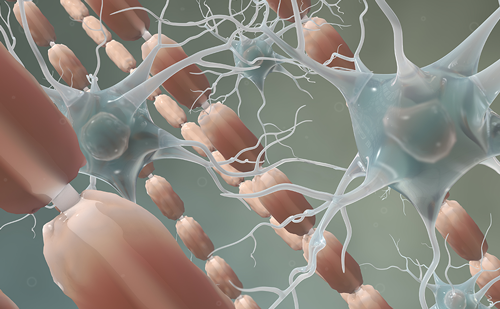
T and B cells in multiple sclerosis immunopathology
Knowledge of multiple sclerosis (MS) pathophysiology has progressed dramatically from the first description of the disease in 1868 to the understanding of immune processes in the 1990s to the present day. Genetic1,2 and environmental3 factors contribute to MS and cause an imbalance in immune regulatory networks comprising both T and B cells.4–6 In MS, the balance of T cell subtypes and responses is skewed. CD4+ naïve T cells differentiate into different cell types.
• The number of Th17 cells is increased.7
• In the central nervous system (CNS), microglial cells produce pro-inflammatory cytokines such as tumour necrosis factor (TNF)-α, and cytotoxic substances such as reactive oxygen species and reactive nitrogen species that lead to neuro-inflammation and the direct destruction of neurons.8
• CD8 ‘killer’ T cells destroy axons; membrane damage in major histocompatibility complex class I restricted neurons by CD8+ T cells suggest granule-mediated death.9–11
• Interleukin (IL)-10 producers including CD4+, CD25+ and regulatory T cells (Tregs) are able to suppress inflammation. Tregs normally act to inhibit autoreactive cells. Numbers and functional capacity of Treg cells is impaired in patients with relapsing-remitting MS (RRMS),8,12 which allows autoreactive T cells to induce CNS damage.
B cells are potent antigen-presenting cells that can contribute to the pathogenesis of MS via cytokine production, antigen presentation and formation of autoantibodies.1,13 High levels of CD80 (B7-1) antigens on the surface of B cells permit them to activate antigen-specific cells.14 T and B cells form clusters which lead to immune activation and the formation of adaptive memory. B cells can activate autoreactive T cells. Large B cell aggregates comprising T cells and plasma cells can form in the inflamed cerebral meninges of secondary progressive MS (SPMS) patients.15 It is difficult to eliminate cell clusters behind the blood–brain barrier, which may explain disease progression in patients with SPMS. In MS there are complex cellular networks that drive and dampen disease pathophysiology (see Figure 1). The interactions between T and B cells provide multiple targets for MS treatments. A preferred approach in MS therapy, therefore, is to target more than one component.1,12,16–22


There are many approaches to targeting lymphocytes in MS, including modulating activated lymphocyte proliferation,23 decreasing lymphocytes by selective depletion followed by chronic depletion or repopulation24 and interfering with lymphocyte trafficking.25 Since both T and B cells, and also the interaction between them, contribute to MS pathophysiology, upstream targeting of both cell types directly is a rational therapeutic approach.1,5,21,26 This article aims to summarise the targeting of both T and B cells as a treatment approach in MS, with a focus on alemtuzumab (Lemtrada®, Genzyme, UK).
Targeting T and B cells for durability of effect
Alemtuzumab – a unique mode of action
Alemtuzumab is a recombinant humanised immunoglobulin G1 (IgG1) monoclonal antibody that selectively targets CD52, which is a protein of unknown function that is abundant on the surface of both B (CD19+) and T (CD3+) lymphocytes.27 Innate immune cells, however, express lower levels of CD52 and so are minimally or transiently affected by alemtuzumab treatment.28,29 Alemtuzumab has been approved for the treatment of RRMS in more than 40 countries, including the EU in 201328 and the US in 2014.30 It is administered intravenously in two annual courses: 12 mg/day given on five consecutive days at the initiation of treatment, and 12 mg/day on three consecutive days, 12 months later.28,30
The mechanism by which alemtuzumab exerts its therapeutic benefits in MS has not yet been elucidated fully. Research does suggest, however, that the drug’s immunomodulatory effects can be explained though depletion and repopulation of lymphocytes.24,31 This may reduce the potential for relapse, ultimately delaying the disease progression. Alemtuzumab depletes T and B lymphocytes primarily via antibodydependent cytolysis and complement-dependent cytolysis (see Figure 2).27,32 Remaining lymphocytes retain normal function, and there appears to be minimal impact on the development of immune responses; owing to the spared immune system, the response to pathogenic organisms is relatively intact. This has been demonstrated in human CD52 transgenic mice.29
CD4+ and CD8+ T cells and CD19 B cells initially decrease after a dose of alemtuzumab, but increase over the following 11 months.33,34 The rate of lymphocyte reconstitution differs among the subsets;35 selectively delayed CD4(+) T cell repopulation following alemtuzumab-induced lympopenia may contribute to alemtuzumab’s long-lasting suppression of disease activity.36 During repopulation after alemtuzumab treatment, there is a shift in the relative proportions of T cell and B cell subsets.29,31 Proportions of regulatory T cells and memory-phenotype T cells are increased, whereas the proportion of naïve T cells is decreased.31,36 The proportion of B cells of a mature naïve phenotype also reduces after alemtuzumab treatment, whereas the immature cell fraction is increased.31 The differential reconstruction may contribute to extended efficacy of alemtuzumab in MS without increasing the risk of infection.36 There are, in addition, alterations in the cytokine profile, which include substantial decreases in IL-17 and in cytokines that promote IL-17, such as IL-21 and IL-23.36
Targeting T and B cells to optimise multiple sclerosis treatment strategies – alemtuzumab
The clinical development of alemtuzumab includes a phase II (CAMMS223; NCT00050778)37 and two large phase III studies (CARE-MS I; NCT0053034838 and CARE-MS II; NCT NCT0054840539) versus an active comparator, (high-dose interferon beta-1a [IFNβ-1a (44 mg)]), and an extension study (NCT00930553).40,41 In CAMMS223, CARE-MS I and CARE-MS II, the demographics and baseline characteristics were balanced between the patient group who received 12 mg alemtuzumab treatment courses and the group who received the comparator treatment, high-dose subcutaneous IFNβ-1a three-times weekly. The primary endpoints were annualised relapse rates (ARR) and sustained accumulation of disability (SAD).37
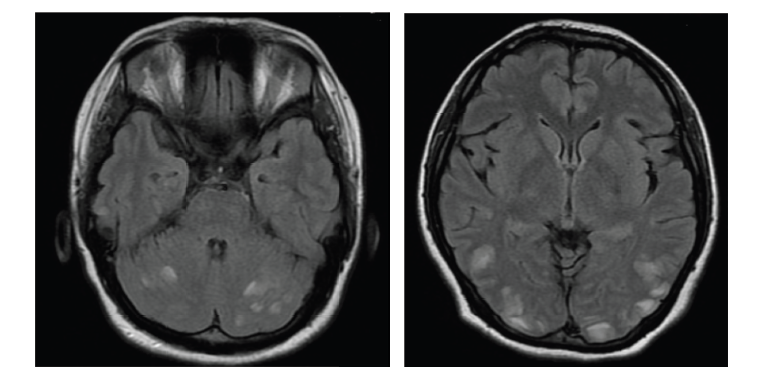
In the CAMMS223 study in patients with early RRMS (n=334), alemtuzumab was associated with a significant reduction in the rate of SAD, when compared with IFNβ-1a (9.0% versus 26.2%; hazard ratio, 0.29; 95% confidence interval [CI], 0.16–0.54; p<0.001) and the ARR (0.10 versus 0.36; hazard ratio, 0.26; 95% CI, 0.16–0.41; p<0.001).37 The mean disability score, measured on a 10-point scale, improved by 0.39 points in the alemtuzumab group. In contrast, this score worsened by 0.38 points in the IFNβ-1a group (p<0.001). The lesion burden, as assessed on T(2)-weighted magnetic resonance imaging, was reduced in the alemtuzumab group when compared with that in the IFNβ-1a group (p=0.005). From Month 12 to 36, brain volume (BV) on T(1)-weighted magnetic resonance imaging (MRI) increased in the alemtuzumab group but decreased in the IFNβ-1a treatment group (p=0.02). Adverse events

(AEs) in the alemtuzumab group, versus the IFNβ-1a group, included autoimmunity (thyroid disorders [23% versus 3%, respectively] and immune thrombocytopenic purpura [3% versus 1%, respectively]) and infections (66% versus 47%, respectively). The CAMMS223 study was not powered to identify any uncommon AEs.37
The CARE-MS I study recruited only previously untreated patients with early RRMS; the CARE-MS II trial recruited only patients with RRMS and at least one relapse on IFNβ-1a or glatiramer acetate. In total, 187 (96%) of 195 patients who were randomly allocated IFNβ-1a and 376 (97%) of 386 patients randomly allocated alemtuzumab were included in the primary analyses. No treatment effect on the endpoint of reduced accumulation of disability was observed in CARE-MS I. Over 2 years, courses of alemtuzumab treatment resulted in 55% lower ARR (p<0.0001) and 30% lower six-month SAD (p=0.22) than IFNβ-1a (see Table 1). In addition, 78% of patients receiving alemtuzumab were relapse-free compared with 59% of patients receiving IFNβ-1a.38
In CARE-MS II, 202 (87%) of 231 patients allocated to IFNβ-1a and 426 (98%) of 436 patients allocated to alemtuzumab 12 mg were included in the primary analyses.39 Over 2 years, alemtuzumab resulted in 49% lower ARR (p<0.0001) and 42% lower 6-month SAD (p=0.0084) than IFNβ-1a (see Table 1). Further, 65% of patients receiving alemtuzumab were relapse-free compared with 47% receiving IFNβ-1a. Patients who had been treated with alemtuzumab were more than twice as likely to have disability improvement sustained over 6 months than those treated with IFNβ-1a.39 In both CARE-MS I and CARE-MS II, alemtuzumab also produced reductions in MRI disease activity (including change in T2 lesion volume, percentage of patients with Gadolinium (Gd)-enhancing lesions, new/enlarging T2 lesions, new T1 lesions, and percentage reduction in brain parenchymal fraction) over those observed with IFNβ-1a.38,39
Evaluating durability of effect with alemtuzumab
Of the 60 patients who entered the ongoing extension study to CAMMS223, 95% (57) remained on study at Year 10. A low ARR was maintained through 10 years of follow-up.43 In the ongoing CAREMS I and CARE-MS II extension study (NCT00930553), patients can receive retreatment at any time 12 months after the second course of alemtuzumab. Of patients treated with alemtuzumab or IFNβ-1a, 95% and 93%, respectively, enrolled in the extension study.44,45 Less than 2% of patients received other DMTs in Years 3 and 4 in CARE-MS I and, in


CARE-MS II, 5% of patients received other DMTs in Years 3 and 4.44,45 ARR was maintained at 0.15 and 0.18 in Year 5 in the CARE-MS I and II extension studies, respectively (Figure 3).46,47 After 5 years of alemtuzumab, 88% and 85% of patients previously in the CARE-MS I and II studies, respectively, were relapse-free.46,47 In addition, in pooled 5-year data for CARE-MS I and II, 73%, 72% and 69% of patients had no evidence of disease activity (NEDA) in Years 3, 4 and 5 of the extension study, respectively and over Years 3–5, 51% had sustained NEDA (see Figure 4).42 Durable efficacy in terms of NEDA was also shown in half the subgroup of patients who had highly active RRMS and an inadequate response to prior therapy in the 5-year follow-up of the CARE-MS II study.48 Highly active disease was defined as ≥2 relapses in the year prior to randomisation and ≥1 Gd-enhancing T1 lesion at core study baseline. In Year 5, among the subgroup of treatment-naive patients with highly active RRMS at baseline in CARE-MS I, NEDA was achieved by 61% of patients, and the majority were free from either clinical (84%) or MRI activity (67%).49
Reductions in ARR of 69% and 71% were observed in the first 2 years in patients who discontinued subcutaneous IFNβ-1a and switched to alemtuzumab in the CARE-MS I and CARE-MS II studies, respectively; these effects were maintained through the third year. In addition, 88% and 90% were free from relapse in Year 3 after switching.50,51 BV loss also slowed after discontinuing subcutaneous IFNβ-1a and switching to alemtuzumab in the CARE-MS I and CARE-MS II extension study.52 Median yearly BV loss in IFNβ-1a-treated patients in Year 2 in CARE-MS I (-0.50%) and CARE-MS II (-0.33%) was reduced in Years 1, 2 and 3 after switching to alemtuzumab (CARE-MS I: -0.07%, -0.13%, -0.09%; CARE-MS II: 0.02%, -0.05%, -0.14%).52
Reasons for durability of treatment effect with alemtuzumab
The long-lasting suppression of MS activity may be explained by a shift from a pro- to an anti-inflammatory phenotype and cytokine profile caused by alemtuzumab. These factors may underpin the sustained disability improvements seen in the clinical trials. Alemtuzumab depletes peripheral, circulating CD52+ cells whereas those in the bone marrow and thymus are unaffected.27 The delayed reconstitution of CD4+ cells or the effect of an altered immune repertoire following reconstitution may mediate alemtuzumab’s long-lasting clinical effect.32 The delay in CD4+ cell reconstitution is a result of deficient CD4+ cell homeostatic proliferation, susceptibility to apoptosis,53 and a relative expansion of immunoregulatory CD4+CD25+CD127low Treg, TGF-beta+, IL-10+, and IL- 4+CD4+ cells.32 Patients with RRMS subsequently exhibited expansion of TGF-β-, IL-10- and IL-4-secreting immunoregulatory CD4+ cells, followed by the suppression of Th1 and Th17 cells.32 Immune reconstitution following alemtuzumab treatment is also characterised by the relative expansion of Th2 cells.36,54
Strong evidence that alemtuzumab promotes neuro-repair is derived from post hoc analysis of the phase II CAMMS223 trial.55 Patients were examined who had been treated with either alemtuzumab or IFNβ-1a and had no clinical evidence for disease activity in the 3 months before treatment, or clinical and radiological disease activity evidence for 36 months thereafter. Patients in both treatment groups, who had been selected for maximal disease inactivity, seemed to share equal suppression of cerebral inflammatory activity. Each group of patients therefore had the same opportunity for endogenous repair, yet disability improvement was seen only after alemtuzumab treatment and not treatment with IFNβ-1a.55 Potential neuro-protective effects reported for alemtuzumab are the production of neurotrophic factors including increases in brain-derived neurotrophic factor, fibroblast growth factor, platelet-derived growth factor and ciliary neurotrophic factor.55 These bioactive, neurotrophic factors promote neuronal survival, axon growth and survival of oligodendrocytes in vitro.
Can treatment with alemtuzumab that involves depletion and repopulation of T and B cells provide a consistent safety profile?
Important side effects associated with alemtuzumab include: infusion reactions; hypersensitivity and immunogenicity; cytokine release syndrome; tumour lysis syndrome; immunosuppression and opportunistic, cytopaenias: pancytopaenia, lymphopaenia and thrombocytopaenia; autoimmune haemolytic anaemia; thyroid disorders and cardiotoxicity.56 A pooled analysis of the CARE-MS I and II studies and the CARE-MS I extension showed the effects of alemtuzumab on immunity.57 A steady decline was seen in the rate of infections from 59.4% in Year 1 to 42.1% in Year 5 and serious infections decreased from 1.8% to 1.3% from Year 1 to Year 5.57 Patients who developed infections had similar lymphocyte counts to those who did not.58 The most frequent treatment-related infections were: nasopharyngitis, urinary tract infection, upper respiratory tract infection, sinusitis, oral herpes, influenza and bronchitis.28 The most frequent AEs with alemtuzumab were infusion-associated reactions: immune-related AEs declined from 85% to 45% during the first to the fifth treatment.57 Most occur on the first day of the course and are mainly mild-to-moderate in severity. Anti-glomerular basement membrane (anti- GBM) disease and other nephropathies (glomerulonephritis with positive anti-GBM antibody and membranous glomerulonephritis) occurred in 0.3% (4/1,486) of patients in MS clinical trials and may occur months or years after alemtuzumab treatment.28 In CARE-MS I, II core and extension studies (1,322 patients in total), nephropathies were seen in 0.1% of patients in Year 3 and idiopathic thrombocytopenic purpura (ITP) was seen in 0.2–0.9% of patients over 5 years.41 The safety monitoring programme, which includes monthly complete blood counts and physician and patient education to recognise the signs and symptoms of ITP, affords opportunity for early detection and intervention, which may allow for the best patient outcomes.59 Monitoring for side effects and regular testing must continue for 4 years after the last infusion. Autoimmune thyroid AEs peaked in Year 3 (31.3 per 100 patient-years) and then declined in Years 4 (17.6%) and 5 (13.6%). Most were mild-tomoderate (Grade 1 or 2) in severity and the most frequently reported thyroid AEs were hypothyroidism, hyperthyroidism and Graves’ disease.60 During the CARE-MS extension study, the rate of malignancies at 2.4% did not differ from that seen during the core studies.61 In total, 1,486 patients in the extension had received 5 years of therapy, and cumulatively 8,266 years of follow-up. No meaningful trends in malignancies in terms of incidence or rate by number of treatment courses, years of follow-up, or cumulative alemtuzumab dose were observed. The most frequently occurring malignancy with alemtuzumab was of the thyroid, of which all were papillary and at Stage 1; the pooled rate of thyroid malignancy was 0.073/100 patient-years. Half (3/6) were microcarcinomas (<10 mm). Overall clinical trial evidence suggests that there is no increased risk of thyroid cancer with alemtuzumab. Ascertainment bias may have increased apparent frequency. This risk was not significantly different in comparison with a retrospective cohort of 32,348 patients with MS.61
There are no clinical studies of alemtuzumab in pregnant women; however, as MS is diagnosed frequently in women of childbearing age, data on pregnancy outcomes were collected as part of the safety followup of the CAMMS223, CARE-MS I and CARE-MS II extension.62 Out of the 181 completed pregnancies with known outcomes there were 122 (67.4%) live births. Both the spontaneous abortion risk (21.5%) and stillbirth rate (0.6%) in alemtuzumab-treated patients remains comparable to rates in the general population. To date, there has been no indication of increased rates of congenital abnormalities in women who became pregnant.62
Supportive evidence of neurorehabilitation with alemtuzumab – improving quality of life and reducing brain volume loss
The CARE-MS I and II studies showed that alemtuzumab substantially improves quality of life (QoL) measures. At all time points over 24 months during randomised treatment, alemtuzumab was associated with significantly improved Functional Assessment of Multiple Sclerosis (FAMS) scores compared with baseline and IFNβ-1a treatment (both p<0.05 to <0.0001).63.64 Sustained reduction in disability (SRD) had a significant effect on MS-related QoL measures (on both FAMS and Short-Form 36 scores, p<0.05 for comparisons between those with improvement in pre-existing disability and those without improvement).63,64 The durability of SRD remained associated with improved QoL over 4 years despite most patients not receiving retreatment with alemtuzumab over the 3 years following the initial treatment at Months 0 and 12.
In the CARE-MS II study, the development of thyroid AEs in alemtuzumabtreated patients with an inadequate response to a prior therapy did not affect QoL scores.65 Alemtuzumab-treated patients who developed thyroid AEs maintained greater QoL improvements than patients treated with IFNβ-1a. Cognitive impairment has not been examined directly in alemtuzumab-treated patients although a phase IV study to investigate neuropsychological functioning is ongoing (NCT00914758). The aim is to investigate the efficacy of alemtuzumab and IFNβ-1a in treating MS-related cognitive problems (e.g., attention, memory, speed of thinking). Slowing of BV loss has the potential as a surrogate for improved cognitive function so may be indicative of neurorehabilitation.66 In healthy individuals, BV loss occurs at a rate of 0.1–0.3%/year, whereas in MS it is more rapid at 0.5–1.35%/year.67 BV is an increasingly used outcome measure and has been assessed in numerous clinical studies, including CARE-MS I and CARE-MS II.38,39 BV loss with alemtuzumab was reduced to the normal range within 3–4 years and was significantly less than for patients receiving IFNβ-1a (p<0.0001 and p=0.0121, for CARE-MS I and II, respectively).66,68,69 In the CARE-MS extension study, the median annual BV loss in both studies was ≤0.2% in Years 3, 4 and 5 of the extension, which was lower than that observed during the 2-year pivotal studies.66,70
Discussion
T and B cells are key factors in the immunopathophysiology of MS and therapeutic strategies targeting both T and B cells are likely to be well suited to the pathophysiology of MS. Such treatments may be more effective than therapies that are active against only one cell type, although this has not yet been proven. Interestingly, alemtuzumab does not appear to be effective in other autoimmune diseases such as neuromyelitis optica (NMO) or NMO spectrum disorders (NMOSD). Moreover, on the basis of an NMO case with better response to rituximab compared to alemtuzumab treatment, it has been hypothesised that this beneficial effect may be attributed to a much more prolonged Blymphocyte depletion under rituximab treatment.71 Alemtuzumab has also been reported to convert a definite NMO to a secondary progressive course (myelopathy). This conversion is of interest, particularly taking into consideration that NMOSD is essentially attack-related.72
By exploiting both T and B cell targets in MS, alemtuzumab constitutes a highly effective and selective approach to managing MS and improving long-term outcomes. Alemtuzumab has a unique mode of action plus a durable effect that is maintained up to 5 years and longer, in the absence of re-treatment in many patients. Further, after depleting circulating T and B lymphocytes, alemtuzumab treatment is followed by differential repopulation that changes the balance of the immune system. These effects have been linked with the treatment’s consistent and manageable safety and tolerability profile.
The durability of the clinical effects of alemtuzumab after just two courses of treatment offers an entirely different treatment approach in MS. The extended efficacy of alemtuzumab has been demonstrated in a comprehensive clinical trial programme (including up to 5 years’ results in the two phase III studies). In these phase III studies, the treatment has shown superior efficacy to IFNβ-1a in terms of relapse, disability outcomes, MRI disease activity and slowing of BV loss. Alemtuzumab is currently used as first-line treatment in some European countries although, in the US, this is not the case.
Alemtuzumab also appears to promote neurorehabilitation by improving measures of physical functioning, disability, measures of QoL, and BV loss. Alemtuzumab has therefore demonstrated the potential to improve markedly the prognosis for many patients with MS while reducing the treatment burden.