Understanding MS Better in 2014
Contribution of Epidemiological factors
Multiple sclerosis (MS) is considered to be an immune-mediated neuro-inflammatory and neurodegenerative disease of the central nervous system (CNS) with heterogeneous clinical presentation and course, neuroimaging and pathological findings. Several genetic and environmental factors have been shown to show some association with MS; gene–environment interactions are hypothesised to have a stronger effect and the interplay between these factors might be due to common pathogenic mechanisms. Epidemiological factors are involved in the causality of MS and affect the disease course. Several well-validated environmental factors have been identified that are associated with MS susceptibility including vitamin D, viral infections (especially Epstein Bar virus [EBV]), smoking and adolescent obesity.
Vitamin D has been implicated to play a role in MS since several reports showed that low vitamin D levels might increase the risk of MS and may contribute to disease progression. Raised vitamin D levels decrease the risk of MS and this may explain the latitude effect on MS since ultraviolet light exposure increases vitamin D synthesis exerting a protective effect. Vitamin D may also influence disease course. The evidence for a protective effect is strong and has been demonstrated in several studies,1 but is not conclusive and a number of matters remain to be confirmed (e.g. the critical period for exposure, dose-response and gene/environmental interactions).
Epidemiological data are suggestive that EBV infection is associated with the development of MS. People with symptomatic EBV infection or with higher antibody responses to EBV are at greater risk of developing MS. Whereas EBV infection is evident in 90 % of the adult population, it is seen in 99 % of individuals with MS. In a 7-year follow-up of patients with clinically isolated syndrome (CIS), increased EBV-encoded nuclear antigen 1 (EBNA1)-specific immunoglobulin (Ig)-G responses were associated with a two times higher risk of developing MS, as well as greater disability and more new magnetic resonance imaging (MRI) lesions. People infected with EBV who develop mononucleosis have ~twofold greater risk of developing MS.2,3 EBV titres are elevated prior to disease onset and a history of infectious mononucleosis is more common in subjects with MS. However, it is unclear if EBV is causal or a marker of a predisposition to certain types of immune response.
Studies of genetics and gene-environment interactions could bring us closer to unravelling the biological relationship between smoking and MS, as the cause of this complex disorder likely involves interactions between environmental factors and genetic susceptibility. An increased risk of MS among smokers has been consistently found in numerous longitudinal studies with excess rates ranging from 1.3 to 1.7 for heavy long-term smokers compared with never smokers. Smoking increases both the incidence of MS and the risk of secondary progression and increases the risk of MS both in current and past smokers with duration and intensity independently affecting MS susceptibility.4,5 It may also influence the MS disease course.
Higher body mass index (BMI) (>27 kg/m2) before age 20 is associated with increased risk of MS with a twofold risk in women obese at age 10 and 20, although the mechanism is unclear. 6
A major question in terms of risk factors is when MS starts; probably several risk factors have an effect in adolescence. There is early but weak evidence (apart from major histocompatibility complex [MHC]) of gene/environment interactions. The Genes and Environment in Multiple Sclerosis (GEMS) project was set up to identify genetic, environmental and immune factors that may increase a person’s risk of developing MS in first-degree relatives. Results have confirmed the role of smoking but not BMI or mononucleosis in family members. The future goal is to shift the focus from treating MS to primary prevention for which it will be crucial to understand and then target the pathways that lead to immune dysregulation of MS.7
Predictive Markers in Multiple Sclerosis
A biomarker can be defined as ‘a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathological processes or pharmacologic responses to a therapeutic intervention’.8 The identification of validated biomarkers would be of considerable importance in MS. MS biomarker types include molecular and imaging categories and should ideally capture heterogeneity and assist in: diagnosis and disease stratification, predicting disease course, identifying new beneficial therapies, personalised therapy based on predicting treatment response and identifying patients at high risk of side effects. Of the numerous candidate biomarkers proposed, some have been validated and shown to be clinically useful.9
IgG oligoclonal bands (OCBs) represent IgG unique to the cerebrospinal fluid (CSF), that is, without corresponding IgG in the serum. They are commonly used as part of the diagnostic workup for MS, but are not essential to make the diagnosis. In patients with CIS, MRI and CSF OCBs are important tools for predicting conversion to MS, but the role of other body fluid biomarkers is controversial requiring confirmation. For example, the presence of IgG CSF OCBs doubles the risk of a second attack and in patients with IgM OCBs it occurs earlier.10,11 Other potential CSF biomarkers such as fetuin A, CXCL13, 14-3-3 protein and neurofilaments need to be validated in large CIS cohorts using multivariable analyses.
A study of 60 patients to identify proteins in CSF associated with conversion from CIS to MS using isobaric labelling and mass spectrometry for relative and absolute quantitation (i-TRAQ) found that chitinase 3-like 1 (CHI3L1) levels were increased and associated with shorter time to Clinically Definite Multiple Sclerosis (CDMS), brain MRI abnormalities at baseline and disability progression.12 CHI3L1 is primarily secreted by activated macrophages with expression induced by pro-inflammatory cytokines. Increased levels occur in disorders characterised by chronic inflammation. A large multicentre study of CIS patients has been initiated to validate this finding.
Genomic Data
Gene expression data are useful for diagnosis (differential, predisease state, across all disease stages) and for prognosis (relapse versus remission, outcome, secondary progressive MS [SPMS] and optic neuritis [ON]) of MS. Early gene expression studies showed differences between controls and MS patients regardless of treatment, non-treatment, the presence of remission or a relapse13 and between MS and other autoimmune diseases. Thus, there is a need to develop a tool that simplifies the exclusion of other explanations for neurological symptoms very early in the disease course prior to application of McDonald’s criteria. Archiron et al. merged MS genomewide association studies (GWAS) with differentially expressed genes (between MS and non-MS patients) to investigate the expression of MS susceptibility loci genes to assist in diagnosing MS and identified 42 genes with the potential to differentiate MS patients. Several genes are differentially expressed in an MS relapse compared with remission. For example, the TBX21 gene has been shown to be significantly underexpressed in acute relapse, whereas interleukin 8 (IL8) gene expression was significantly higher. By contrast, MMP9 gene expression was higher in both relapse and remission.14
Hanael investigated the processes that are common to or differentiate SPMS and relapsing-remitting MS (RRMS). He found that inflammation continues in SPMS with the driving force switched from T- and B-cells to over-activation of macrophages and that unique gene signatures can predict conversion to SPMS.15 Furthermore, activation of IFN-related genes is necessary for beneficial clinical response to treatment and it therefore may be possible to select SPMS patients that are likely to respond.
Gene expression data can also help in identifying patients with benign MS (BMS) who may progress. For example, the Pol-1 pathway is down-regulated in BMS and over-activated in RRMS and over-activation suppresses apoptosis giving enhanced autoreactive cell survival.16 Thus directly targeting the Pol-1 transcription pathway may represent a new class of MS therapeutics. Furthermore, CD19+ B-cells appear to have a significant role in the pathogenesis of the early phase of the first demyelinating event of acute ON, suggesting that they could be a target for immunomodulation in early ON. 17
Repair and Remyelination
Immunogenetics of Multiple Sclerosis
A wealth of data confirms that genetic variation is an important determinant of MS risk. Population, family and molecular studies provide strong empirical support for a polygenic model of inheritance, driven primarily by allelic variants relatively common in the general population. Around 30 years ago it was recognised that immune responsiveness is inherited and many human leukocyte antigen (HLA)- associated diseases exist. In MS, HLA class II genes (DR2) confer ~30 % of the genetic risk and the familial risks are largely genetic. The number of MS-associated SNPs identified has expanded rapidly especially with the introduction of the GWAS. An international collaborative GWAS involving 9,772 cases replicated almost all of the previously suggested associations and identified at least 29 new susceptibility loci giving a total of 53. The identity of the HLA-DRB1 risk alleles within the MHC has been refined and variation in the HLA-A gene underlies the independent protective effect attributable to the HLA class I region. Furthermore, the ImmunoChip MS project set up in 2013 by the International Multiple Sclerosis Genetics Consortium (IMSGC), identified 48 new genes (14,498 MS patients and 24,091 controls).18 Moreover, ImmunoChip network analysis of 79 genes indicated that two-thirds were expressed in the immune system, 50 % in the CNS but three genes only in the CNS.
There is modest co-inheritance between MS and other autoimmune diseases but parents of MS patients have no increased risk of autoimmunity indicating that shared genetic factors may not explain the increased risk.19 Recently, the identity of the HLA-DRB1 risk alleles within the MHC have been refined and it has been confirmed that variation in the HLA-A gene underlies the independent protective effect attributable to the HLA class I region. The risk of MS depends on both HLA-A and HLA-D genotypes. 20
Numerous studies have assessed the interaction between genes and environmental factors in terms of MS risk. In particular, there is an increased risk in smokers who are HLA-DRB1*15 positive and HLA-A*02 negative.21 Some genetic studies have suggested that MS is primarily inflammatory. Future genetic research will attempt to identify the genes behind each associated SNP marker and investigate the genetics of the course and outcome of MS, the MS subtypes and MS treatment.
Animal Models to Investigate Potential Therapies for Demyelination
Experimental autoimmune encephalomyelitis (EAE) is the most commonly used experimental model for the human inflammatory demyelinating disease, MS. Models of EAE share similarities and differences with MS and include acute, chronic relapsing, immunisationand virally induced Theiler’s murine encephalomyelitis virus (TMEV) EAE and cuprizone-induced demyelination. EAE is actively induced with myelin antigens in murine, rat and primates with suitable genetic backgrounds. A major criticism of the EAE model is that the pathology differs significantly from MS. The pathogenesis of MS involves inflammation, demyelination and axonal damage/loss. However, both inflammatory lesions and demyelination occur in EAE and there is a correlation between inflammation and axonal damage.22 Many features of MS are seen in both rodent and non-human primate models. It has also been suggested that classic EAE is a monophasic model whereas this is not the case with MS and MS subtypes do not occur in EAE. However, many of these features can be found in rodent or non-human primate models including triggers, spontaneous initiation, benign, acute and hyperacute, RR or relapsing progressive forms and ON involvement. New candidate immunotherapies have also been successfully tested in EAE, such as ion channel-based and neurotransmitter-based approaches, neuropeptides, cannabinoids and cell-based therapies.23 Thus EAE has helped in the development of immunotherapies that effect the inflammatory phase of MS. However, it is also well-known that many therapies that worked in this model have not shown to be beneficial in the human disease.
EAE models have also provided useful data in terms of halting the degenerative process or induction of remyelination in MS. Both rodent and non-human primate models have demonstrated the effect of neuronal stem cell transplantation in suppressing inflammation, enhancing remyelination and neurogenesis. Both mesenchymal stem cells (MSC) and stem cells administered intravenously, intrathecally, intranasally or by neurosurgical implantation in the CNS have been found in the spleen, lymph nodes and brain. The intrathecal route may be optimum as it results in direct targeting of the disease, good cell survival and migration/integration in their natural environment. EAE models therefore have facilitated the development of immunotherapies affecting the inflammatory phase of MS and may shed light on the pathogenic processes and mechanism involved in regeneration and remyelination.
Remyelination – A Strategy To Prevent Disability Progression in Multiple Sclerosis?
MS is an inflammatory-mediated demyelinating disease of the human CNS and demyelinated lesions in white matter/grey matter are the pathological and radiological hallmark of patients with MS. DMTs reduce the relapse rate and inflammation in RRMS, but completed trials have failed to show improvement in PMS. The irreversible damage of chronically demyelinated axons leads to disease progression. Remyelination occurs in MS and is neuroprotective, but is generally insufficient. Remyelination and exogenous repair with grafts and promoting endogenous repair, however, is a potential approach to treating PMS. To date, cell types evaluated for exogenous remyelination include myelin competent cells (oligodendrocyte precursor cells, Schwann cells and neural stem cells [NSCs]), non-myelinating cells (olfactory ensheating cells and boundary cap cells) and induced pluripotent stem cells (iPSCs). A study of human iPSC-derived oligodendrocyte progenitor cells (OPCs) in dysmyelinating mutant mice showed myelination and increased survival.24 Strategies with repairing cells are still experimental but iPSCs allow autologous graft, thus minimising rejection.
OPCs represent 5–8 % of cells in the adult brain and are disseminated in the CNS. After demyelination, adult OPCs can become activated and more mobile than quiescent OPCs (chemokinesis). Both CCL2 and IL1B genes (involved in the innate immune system) are upregulated on activated adult OPCs and induce the increased mobility, which is necessary for their recruitment to the demyelinated plaque.25 Endogenous guidance cues that control the migration of OPC during development include class 3 semaphorins (Sema 3A-attractant and 3F-repellant) and netrin 1 genes.26 Over-expression of Sema 3F gene increases both OPC recruitment (not due to proliferation) and also the remyelination rate.27 By contrast, overexpression of netrin prevents OPC recruitment and delays remyelination. Thus, early recruitment of OPCs after demyelination promotes remyelination, whereas preventing this recruitment decreases remyelination rate. The leucine-rich repeat and Ig domain containing 1 gene (Lingo 1) inhibits oligodendrocyte maturation and therefore an anti-lingo monoclonal antibody has been evaluated in a completed phase I trial and currently two phase II trials in RRMS and ON are ongoing.28,29
Many unsolved questions concerning remyelination remain, including the type of endogenous repair strategy (promoting recruitment of maturation) and which patients are suitable for treatment. A further limitation is the lack of a surrogate marker for remyelination.
Panel Discussion
It is uncertain if DMTs completely suppress inflammation and the resulting outcome could be problematical since inflammation is necessary for remyelination, but the exact mechanism is not fully understood. High-dose cytotoxic drugs suppress inflammation but not in the brain. The compartmentalisation30 of inflammation that occurs in the later stages of MS is seen in the Tylers animal model, which could therefore be used to study therapies. Interestingly, microbes in the gut of EAE mice appear to have a role in suppressing inflammation and this could be true for MS but studies are needed to verify this effect.
Mode of Action of Immunomodulatory Drugs in Multiple Sclerosis
MS is a chronic, immune-driven disease and the clinical course mirrors the different stages of pathology from the initial mainly inflammation and regeneration to destruction of neurons in the final stages. Within an individual MS lesion, different stages of inflammation and degeneration can occur. The phases of the disease may therefore require changing therapeutic approaches, but it is important to identify and understand the targets for intervention. Over time immunologically relevant target antigens may change. B-cells are involved in antigen presentation and cytokine production and have a complex role in MS. This has been exemplified by a study of atacicept (inhibits the survival and function of B-cells), which resulted in increased clinical activity.31 Thus a highly specific treatment approach may only be effective at a certain time.
Knowing the mode of action (MOA) of a DMT may be useful in identifying the right drug for a patient and predicting the risk and the possibility of neuroprotection and repair. The MOA may also predict the overall magnitude of a DMT’s clinical efficacy in an MS population, but not in the individual patient. Predicting safety from the MOA is also important. Drugs with pleiotropic effects are likely to exhibit a broad spectrum of safety signals while those with highly specific targets should have better predictability. However, the human immune system is too complex to fully understand the implications of highly specific therapeutic interventions and experimental models are poor at predicting safely in humans.
Neuroprotection is an important goal for therapy, but strong evidence is lacking with most DMTs. No evidence for a direct neuroprotective effect exists for IFN and natalizumab, it is very weak for glatiramer acetate (GA), laquinimod and alemtuzumab but stronger for dimethyl fumarate (DMF) and fingolimod. Studies with DMF in neuronal cultures and the R6/2 mouse model of Huntington’s disease indicate neuroprotection,32,33 and nerve repair has been demonstrated with fingolimod in the mouse nerve crush model. However, good evidence for direct neuroprotective effects or repair in patients is lacking for the available DMTs. Currently, the choice of the right immunotherapy for the individual patient based on MOA is a more evidence-based decision rather than a scientifically driven process.
Impact of Natural History on Treatment Decisions
Individualisation of Treatment
Although the ultimate goal of treatment is to cure MS, more realistically the aim is to prevent or delay disability. Disability results from the residual deficits following relapses, the progressive disease course (the major cause) or both. RRMS and progressive MS (PMS) can have an active or inactive (defined as >1 year with no relapses or new MRI activity) disease course.34 With RRMS, the main pathological correlates include subclinical relapses (MRI lesions), symptomatic relapses with partial or complete recovery or episodic inflammatory demyelination and remyelination. By contrast, PMS is characterised by insidious worsening neurological deficit with or without preceding or ongoing relapses and progressive axonal dysfunction or loss often with limited inflammation.
Radiologically isolated syndrome (RIS) is described as the incidental discovery of lesions suggestive of MS on brain MRI with demonstration of dissemination in space without symptom expression, a normal neurological examination and no better medical explanation to account for the observed anomalies. In RIS, some high-risk factors for conversion to CIS/MS are non-modifiable, such as family history of MS, while others including vitamin D level, obesity and smoking can be modified in order to attempt primary prevention.35,36 However, trials of DMTs are required to prove this in high-risk patients. Similarly, the prevention or delaying of RRMS would involve the use of tier-1 DMTs (interferon ßs [IFNßs] and GA) at an early stage of the disease course together with lifestyle and diet modification. In higher-risk patients, more potent DMTs are required (tier-2 including mitoxantrone, alemtuzumab, rituximab) to prevent or delay progression to RRMS, but they are associated with more severe side effects. Several factors such as greater age (in men), smoking, obesity and spinal cord disease are thought to increase the risk of developing PMS and in such patients preventing and/or repairing early relapses together with lifestyle modifications may delay PMS. The strongest risk is age but 25 % of patients never develop PMS.37 Although PMS cannot be slowed, intervening with ongoing relapses helps reduce disability. Different approaches (algorithms) have been developed to individualise the management of MS, including acute treatment of relapses and prevention of relapses with tier-1 or tier-2 DMTs.38 However, these algorithms are only guidelines and all have limitations such as the definition of disease severity, treatment failure and active disease.
Why Do Relapsing-Remitting Multiple Sclerosis Therapies Not Work for Progressive Multiple Sclerosis?
In 2014 a revised definition of PMS was proposed incorporating PPMS (progressive accumulation of disability from onset) and SPMS (progressive accumulation of disability after an initial relapsing course). The course can be:
- Active with progression (PPMS);
- Not active without progression;
- Active without progression; and
- Not active with progression.34
The different pathologies associated with MS suggest different therapeutic targets. Altered peripheral immunity to myelin could be due to broken tolerance and may be restored by DNA vaccines, or may be due to defective immunoregulation where peptide, cytokine or cellbased therapies could re-establish it. Many DMTs have been approved for RRMS but it is uncertain if they are effective for inflammatory tissue injury in the CNS, although some can enter the CNS. Macroglial and microglial activation in PMS are involved in continuing cortical demyelination, a process that has also been identified in early MS. Furthermore, subpial demyelination also occurs and may reflect compartmentalised inflammation.39 Vigorous remyelination occurs at times in MS, but almost always fails. Remyelination is unequivocally neuroprotective since chronic axonal degeneration is entirely absent from remyelinated shadow plaques.40 After demyelination sodium influx occurs, which reverses the sodium–calcium exchange leading to accumulation of intra-axonal calcium and activation of injury cascades.41 The proof-of-principle that PMS may be treatable has been shown in a phase II trial assessing the effect of high-dose simvastatin on brain atrophy and disability in SPMS. The mean annualised atrophy rate was significantly lower in treated patients (43 % reduction versus placebo; p=0.003).42 A phase III trial is now justified to confirm this promising result.
Main Driving Mechanisms of Different Phases of Multiple Sclerosis
Both B-cells and plasma cells are prominent components of inflammation in MS. In PMS, inflammation occurs within the blood–brain barrier (BBB) so only anti-inflammatory drugs that pass through the BBB are likely to be effective. Furthermore, as MS progresses, differences are observed in inflammatory features. The slow expansion of preexisting lesions in particular but also subpial cortical demyelination, diffuse white matter injury and brain atrophy are more characteristic of SPMS than RRMS. Demyelinaton and neurodegeneration are the result of mechanisms involving cytotoxic T-cells and are antibody mediated in acute MS and RRMS, but in PMS they are more likely to result from oxidative injury and mitochondrial damage.
Fischer et al. studied gene expression in active cortical lesions from PMS and identified 301 genes associated with oxidative injury in mitochondria, which is a major mechanism of demyelination and neurodegeneration in MS lesions. A similar degree of oxidative injury was not seen in other inflammatory brain diseases.43 The predominant changes in expression of genes were for axonal and dendritic plasticity and myelin regeneration. Mitochondrial injury in MS is driven by inflammation in which oxidative bursts accumulate with disease duration leading to energy deficiency. Furthermore, injured mitochondria are an additional source of reactive oxygen species.
The pathophysiology of PMS has consequences for therapy. Since there are similar disease mechanisms between RMS and PMS, early effective treatment should delay onset of progression. However, drugs that are effective in PMS must act within the CNS and treatment should target both inflammation and neurodegeneration.
Impact of Magnetic Resonance Imaging Techniques on Clinical Practice
Specificity of Magnetic Resonance Imaging for Multiple Sclerosis
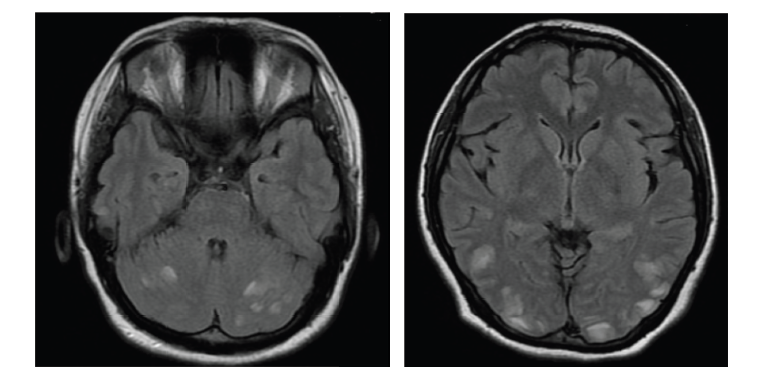
MRI has played an expanding and unique role in the diagnosis, management and differential diagnosis of MS. MS lesions exhibit numerous different characteristics in terms of their site, shape, distribution and evolution. Differential diagnosis involves distinguishing MS from other conditions such as metabolic, vascular, genetic, psychiatric disorders and neoplastic, infectious, diseases and also from variants that mimic MS (e.g. acute disseminated encephalomyelitis [ADEM]). MRI plays a major role in the diagnosis of RIS by distinguishing it from an incidental radiological finding. Diagnosis of RIS involves a careful collection of clinical history, a meticulous clinical examination and extensive differential diagnosis using MRI.44 The 5-year risk of an initial clinical event in RIS depends on a number of factors including involvement of the spinal cord, gender, age (≤37 versus >37 years) – the risk increases with the number of these factors identified. 35
MRI scans significantly assist in reaching a definitive diagnosis of MS. Leber’s hereditary ON (LHON) and MS-like disease (LMS) in association with MS often coexist, so it is important to define their features.45 MRI scans are also useful for distinguishing MS from other disorders. For example, idiopathic inflammatory demyelinating lesions (IIDLs) of the brain that have a morphological pattern characteristic of MS and thus pose significant diagnostic problems. IIDLs often present as ringlike lesions and sometimes megacystic, Balolike or diffusely infiltrating lesions. The ability to recognise these patterns may assist in the differential diagnosis. Moreover, fluid-attenuated inversion recovery (FLAIR) MRIs can distinguish MS from PML lesions by their shape, size, mass effect, location and persistence.46
Biological Correlates of Magnetic Resonance Imaging Findings in Multiple Sclerosis
Biological correlates of MRI include clinical (relapses, relapse-related disability and progression) and pathological (inflammation, demyelination and neuroaxonal loss) parameters. In RRMS there are ~10 new gadolinium (Gd)-enhancing lesions per relapse and a robust correlation of treatment effect on active MRI lesions and relapses is seen.47,48 Brain atrophy, a global measure of neurodegeneration, correlates with treatment in RRMS trials and can be used to monitor neurodegeneration in clinical progression. Approximately 75 % of disability is correlated with new lesions/atrophy.
Cortical lesions can be visualised on MRI by double inversion recovery (DIR) and phase-sensitive inversion recovery (PSIR). However, DIR has limited sensitivity, detecting ~18 % of intracortical lesions,49 while PSIR is more sensitive and accurate detecting three times more cortical lesions.50 Magnetisation transfer ratio (MTR) reflects demyelination in MS cortex and can show segmentation of outer and inner cortex. A recent study demonstrated that the MTR is: higher in the outer cord layer than cord white matter, lower in patient groups compared with controls (controls>CIS>RRMS>SPMS=PPMS), abnormal in CIS and RRMS patients and independently correlated with cord atrophy. 51
Spinal cord atrophy can be measured by 3D T1 MRI and correlates with EDSS – the mean rate of cord area loss is 1 % per year. However, there is no consistent correlation between T2 lesion load and disability. A more accurate measure of cord lesion can be obtained with a combination of 3D-T2 and 3D-PSIR (T1) axial images.52 In a multivariate regression model cord lesion load and cord atrophy have been shown to independently contribute to EDSS (R2 = 0.56).53 Diffuse abnormalities appear as hyperintense areas on T2-weighted MRI with ill-defined edges, but are not visible on T1-weighted MRI. Kearney demonstrated that progressive MS and disability are associated with more intensive focal lesions, grey matter involvement and diffuse abnormalities in the spinal cord. Furthermore, cord atrophy and grey matter radial diffusivity independently contribute to EDSS .
Future Magnetic Resonance Imaging-based Techniques that should be Part of Daily Multiple Sclerosis Practice
In order to monitor inflammatory activity it is likely that a subjective count of new lesions will be necessary using MRI techniques. This will entail using image subtraction from consecutive timepoints with automated software accounting for intensity normalisation inhomogeneity correction and image co-registration.54 The utility of monitoring lesion activity (inflammation) is exemplified by a 20-year study in CIS patients of disability and T2 MRI lesions. The estimated rate of lesion growth over 20 years was 0.8 cm3/year in those with a RRMS course and 2.89 cm3/ year in those who developed SPMS.55 Results from another study in RRMS patients indicated that the number of new T2 lesions at 1 year predicted the 5-year EDSS score.56 Finally, Rio et al. showed that MRI changes during the first year of IFNß treatment can have prognostic value for identifying patients with increase disability after 2 years therapy with only the presence of >2 active lesions at year 1 related to an increase in disability after 2 years of therapy.57
Diffusion tensor (DTI) MRI images have been used in CIS patients to examine the relationship between white matter lesions and deep grey matter loss. The proportion of the thalamocortical volume over the entire white matter volume was 28 % and 78 % of the lesion volume was found in the thalamocortical tracks.58 It should also be necessary to monitor the consequences of inflammatory demyelination and degeneration by documenting tissue loss with MRI volumetric measures. Many options and software are available for this monitoring, such as brain surface contour measurement, grey/white matter segmentation and cortical thickness but validation is uncertain. Furthermore, it is necessary to consider the following before using volumetric measures in daily practice: standardised MRI protocol, software with low scan– rescan reproducibility and highly correlated with clinical trial data on atrophy, >6 months interval between scan, need to establish a range using reference populations (normal ageing, untreated MS), age- and gender-matched normative data
The consequences of inflammatory demyelination and degeneration should be monitored as they are clinically relevant and new MS DMTs have an impact of brain volume loss.
The Changing Spectrum of Neuromyelitis Optica
Diagnostic criteria for neuromyelitis optica (NMO) and transverse myelitis were first developed in 2006, but subsequently a number of observations have suggested that they should be revised, including:
- The discovery that NMO-IgG can be reliably recognised earlier;
- Recurrent myelitis or recurrent ON occur;
- Brain lesions may occur – as the presenting manifestations and can be highly suggestive or diagnostic; and
- Co-association of other autoimmune conditions that may exclude NMO.
Consequently in 2011 an International Panel for NMO Diagnosis (IPND) met to revise the criteria. The resulting criteria included NMO spectrum disorders (NMOSD) as the unified term, stratification by serostatus and the provision for future revisions. The clinical course and laboratory findings are more typical of MS and other pathology and there are established and suspected comorbidities that mimic NMOSD. Diagnosis of paediatric NMOSD uses the same criteria as adult although there is a greater incidence of cerebral presentations and it must be distinguished from longitudinally extensive transverse myelitis (LETM) in paediatric MS.
Jarius et al. highlighted that NMO is heterogeneous with seropositivity more likely to be associated with women, systemic autoimmune disease, unilateral ON, ON or myelitis and relapses.59 Furthermore, a study examining the distinction between myelin oligodendrocyte glycoprotein (MOG) antibody-positive and aquaporin-4 (AQP4) antibody-positive (NMOSD) found that patients with NMOSD and MOG antibodies have distinct clinical features, fewer attacks and better recovery than those with AQP4 antibodies or those who were seronegative for both antibodies.60
Two manifestations of NO are now recognised with respect to AQP4 and MOG: AQP4 positive, relapsing and autoimmune occurring in older predominantly female patients; MOG positive, ADEM-like, monophasic occurring in younger patients with an equal sex ratio.61
Stem Cells in Neurological Disorders
The multifocal nature of MS complicates cellular therapy and puts emphasis on both the donor cell origin and the route of cell transplantation. Considerable progress had been made in the development of NSCs. Damaged cells can be replaced by transplantation of either brain tissue, neural precursors cells (NPCs) or neural cells, all which differentiate into the desired cell type. The next goal is to prevent or repair tissue damage using transplantation of undifferentiated NPCs. NPCs exhibit therapeutic plasticity showing pathotropism, bystander (paracrine effects) and the ability to replace cells.62,63
The origin of microglial cells was uncertain but recently it was discovered that in mice they develop in the yolk sac and infiltrate the early forebrain of embryos via the blood circulation and therefore their appearance in the CNS precedes the onset of neurogenesis.64 Transplanted stem cells work therapeutically through cell replacement and also via the bystander effect. NPCs and other types of stem cell exert neuroprotective effects by secreting trophic factors and immunomodulatory molecules. These foster endogenous precursors to promote remyelination and to directly and indirectly rescue damaged axons/neurons and also recapitulate physiological non-neurogenic homeostatic functions exerted by endogenous NPCs.
A number of important issues, however, remain to be addressed, for example, the optimum way to tightly control and regulate the various therapeutic stem cell-mediated effects in vivo. These include:
- The differentiation state of the cells (stem or precursor).
- Whether the cells should be injected in the acute or chronic phase.
- The number of cells in single or multiple injections.
- The injection route (homotopic or heterotopic).
Symptomatic Treatment in Multiple Sclerosis
The localisation and severity of MS lesions within the brain and spinal cord is unpredictable and, therefore, a wide range of body systems can be adversely affected to a variable degree. Since there is no cure for MS, management of symptoms should be a priority. Fatigue, cognitive loss, psychological problems, spasticity, autonomic dysfunction, tremor and pain are major problems with MS. Consequently, there are myriad symptoms and comorbidities associated with MS that can impact negatively on patient quality of life (QoL). Symptomatic treatment in MS is the main pre-occupation of patients and their neurologists. Multiple, disparate symptoms occur in different systems but there are limited therapeutic options. To date, trials of symptomatic treatments have been of poor quality and low-powered with subjective qualitative endpoints and few quantitative ones. There is a perception that large pharmaceutical companies are not interested in such therapies since they are very expensive to develop and 45 % of trials are industry funded. Symptomatic outcomes, however, are generally tertiary endpoints in DMT trials.65 However, many existing drugs for other indications have potential efficacy against these symptoms and could be re-purposed, but academic neurologists need to set up better trials to evaluate them.
The aim of symptom management is to reduce symptoms, improve health-related QoL and ensure independence through pharmacological treatment. Currently some symptoms are managed well (e.g. spasticity and pain) while others are not (e.g. cognition and visual impairment). For example, 4-aminopyridine provides partial restoration of saltatory conduction – in a trial only ~30 % responded with >20 % improvement in the timed 25-foot-walk test.66 In the real world only 16 % of patients had objective improvement at 6 months, indicating benefit decreases over time, although 60 % reported improvement. Furthermore, chronic neurogenic pain can be managed by drugs (such as cannabinoids [e.g. Sativex], which significantly improve pain score) and spinal cord stimulation.67 Bladder dysfunction is also well controlled both with and without drugs and a simple algorithm has been developed.68 By contrast, fatigue is poorly managed with no strong evidence for successful drug treatment but aerobic exercise, physiotherapy, yoga and progressive resistance training having a weak effect. Unfortunately the numerous drugs that can be used to relieve symptoms often have side effects that worsen the symptoms being treated.
Neurologists need to collaborate to develop clinical trials and establish better quantitative measures to address patients’ unmet needs. In addition, funding agencies should urgently allocate specific directed funding for individual symptom relief.
Panel Discussion
The consensus was that treatment should be stopped when SPMS starts but in the US it is restricted when a certain age is reached. A biomarker to inform when it is safe to stop treatment would be valuable. The treatment rationale for MS is debatable because as many as 90 % of lesions could be asymptomatic. The participants at this meeting agreed, however, that early treatment is beneficial, although it is important to choose the best medication and aim to personalise treatment. As funds for drugs treatments are limited in most countries, there is an increasing need for safe and effective therapies in MS that are, above all, less expensive. Future MS Days meetings are planned with the aim of continuing to help clinicians to keep up-to-date with the latest developments and advocate the most effective treatments and best practice in MS management.
Nation-specific Treatment Approaches in Multiple Sclerosis
Based on the natural history of MS, early aggressive treatment should be initiated in RRMS to suppress disease activity since preventing relapses and development of underlying progression should reduce later disability. Evidence that earlier treatment potentially gives better outcomes has been accumulated with all DMTs from CIS and long-term follow-up studies.69
An assessment of how countries approach treatment of RRMS has recently been completed. In order to achieve more uniform access to effective treatment a number of factors should be considered, including the efficacy of the healthcare system, the advocacy and knowledge of providers and the role of regulators, lay organisations and pharma. Responses to severn questions were collected from 16 countries. MS prevalence varied from >200/100,000 in Denmark and Germany to <10/100,000 (China, India, Japan and Korea) and in all countries a drug regulatory authority oversaw the availability of MSspecific drugs. However, there was variation regarding the time when DMTs were available to prescribe (from when marketed to <5 years) and reimbursement (from all DMTs to only one). Furthermore, within countries, availability varied according to the source of reimbursement (private health insurance or government) and also varied as a result of directives from regulatory authorities (e.g. European Medicines Agency, National Institute for Health and Care Excellence in the UK, Pharmaceutical Management Agency in New Zealand, US Food and Drug Administration). Unfortunately, these regulations have disadvantaged clinicians and patients by not allowing for changing clinical paradigms and impeding responsiveness to changing practice based on experience, accumulating knowledge and evidence.
MRI availability ranged from very limited in two countries to widespread in the others. Accessibility was restricted to a greater or lesser degree in many countries and routine use to monitor MS ranged from ≥9 to ≤1 scans per annum. In all countries MRI was used to determine McDonald 2010 diagnostic criteria but treatment of CIS was not routinely offered in five, limited to injectable DMTs in four, injectable and some other DMTs in six and all treatments were offered only in Australia. Access to treatment showed considerable variation especially in the Asian Oceania region (60 % of the world population). The high cost of DMTs and recent large price increases makes them difficult to afford in many countries. This study highlights the inequality of treatment access in some countries. To help address this problem, support from international agencies is needed (e.g. Multiple Sclerosis International Federation, World Brain Alliance) together with prescribing generics and innovative or more economic use of DMTs (such as dosage based on bodyweight or longer dose intervals).
Challenges and Difficulties in the Diagnosis and Treatment of Multiple Sclerosis in Turkey
The findings of a 36-question survey to compare the opinion of 318 neurologists (285 general versus 33 MS experts) in 22 cities in Turkey on MS diagnosis, management, pregnancy issues and timing/interpretation of MRI scans were discussed. The survey results indicated that:
- In clinically stable patients fewer general neurologists refer patients for a follow-up MRI scan than MS experts whereas 6-month MRI referral rates are higher in general neurologists. MS experts also tend to follow patients more frequently.
- General neurologists were more likely to depend on radiologist’s reports, whereas MS experts interpret MRIs themselves.
- MS experts consider presence of black holes and brain atrophy in progressing patients to be more important variables than general neurologists.
- General neurologists switch DMTs faster and treat more RIS patients and would not consider brain atrophy or low vitamin D levels factors for treatment change.
Often the radiologist did not wait long enough to obtain a good GD contrast and their reports generally contained errors. On switching, if a new lesion appeared after 1 year of treatment, it was generally agreed that it is best to maintain treatment and monitor the patient closely. The time needed to assess treatment response varied from 3 to 12 months and a patient should be followed up 1 month after treatment initiation. All neurologists had easy access to CSF analysis and most would not treat RIS. The panel expressed concerns regarding over-diagnosing MS and were cautious about pregnancy advising on a patient-by-patient basis, although there was no consensus. Most would stop treatment during pregnancy. The level of vitamin D was assessed in some, mostly private, hospitals in Turkey.70,71
Future Focus of Multiple Sclerosis Treatment
Preventing Clinical Multiple Sclerosis from the Beginning by Treating Radiologically Isolated Syndrome?
CIS describes the first clinical episode of symptoms and signs suggestive of an inflammatory demyelinating disorder of the CNS, whereas the term RIS was proposed to describe asymptomatic individuals who possess radiological abnormalities highly suggestive of MS. Incidental findings are observations of potential clinical significance in healthy subjects or patients recruited to brain imaging studies. In this respect, widespread use of MRI has increased the detection of white matter anomalies that may herald the onset of a seminal event prior to the onset of symptoms – prevalence from incidental findings varies from 0.05 to 2 %. RIS can be defined as a presentation with MRI findings highly suggestive of MS based on location and morphology within the CNS but in the absence of overt clinical symptoms. Prevalence of RIS is unknown but estimates from three large post-mortem investigations ranged from 0.08 to 0.2 % and a meta-analysis of 15,559 of the general population reported 0.06 %.73–76 The diagnosis of RIS requires the presence of incidentally identified CNS white matter anomalies meeting the following MRI criteria:77,78
- Ovoid, well-circumscribed, homogeneous foci with/without corpus callosum involvement.
- T2-hyperintensities (>3 mm) fulfilling three of four Barkof criteria for dissemination in space.
- CNS anomalies not consistent with a vascular pattern.
- No historical accounts of remitting clinical symptoms.
- MRI anomalies not due to direct physiological effects of substances (recreational drugs, toxic exposure).
- Exclusion of MRI phenotypes suggestive of leukoaraiosis or extensive white matter pathology lacking involvement of the corpus callosum.
- MRI anomalies not better accounted for by another disease process.
An Radiologically Isolated Syndrome Consortium (RISC) study evaluated the 5-year risk of the development of the first symptomatic demyelinating event in 451 RIS subjects. Of these, 83 % had positive spinal cord MRI and 10 % developed PPMS, which mirrors populationbased studies. The main risk factors were spinal cord lesions, age <37 and male gender.35 However, standardised studies are required to improve diagnostic criteria and risk estimates. Management/ treatment of RIS is controversial. Three strategies have been proposed: wait (no follow-up, but patients advised to seek healthcare if symptoms occur); planned clinical and radiological follow-up; and treat with DMT (but potential benefit unproven). Surveys suggest that periodic evaluation is the most common approach but off-label treatment is increasing.