The options available for treating multiple sclerosis (MS) have increased substantially over the last two decades. Initial first-line disease-modifying therapies (DMTs), included intramuscular (IM) interferon (IFN) β-1a (Avonex®, Biogen, Cambridge, Massachusetts, US), subcutaneous (SC) IFN β-1a (Rebif®, EMD Serono, Rockland, Massachusetts, US), SC IFN β-1b (Betaferon®, Bayer, Leverkusen, Germany; Extavia®, Novartis, Basel, Switzerland [2007]) and SC glatiramer acetate [GA] (Copaxone®, Teva Neuroscience, Petah Tikva, Israel). Mitoxantrone and later natalizumab, both high efficacy treatments, were generally used second-line.1–7 Although moderately efficacious, patient adherence to IFNs and GA was and remains an important challenge despite innovations in the formulation and delivery of these DMTs.8,9 Further, some patients with MS develop neutralising antibodies (NAbs) when treated with IFN-β, which abrogates the therapeutic efficacy.10 Poor adherence to these DMTs has been shown to result in a reduction in efficacy and in worse patient outcomes.11
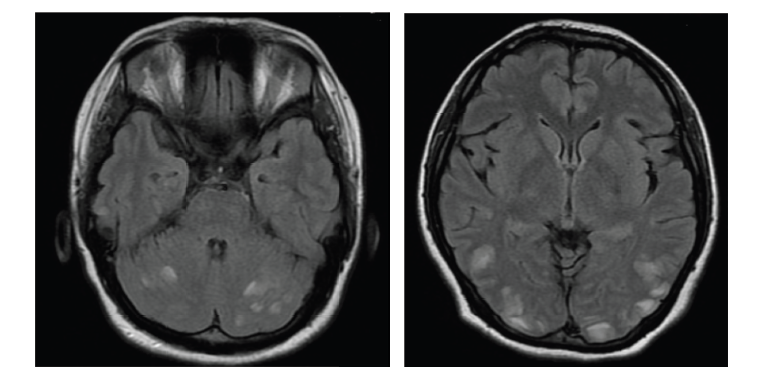
It is common practice in some countries for physicians to prescribe several first-line therapies such as IFN β-1a or GA before switching to monoclonal antibodies.12 However, there is growing evidence that, in addition to the early initiation of treatment after diagnosis,13 early treatment optimisation after insufficient response to initial treatment is important to achieve a favourable outcome.14 Recently, a new strategy has emerged, ‘treating to target,’ where the aim is to achieve no evidence of disease activity (NEDA). This composite measure is defined as no relapse activity, no Expanded Disability Status Scale (EDSS) disability progression, and no new magnetic resonance imaging (MRI) lesions (T1 Gd+ and/or active T2 lesions).15–17 Confirming NEDA necessitates regular monitoring of relapses, disability and for subclinical activity on MRI.18 There is a report from a study of 152 patients indicating that the monoclonal antibody, natalizumab, is associated with a higher proportion of patients achieving NEDA status compared with those reported previously for injectable treatments.19
Monoclonal antibodies are used therapeutically in a variety of medical disciplines including oncology, rheumatology, gastroenterology, dermatology and prevention of transplant rejection. Three monoclonal antibody treatments are currently approved for treating MS, (natalizumab,20–24 alemtuzumab25–30 and daclizumab31). These are high efficacy treatments but tend to be reserved for more active patients, in particular in patients with rapidly-evolving severe MS (Table 1). Other humanised monoclonal antibodies are currently in advanced development (Phase II and III) mainly in the treatment of patients with relapsing-remitting MS (RRMS). These include ocrelizumab,32,33 ofatumumab (both anti-CD20)34,35 and opicinumab (anti-LINGO-1).36

The anti-CD20 monoclonal antibody, rituximab,37 was in development and despite being very effective in phase II the development programme was terminated due to issues linked to immunogenicity, due to it only being partially humanised, and its imminent patent expiry. Two further monoclonal antibodies, tocilizumab38,39 and eculizumab,40,41 are in development for neuromyelitis optica, which although often misdiagnosed as MS has a different pathogenesis. Table 1 gives a summary of the monoclonal antibodies currently in Phases I, II and III.
Monoclonal antibodies have distinct structural characteristics (e.g. chimeric, humanised, fully human) and different targets, including blocking interactions, cross-linking, induction of signal transduction by receptor binding, complement-dependent cytotoxicity, antibodydependent cell-mediated cytotoxicity. These confer various and different mechanisms of action in MS (Table 1).
Monoclonal antibodies and the implications for therapy
Monoclonal antibodies are potentially advantageous for the treatment of MS in that they are designed to be very specific in terms of their relevant target and unlike small molecules have very few off-target effects.42 Many monoclonal antibodies can also be given over an initial short period and then patients do not necessarily need to receive any further doses for 6 months or longer, e.g. ocrelizumab and alemtuzumab. In contrast, the injectable and oral DMTs for MS require long-term, frequent (often daily) administration.7,43,44
Monoclonal antibodies for MS cannot be considered a single class of treatments given the multiplicity of targets and wide spectrum of benefit–risk profiles. Immunogenicity profiles and effector functions likewise vary considerably with antibody type. When choosing an appropriate treatment, careful consideration must be made of the many unique characteristics of each monoclonal antibody therapy, especially, rare serious adverse events and uncertainties about long-term safety.
Some monoclonal antibody treatments have serious safety concerns, which may discourage their use in many patients and may limit their use as first-line therapies.45,46 Diligent monitoring of patients (for conditions such as John Cunningham virus [JCV]/progressive multifocal leukoencephalopathy [PML] with natalizumab), however, has been shown to reduce the risk of serious adverse events in those receiving monoclonal antibodies.47 Certain treatment-related complications may not become apparent until monoclonals are more widely prescribed, as exemplified with natalizumab and the association with PML. Currently a strategy is available to help predict which individual patients may develop PML;47 four major risk factors have been identified: JCV sero-positivity, a high antibody index against JCV, the prior use of immunosuppressants and a treatment duration with natalizumab of 2 years or more. The TYSABRI Outreach: Unified Commitment to Health (TOUCH) Prescribing Program is in place to inform prescribers, infusion centre healthcare providers, and patients about the risk of PML associated with natalizumab, including the increased risk of PML with treatment duration and prior immunosuppressant use. The program also seeks to warn against concurrent use with anti-neoplastic, immunosuppressant, or immunomodulating agents and in patients who are immunocompromised and promote early diagnosis of PML and timely discontinuation of natalizumab in the event of suspected PML.
The benefit–risk profiles of these monoclonal antibody treatments therefore need to be carefully considered and understood before using them.48 Further, review of clinical efficacy and safety results are needed as well as consideration that the clinical trials of monoclonal antibodies have been evaluated using different methods and comparators and in different patient populations. The treatment of MS requires a consistent policy to be developed;49 unfortunately, patients currently have variable access to effective treatments. This is likely to become an increasingly pressing issue, especially as new therapies become available. Screening and monitoring is required to enable the optimal use of monoclonal antibodies to improve treatment outcomes for patients with MS.
Natalizumab
In a randomised, double-blind trial, 213 patients with relapsing remitting or relapsing secondary progressive MS to receive 3 mg of intravenous natalizumab/kg of body weight (n=68), 6 mg/kg (n=74) or placebo (n=71) every 28 days for 6 months.50 The mean number of new lesions was significantly reduced in both natalizumab groups (9.6 per patient in the placebo group versus 0.7 in the group given 3 mg of natalizumab per kg (p<0.001) and 1.1 in the 6 mg natalizumab per kg group (p<0.001). In addition, 27 patients who received placebo relapsed versus 13 and 14 in the 3 mg natalizumab per kg and 6 mg natalizumab (p=0.02). In the randomised, placebo-controlled trial, Natalizumab Safety and Efficacy in Relapsing Remitting Multiple Sclerosis (AFFIRM; n=942), natalizumab reduced both the risk of the sustained progression of disability and the rate of clinical relapsed in patients with relapsing MS (RMS) versus placebo.51 Over 2 years, natalizumab treatment reduced the risk of sustained disability progression by 42% (hazard ratio, 0.58; 95% confidence interval [CI], 0.43 to 0.77; p<0.001) and the rate of clinical relapse at 1 year was reduced by 68% (p<0.001) versus placebo. Natalizumab also demonstrated a sustained effect in the prevention of new lesion formation in this trial.52 Sub-group analysis was performed for patients who had experienced two or more relapses in the prior year and also had at least one gadolinium-enhancing lesion on brain MRI or a significant increase in T2 lesion load when compared with a previous

recent MRI.53 The Tysabri (natalizumab) Observational Program is an open-label, multinational, 10-year prospective study in clinical practice settings. Interim, 5-year results have confirmed the overall safety profile of natalizumab and the low relapse rate and stabilised disability levels in natalizumab-treated patients with RRMS in clinical practice.54
Alemtuzumab
In the International Campath-1H in Multiple Sclerosis (CAMMS223) trial, in 334 patients with early RRMS, alemtuzumab significantly reduced the rate of sustained accumulation of disability, compared with IFN β-1a (9.0% versus 26.2%; hazard ratio, 0.29; 95% CI, 0.16 to 0.54; p<0.001). In the alemtuzumab group compared with the IFN β-1a group, adverse events included autoimmunity (thyroid disorders [23% versus 3%] and immune thrombocytopenic purpura [3% versus 1%]) and infections (66% versus 47%).55
Of 334 patients originally randomised in the CAMMS223 trial, 198 participated in the extension phase (151 [68%] alemtuzumab and 47 [42%] IFN β-1a).56 At 5-year follow-up of CAMMS223 clinical trial, alemtuzumab versus IFN β-1a reduced both the risk of sustained disability accumulation and the rate of relapse by 72% and 69%, respectively (both p<0.0001).
In the 2 year, rater-masked, randomised, controlled phase III trial, Comparison of Alemtuzumab and Rebif® Efficacy in Multiple Sclerosis, Study One (CARE-MS I) (n=386), 75 (40%) patients treated with IFN β-1a relapsed (122 events) compared with 82 (22%) patients who were treated alemtuzumab (119 events; rate ratio 0.45 [95% CI 0.32–0.63]; p<0.0001).57 However, no benefit was observed in respect of disability endpoints. CARE-MS II, was also a 2 year, rater-masked, randomised, controlled phase III trial, with 667 RRMS patients and at least one relapse on IFN β or GA.58 In total, 104 (51%) patients treated with IFN β-1a relapsed (201 events), compared with 147 (35%) patients in the alemtuzumab group (236 events; rate ratio 0.51 [95% CI 0.39–0.65]; p<0.0001), representing a 49.4% improvement with alemtuzumab. In addition, 40 (20%) patients treated with IFN β-1a had sustained accumulation of disability compared with 54 (13%) of those treated with alemtuzumab (hazard ratio 0.58 [95% CI 0.38–0.87]; p=0.008). This corresponded to a 42% improvement in the alemtuzumab group. Common adverse events of alemtuzumab include infusion-related reactions, which are generally mild and short-lived, and increased risk of infections following a treatment course.59 Potentially very serious side effects may also occur including thyroid disorders, kidney problems and blood clotting problems.

Daclizumab
Daclizumab high yield process (HYP) demonstrated clinically important effects on disease activity in during 1 year of treatment versus placebo in patients with RRMS in the Daclizumab high-yield process in relapsing– remitting multiple sclerosis (SELECT) study.60 Improvements versus placebo were also reported on health-related quality of life61 and disease-activity-free status.62 five hundred and seventeen (91%) of 567 patients who completed the SELECT trial entered Daclizumab high-yield process in relapsing-remitting multiple sclerosis (SELECTION), a 52-week extension study which aimed to assess the safety and immunogenicity of extended treatment with daclizumab HYP.63 Adverse events and immunogenicity were not increased in the second year of continuous treatment with daclizumab HYP or during treatment washout and reinitiation. In the Efficacy and Safety of BIIB019 (Daclizumab High Yield Process) Versus Interferon β 1a in Participants With Relapsing-Remitting Multiple Sclerosis (DECIDE) study, daclizumab has demonstrated superior efficacy compared with IFN β-1a across several MS outcome measures in RMS patients.31 Treatment with daclizumab compared with IFN β-1a resulted in a 45% reduction in the annualised relapse rate (p<0.001) although the percentage of patients who relapsed did not differ significantly between the daclizumab and IFN β-1a group (51% versus 67%, respectively). There was a 54% reduction in the number of new/ enlarging T2 hyperintense lesions at week 96 for daclizumab versus IFN β-1a (p<0.0001). In addition, an increased incidence was seen in the daclizumab-treated group versus IFN β-1a in serious infections (4% versus 2%), serious cutaneous events (2% versus 1%), and alanine transaminase (ALT) or aspartate aminotransferase (AST) elevations (>5x upper limit of normal) 6% versus 3%.31 No treatment-related deaths occurred and there was no evidence of an increased risk of malignancies versus IFN β-1a. The most common adverse events associated with daclizumab are elevations of liver enzymes and hepatic injury, cutaneous events, infections, gastrointestinal disorders and depression.64
Ocrelizumab
In a phase II, randomised, placebo-controlled, multicentre trial, patients with RRMM were assigned to either placebo, low-dose (600 mg) or highdose (2000 mg) ocrelizumab given as two doses on days 1 and 15, or IM IFN β-1a (30 μg) once a week.33 At 24 weeks, the number of Gd-enhancing lesions was 89% lower in the 600 mg ocrelizumab group compared with the placebo group (95% CI 68–97; p<0.0001), and 96% lower in the 2000 mg ocrelizumab group (95% CI 89–99; p<0.0001).
OPERA I and II are two identical Phase III, multicentre, randomised, double-blind, double-dummy, parallel-group trials aiming to assess the efficacy and safety of ocrelizumab (n=821) versus IFN β-1a (n=835) in patients with relapsing forms of MS.65 Ocrelizumab significantly reduced annualised relapse rate, the primary endpoint (Figure 1). Another Phase III trial, ORATORIO, has assessed the efficacy and safety of ocrelizumab versus placebo in patients with primary progressive MS. Initial analysis has revealed that, compared with placebo, ocrelizumab gave a statistically significant reduction in confirmed disability progression at 12 weeks (Figure 2).66 A similar reduction was seen in the secondary endpoint of confirmed disability progression at 24-weeks. Overall, the safety profile over the controlled treatment periods for the Phase III trials in RMS and primary progressive MS was favourable in comparison with IFN β-1a or placebo.
Opicinumab
Leucine rich repeat and Immunoglobin-like domain-containing protein 1 (LINGO-1) is a cell surface glycoprotein specific to the central nervous system67,68 that suppresses oligodendrocyte differentiation and myelination.69,70 Opicinumab (also known as BIIB033 or anti-LINGO-1) is a potential first-in-class fully human monoclonal antibody that is antagonistic to LINGO-1. Data from a preclinical study in rats suggest that blocking LINGO-1 with opicinumab leads to axonal protection during acute optic nerve injury.36 An international phase II study (RENEW) investigated the efficacy of opicinumab in participants with their first episode of acute optic nervitis (ClinicalTrials.gov identifier: NCT01721161). In addition, a phase II study is in progress to evaluate the efficacy, safety and tolerability of opicinumab in patients with active relapsing MS when used concurrently with IFN β-1a (ClinicalTrials.gov Identifier: NCT01864148).
Conclusions
Over the past decade there has been an ongoing tremendous evolution of novel, monoclonal antibody treatment options for MS. However, improved options for the treatment of secondary progressive MS remains an important unmet need. Results for ocrelizumab and other anti-CD20 B cell-depleting monoclonal antibodies for the treatment of relapsing MS have shown promising effects especially on MRI measures of MS disease activity. Results of phase III studies will help determine the place of ocrelizumab in the current armamentarium of MS therapies. Safety issues such as infusion reactions may be mitigated by pre-treatment with corticosteroids in addition to symptomatic management with antihistamines. Post-marketing Risk, Evaluation and Mitigation Strategies (REMS) are needed so that potential adverse events can be identified and managed early and effectively.71 No treatment has as yet been proven to be effective for myelin repair or neuro-regeneration in MS although progress in understanding MS pathology and biotechnological advances will continue to provide hope that this long standing challenge may be met in the future.