Posterior reversible encephalopathy syndrome (PRES) is a syndome characterized by a combination of clinical and radiological features.1–3 Its global incidence is unknown. It is underdiagnosed probably due to limited awareness. PRES presents with the rapid onset of neurological symptoms, such as headache, convulsion, altered consciousness and visual disturbance. Computed tomography (CT) and magnetic resonance imaging (MRI) findings of PRES are focal/patchy symmetrical vasogenic cerebral oedema, typically involving the posterior area of the brain.1–3 PRES has a wide array of aetiologies, such as hypertension, several autoimmune disorders, preeclampsia, immunosuppressive medication and renal failure.1–3 The pathophysiology of PRES is not yet clearly understood.4 It is hypothesized that PRES is caused by severe hypertension that causes dysregulation of cerebral vessels.5,6 Another theory suggests that it is caused by endothelial injury of cerebral vessels caused by inflammatory mediators in patients with autoimmune diseases.5,6 If PRES is recognized and treated early, it has a good prognosis. The clinical symptoms and changes seen in imaging usually resolve completely within days or weeks. However, if not treated and diagnosed properly, patients with PRES will have irreversible neurological deficits.7–9 We present a patient who had PRES associated with SLE and hypertension. This study aims to provide information for the early diagnosis and management of PRES in patients with SLE.
Case report
A 24-year-old woman presented to the emergency department with an acute severe headache and visual disturbance. Two years earlier, she had been diagnosed with systemic lupus erythematosus (SLE) and hypertension. She took azathioprine and methylprednisolone regularly for the treatment of SLE. She also took nifedipine and ramipril for hypertension.
At presentation to the emergency department, the patient had had a severe headache for 2 days, which had become unbearable and was suddenly accompanied by visual blindness. She also felt nauseous and had vomited twice that day. She reported that she often had headaches but never this severe and that this was the first time she had experienced visual blindness.
She was fully awake with normal orientation. Her initial blood pressure was 170/100 mmHg. She described that the pain intensity of her headache was 10/10 on the visual analog scale. Her visual acuity was 1/∞ (light perception only). On neurological examination, her cerebellar, motoric and sensory and other neurological functions were normal. No abnormality was found in her other cranial nerves; only her visual acuity was abnormal. Her pupillary light reflex was normal. She was treated symptomatically with intravenous paracetamol for the headache and ondansetron for nausea. She was also given amlodipine 10 mg in addition to her usual antihypertensive drugs. She was then admitted to the hospital. Our differential diagnosis at this time included neurogenic complications from SLE or space-occupying lesion compressing the optic chiasm.
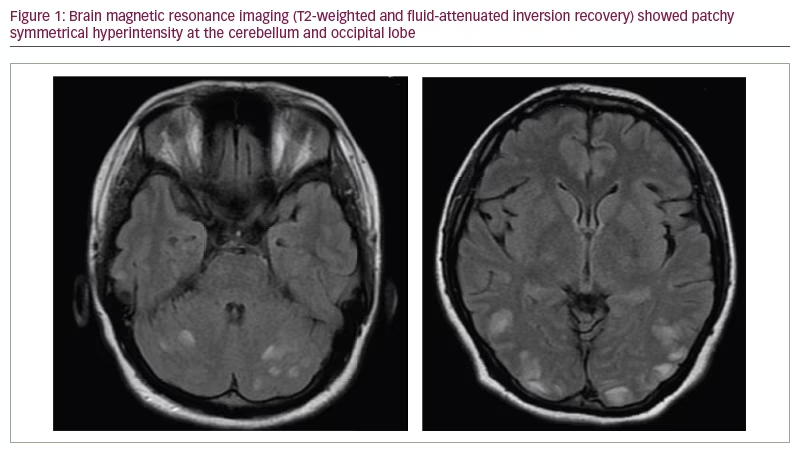
Routine laboratory workup and non-contrast brain MRI examination were obtained. Brain T2-weighted fluid-attenuated inversion recovery (FLAIR) MRI showed multiple hyperintensity patches at the occipital lobe and cerebellum; these findings suggested a diagnosis of PRES (Figure 1). PRES is not regularly treated using corticosteroids, and sometimes, immunosuppressive medicine can precipitate PRES. However, we treated the patient with intravenous methylprednisolone owing to the suspicion that her PRES was related to SLE disease activity. Her blood pressure was maintained using a combination of oral antihypertensive drugs (ramipril 2.5 mg and nifedipine extended release 30 mg). On the day after drug administration, her systolic blood pressure
was around 140–150 mmHg, and her diastolic blood pressure was 90–95 mmHg. She was also treated with intravenous phenytoin for seizure prophylaxis.
On day 1 after admission, the patient’s symptoms and visual acuity had improved. We observed her for two more days, and methylprednisolone treatment was continued and tapered down. Her blood pressure was around 130–140/80–90 mmHg. After two days, her symptoms had gone completely, and her visual acuity returned to normal. No seizure event occurred during the treatment. She was discharged without any neurological sequelae. Her oral antihypertensive drugs and immunosuppressive treatment were continued. She was given oral phenytoin for 1 week after being discharged before it was discontinued. By 1 month after discharge, she took her medications daily without any side effects. We did not observe any neurological deficit or any SLE
flare-up events.
Discussion
PRES was first described in 1996 in a case series reporting patients with reversible neurological symptoms and white matter abnormality on neuroimaging using CT or MRI.10 These patients had risk factors such as hypertension, renal failure and immunosuppressive treatment.
PRES is found predominantly in women, probably due to the fact that the aetiological aspects of PRES are sex specific.9 It is most frequently found in middle-age patients, although it can present across all age groups. A previous study of patients hospitalized with PRES showed that PRES mostly affected women (71.7%), 87.0% of patients had hypertension and 45.5% had hypertensive crisis.11 In another study, patients with PRES mostly presented with seizures (74.0%), encephalopathy (28.0%), headache (26.0%) and visual disturbances (20.0%), and 45.0% of patients had autoimmune diseases, including thrombotic thrombocytopenic purpura and SLE.9 Our patient had SLE and hypertension as risk factors. She also presented with acute visual disturbance and severe headache. Occipital lobe oedema may cause visual disturbance in PRES, although not every patient with PRES with occipital lobe involvement has visual disturbance.9
PRES pathophysiology is still not clearly understood. The most popular theory is that severe hypertension leads to cerebral vessel dysregulation and vasogenic oedema.6 Breakdown in autoregulation occurs when mean arterial pressure is above 150–160 mmHg.6 However, this theory does not explain why there are patients with PRES who are normotensive or whose mean arterial pressure does not reach 150 mmHg.12 The other theory proposes endothelial dysfunction, which results in a dysregulated autoregulatory response of cerebral vessels.13,14 Endothelial dysfunction may be caused by autoimmune diseases, serious inflammation, anti-neoplastic drugs and some immunosuppressive agents.13,14 Our patient had SLE, which might cause dysregulation of cerebral vessels and be further aggravated by hypertension.
Brain imaging is the cornerstone in diagnosing PRES and ruling out other diagnoses. Non-contrast CT scan can visualize vasogenic oedema, but MRI, especially the T2-weighted and FLAIR sequences, is definitely the superior imaging modality.15 Radiological abnormalities in PRES consist of patchy bilateral hyperintense signals on T2- and FLAIR-weighted MRI in the parieto-occipital lobes. These areas are frequently hypointense on CT scans or T1-weighted MRI.16 The most commonly affected areas are the parietal and occipital lobes, followed by the frontal lobes, the inferior temporo-occipital junction and the cerebellum.4 This radiological abnormality usually completely reverses if treated accordingly.4 Parieto-occipital regions are more commonly affected due to fewer sympathetic innervations of vessels that originate from the vertebrobasilar circulation compared with anterior circulation.17,18 Cerebellar oedema is usually found in patients with a history of autoimmunity.9 Indeed, our patient also had cerebellar involvement as well as a history of SLE.
There are no specific guidelines for the treatment of PRES. Identifying and managing its underlying aetiology and treating hypertension is essential for PRES management.19,20 Furthermore, there is no established guideline for the treatment of acute hypertension in PRES.21 Treatment is recommended when the blood pressure equals or exceeds 160 mmHg and 110 mmHg with a goal of 130–150 mmHg and 80–100 mmHg for systolic blood pressure and diastolic blood pressure, respectively.22 Blood pressure should not be reduced drastically because it can lead to brain ischaemia and hypoperfusion. A reduction in blood pressure of 10–20 mmHg every 20 minutes is recommended. Intravenous antihypertensive drugs may be used for blood pressure reduction when patients have a hypertensive crisis (>180/120 mmHg).22,23
In our patient, the underlying aetiology, other than hypertension, was SLE. There is still controversy about whether immunosuppressive agents should be used in the treatment of PRES with SLE because some PRES cases are caused by immunosuppressive medication (such as corticosteroids and cyclosporine), and it is usually advised to withdraw the medications.24,25 However, SLE-related PRES has also been observed in patients with SLE that are treatment-naïve.24,25 PRES observed in normotensive patients and in treatment-naïve patients may suggest that endothelial dysfunction due to SLE plays an important pathogenetic role.23,24 It might, therefore, be reasonable to use steroids for SLE-related PRES due to this pathophysiology.24,25 Some studies have observed patients with SLE-related PRES who have been treated with high-dose corticosteroids combined with other immunosuppressive medications, and most of the patients showed complete clinico-radiographic recovery after the treatment.19,24 Nevertheless, controversy remains about the usage and indication of immunosuppressive medications in the treatment of PRES in SLE. Randomized controlled trials should be performed to establish the usage and indication of immunosuppressive treatment in PRES and SLE.
Our patient was also given phenytoin for seizure prophylaxis. Seizures are a common manifestation of the acute onset of PRES. However, no guidelines exist regarding the prophylactic use of antiepileptic drugs in the acute onset of PRES.26 A study in India observed that the most common antiepileptic drugs used in PRES are phenytoin, carbamazepine and levetiracetam.24 Unprovoked seizures are uncommon after patient symptoms have resolved, and after PRES symptoms and risk factors have been controlled, antiepileptic drugs should be discontinued.27
PRES is reversible when treated promptly, but delay in diagnosis and treatment may cause death and irreversible neurological sequelae. Mortality in patients with PRES is reported to be around 13%,28 and 10–20% of them may have residual neurological symptoms.29,30 However, in a case study from India, the mortality was 7%, and 93% of patients were discharged without any neurological deficit.31
Limitations
PRES has a wide array of differential diagnoses, such as reversible vasoconstriction syndrome and cerebral vasculitis, which can be detected using angiography and several laboratory studies. As our patient responded well to treatment, and owing to financial limitations, we did not perform angiography or further workup. Symptoms and radiological findings in patients with PRES are usually completely reversed with treatment. In this case report, our patient’s symptoms completely resolved, but we did not repeat the MRI examination because of financial limitations.
Conclusion
PRES is a clinical syndrome with specific imaging findings. The diagnosis of PRES requires thorough clinical and neuroimaging examinations. Clinical suspicion of PRES must be high, especially in patients with pre-existing risk factors. Identifying its underlying cause and prompt diagnosis and treatment is important for achieving a better outcome and minimizing neurological sequelae or mortality in patients with PRES.
Minor post publication correction: Compliance with ethics statement updated.