gov identifier: NCT04856982), evaluating the use of tofersen in clinically pre-symptomatic carriers of highly penetrant SOD1 mutations associated with rapid disease progression.51 While plasma neurofilaments represent a promising set of biomarkers for SOD1-ALS and likely C9orf72-ALS, their utility as pre-symptomatic biomarkers for other forms of ALS remains to be determined.
Future questions in the SOD1-ALS field that may also apply to ALS more broadly include how else SOD1 can be reduced, such as with adeno-associated virus (AAV) vectors, combination therapy that may act synergistically with tofersen or alternative routes of drug delivery. Mueller et al. tried an AAV approach to SOD1 knockdown in two patients; however, SOD1 levels were not effectively lowered and one of the two patients developed a meningoradiculitis.52 CRISPR technology or other gene editing may also offer therapeutic benefits in SOD1 and other genetic forms of ALS. Future studies of tofersen may even include an evaluation of tofersen efficacy in the broader sporadic ALS population, based on some studies demonstrating the presence of SOD1 aggregates in the tissue from patients with ALS without pathogenic mutations in SOD1.53,54
Further investigation into novel biomarkers will also augment our ability to design effective clinical trials and track clinical responses to novel therapeutics. As alluded to above, while NfL has proven to be a useful biomarker, other biomarkers that can identify disease at the earliest stages and can be tracked in response to treatment are needed. Mielke et al. recently published a study investigating a CSF RT-QuIC assay for SOD1 aggregation that could potentially be used as a screen to identify patients with ALS who may demonstrate a better response to tofersen.53 This study demonstrated that SOD1 seeding activity occurred in the motor cortex and spinal cords of patients with SOD1-ALS, C9orf72-ALS and sporadic ALS, suggesting that targeting SOD1 even beyond the SOD1-ALS population may hold therapeutic promise.
Conclusions
Since the discovery of the relationship between SOD1 mutations and fALS, SOD1-ALS has been extensively investigated to improve understanding of SOD1-ALS and sALS pathogenesis. This has allowed the field to move in the direction of more rational/targeted molecular therapeutics. The work being done in parallel to identify neurofilaments as reliable biomarkers of neurodegeneration in ALS has also been integral to this effort. The combined efforts of patients, family members, clinicians and researchers invested in changing the course of SOD1-ALS culminated in the accelerated FDA approval of tofersen for SOD1-ALS in 2023. No drug to date in the history of ALS has been shown to decrease neurodegeneration as robustly as tofersen, and the discovery of NfL as a reliable biomarker of neurodegeneration in ALS is opening new avenues to measure the success of novel therapeutics in the field. The SOD1-ALS story has given hope to the field and even inspired a new generation of ALS investigation looking into optimal rehabilitation for patients with ALS who can be stabilized with treatments such as tofersen (The effects of rehabilitation on functional outcomes in patients with SOD1 ALS treated with tofersen; ClinicalTrials.gov identifier: NCT05725759). Despite disappointing outcomes for other ASO therapeutics in the field, including ASOs targeting the expanded sense transcript in C9orf72 and one targeting ATXN2, the early success of tofersen and encouraging anecdotal reports from other efforts now in phase III studies (e.g. FUS) have undoubtedly established a new era in ALS therapeutics and forced many experts to rethink and recalibrate their approach to trial design in the hope of identifying additional therapeutic interventions to make ALS a livable disease for a larger percentage of patients in the not too distant future.