Neuromyelitis optica spectrum disorder (NMOSD) is a rare inflammatory autoimmune disease of the central nervous system (CNS) with a worldwide distribution.1 The first clinical description of NMOSD was made a century ago by Devic and Gault, who documented patients with monophasic and bilateral optic neuritis (ON) and myelitis.2 A few decades ago, NMOSD was considered a variant of multiple sclerosis (MS). However, after the discovery of antibodies against aquaporin-4–immunoglobulin G (AQP4–IgG) in the serum of patients with NMOSD, this disease has been considered a distinct condition from MS.3–5
The diagnostic criteria for NMOSD have evolved over the last decades. In 2015, the International Panel for NMO Diagnosis published the current diagnostic criteria, which defined the disease groups based on the positivity for AQP4-IgG.6 However, even with the use of the best cell-based assays (CBAs) for AQP4-IgG, some patients with clinical symptoms compatible with NMOSD are still seronegative. In addition, some of these patients who were AQP4-IgG seronegative were positive for another antibody (around 20%), targeting the myelin oligodendrocyte glycoprotein (MOG-IgG), which defines the condition as MOG-IgG-associated disease (MOGAD).7–11 In the absence of AQP4-IgG and MOG-IgG, patients are commonly defined as double-seronegative NMOSD.7,9,12–15
The prevalence of NMOSD varies from 0.5 to 4 per 100,000 people, and it might be as high as 10 per 100,000 people in Black populations.16,17 Epidemiological studies showed that NMOSD seropositive for AQP4-IgG is more prevalent in females (9 females to 1 male), and the mean age of onset is 40 years.9,12,18 In MOGAD, the disease usually occurs in a proportion of 1 female to 1 male and is more frequently detected in children than in adults.19,20 However, there are few epidemiological data about double-seronegative NMOSD. Previous studies reported that there are no gender differences in this condition, and that Caucasian populations are more affected.21–26
Due to the lack of information about double-seronegative NMOSD, this article aims to review the data about this condition, including clinical presentation, diagnosis, pathogenesis and current and future treatment options, in an attempt to improve the medical care and management of patients with double-seronegative NMOSD.
Clinical presentation and diagnosis of seronegative neuromyelitis optica spectrum disorder
Clinical presentations of NMOSD can vary from symptoms involving posterior and bilateral ON, longitudinally extensive transverse myelitis (LETM), area postrema lesions and hypothalamic lesions. Patients can present symptoms such as bilateral and usually severe reduced visual acuity, paraparesis or quadriparesis, urinary dysfunction, sensory loss or reduction, nausea, vomiting, prolonged and refractory hiccups, excessive daytime sleepiness and narcolepsy. These symptoms appear as rapidly progressive attacks, may last days and have varying degrees of recovery, over weeks or months.1,27,28
Some clinical differences can be noticed when comparing patients with AQP4-seropositive and double-seronegative NMOSD. Some previous studies showed that patients with seronegative NMOSD present with a multifocal clinical presentation (ON and myelitis), a lower association with other autoimmune disorders, symptoms of shorter duration and a monophasic course when compared with patients with AQP4-IgG-positive NMOSD. Furthermore, there are few studies indicating that myelitis and ON might be less severe in seronegative patients.21,23,29,30 Regarding acute visual symptoms, patients who were AQP4-IgG seropositive have a lower score in visual functional system evaluation, a more severe optic disc oedema and a higher risk of subsequent ON attacks.31 However, the long-term prognosis was revealed to be similar in patients with and without AQP4-IgG positivity.26
Some authors reported controversial findings about onset symptoms in patients with seronegative NMOSD. Some of these publications suggested that bilateral ON isolated or in association with LETM is the most frequent onset phenotype.23,30 However, other studies demonstrated myelitis attacks as the most common first clinical presentation.25,32 In addition, brainstem lesions, such as area postrema lesions, appear to be more frequent in AQP4-IgG-positive NMOSD.9,25,30,32–34 The disease course of NMOSD comprizes recurrent attacks in about 95% of the patients, but this is biased by the AQP4-IgG-positive cases.35 Patients who are seronegative for AQP4-IgG have a higher tendency of monophasic disease or a lower number of subsequent acute attacks.23,25,26,29,32,33 In MOGAD, comparative studies showed that unilateral ON isolated or associated with myelitis is the most frequent onset symptom, and a recurrent clinical course with ON attacks is commonly observed.26
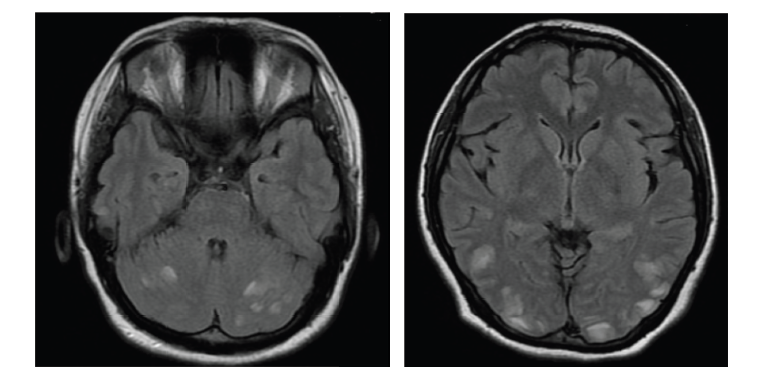
Regarding the radiological pattern, some studies did not find significant differences between patients with seropositive and seronegative NMOSD, with cervicothoracic myelitis seen in both groups.26,29 Nevertheless, in other studies, LETM was more frequent in patients who were AQP4-IgG positive,23,32 while there was no difference in the number of lesions in supratentorial and infratentorial regions based on the AQP4-IgG status.23 A common radiological pattern of ON found in patients with NMOSD is a bilateral, posterior and intracranial inflammatory lesion of the optic nerves, which may be extensive lesions with inflammation occurring up to the optic chiasm. In MOGAD cases, patients present with magnetic resonance imaging (MRI) features, showing ON associated with perineural oedema, short myelitis and fluffy, extensive, acute disseminated encephalomyelitis (ADEM)-like lesions in supratentorial regions.12,36–38
In 2015, the international consensus diagnostic criteria for NMOSD were published.6 At least one core clinical characteristic is necessary for the diagnosis of patients with NMOSD with AQP4-IgG (detected by the CBA), which can be ON, acute myelitis, area postrema syndrome, acute brainstem syndrome, symptomatic narcolepsy or acute diencephalic clinical syndrome or symptomatic cerebral syndrome. Nevertheless, the diagnosis of seronegative NMOSD requires the presence of two core clinical characteristics occurring as a result of one or more clinical attacks. It is mandatory that one attack is related to ON, LETM or area postrema syndrome. In addition, the presence of attacks in more than one area and additional findings in the brain and/or spinal cord MRI are essential for the diagnosis. A recent review emphasizes the importance of following the diagnostic criteria, as a diagnosis can be made after one clinical attack in those who are AQP4-IgG positive.33
The CBA for AQP4-IgG is the gold-standard method for the detection of these antibodies. The antibody titres can vary over time, depending on the disease activity and treatment.33,39,40 In one study, around 30% of patients initially negative for AQP4-IgG by CBA had a positive result in a mean interval of 36 weeks from the disease onset. Some authors recommend retesting AQP4-IgG during an acute attack or within 3 months after the last attack.34
Pathogenesis
Almost all the current knowledge about the disease mechanism related to NMOSD is associated with AQP4-IgG.3 These antibodies selectively bind to aquaporin-4 water channels, mainly M23 isoforms,41 which are more expressed at the level of astrocytic end-foot processes. Primary astrocytic damage is evident in immunohistochemistry analyses,42 while myelin and axonal damage appears as secondary events of the disease.42–44 This explains the presence of high levels of glial fibrillary acidic protein (GFAP) found in the cerebrospinal fluid (CSF) of patients with NMOSD, which can have correlations with disability and lesion length in myelitis.44–47
However, there is an information gap in the pathogenesis of patients with seronegative AQP4-IgG, as the astrocytic damage is not as clear as it is found in patients who were seropositive.5,24 Purified IgG from patients who were seronegative was not associated with the reproduction of typical NMOSD pathology with astrocytic damage.48 Nevertheless, cellular responses against AQP4, such as Th17 cells, may play a role in patients with seronegative NMOSD.46,49
The main characteristic feature of the CSF in patients with NMOSD is pleocytosis, with the presence of neutrophils and eosinophils. Oligoclonal bands may be found in up to 10–15% of cases.9,30,50–52 Furthermore, some studies demonstrated differences in serum and CSF biomarkers, such as GFAP and S100B levels, between patients who were seronegative and seropositive. The authors found that these protein levels were higher in patients with seropositive AQP4-IgG.53 However, in another study, no differences were found in GFAP levels, in the CSF and serum, between patients with seropositive and seronegative NMOSD.54
Management, current treatment options and treatment advances
The aim of NMOSD management is to treat acute attacks, prevent further attacks and reduce the disease-related burden in patients. The treatment of AQP4-IgG-positive NMOSD has improved over the last decades, but the alternatives for seronegative cases are still limited to off-label immunosuppressive drugs.
Acute management
An optimized acute management of attacks promotes a greater recovery of symptoms in patients with NMOSD, mainly due to the suppression of the inflammatory response and CNS injury. The treatment of NMOSD attacks should be initiated early and aggressively, as this can reduce the disability accrual in NMOSD.55–57
The use of high doses of intravenous methylprednisolone (IVMP), 1 g/day for 3–7 days, followed by oral corticosteroid therapy, may be the first-line acute treatment, considering that about 35% of patients may show good recovery.58–60 However, it is common to have a poor response to corticosteroids, requiring the use of five to seven sessions of therapeutic plasma exchange (PLEX) or immune adsorption (IA) on alternate days.55,61 PLEX/IA can be used as a first choice in severe or disabling attacks, as some studies suggest that a greater response can be observed with PLEX/IA when compared with treatment limited to IVMP.59,60,62 In previous studies, PLEX/IA in association with IVMP showed better recovery of symptoms in 65% of patients with NMOSD.63
There are no data about the difference between the acute treatment of attacks in patients with seronegative and seropositive AQP4-IgG. Some preliminary studies demonstrated the benefits of intravenous human IgG, mainly associated with IVMP. However, this recommendation is still controversial.64
Attack prevention treatment
Prevention of attacks is recommended for all patients diagnosed with NMOSD, especially those with recurrent attacks. The aim is to avoid new attacks associated with the accrual of neurological disabilities. After 2019, three drugs were approved for AQP4-IgG-positive NMOSD. However, no drugs have been approved for patients who were seronegative.
Over the last decades, drugs, such as azathioprine (AZA), mycophenolate mofetil (MMF), tacrolimus, mitoxantrone and cyclophosphamide, have been used as off-label preventive treatments for these patients, with previous studies showing a reduction in annualized relapse rate (ARR).65–77 The initial effect on immunosuppression by AZA and MMF starts within 4–6 months, therefore, it is common to use oral corticosteroids for the initial treatment period.54 Previous studies have reported a significant decrease in relapses and the disability level related to AZA.67,78,79 In 2017, a study demonstrated that the use of MMF was effective and safe as a first-line treatment for patients with NMOSD, independent of the serology status of AQP4-IgG.80 In addition, another commonly used first-line therapy is rituximab (RTX), a monoclonal antibody that selectively depletes CD20+ B cells. This therapy requires intravenous infusions every 6 months, and the biological effect may be monitored by CD19+ cell counting. RTX requires safety monitoring for immunoglobulin levels.81 A comparative study demonstrated a high efficacy of RTX in reducing attacks compared to placebo.80,82 This treatment was associated with decreased or stabilization of disability in 93% and a 60% reduction in the ARR in 5 years.83 A greater efficacy of RTX has been reported when compared with AZA and MMF.75,76 Despite the evidence indicating some effects of these immunosuppressive drugs in reducing attacks and disability for patients with seropositive and seronegative NMOSD, RTX showed a greater association with relapse- free after long-term follow-up.84
Tocilizumab (TCZ), a monoclonal antibody against the interleukin-6 (IL-6) receptor, has also been used as an off-label preventive treatment option for patients with NMOSD.71,85 One study showed a decrease in clinical and radiological activity of the disease in patients with a previous use of RTX.85 In a comparative study with AZA (Tocilizumab vs Azathioprine in Neuromyelitis Optica Spectrum Disorders [TANGO] study; ClinicalTrials.gov identifier: NCT03350633),86 TCZ was associated with a longer interval between attacks, as well as a reduction in the ARR. Ringelstein et al. studied the effect of TCZ in ARR decrease in patients with MOGAD and seropositive and seronegative AQP4-IgG NMOSD.87 This outcome was statistically significant for the first and second groups. However, it is worth emphasizing that the representative sample of the seronegative AQP4-IgG group was only 7 patients (MOGAD = 14; AQP4-IgG+ = 36), which may have limited further conclusions related to this group.
Randomized controlled trials (RCTs) have recently been published demonstrating the efficacy of three monoclonal antibodies for the treatment of patients with AQP4-IgG-positive NMOSD, but the results were inconclusive for patients who were seronegative. These drugs target B cells, IL-6 receptor and complement system.88–90 The PREVENT trial (A Randomized Controlled Trial of Eculizumab in AQP4 Antibody-positive Participants With NMO, ClinicalTrials.gov identifier: NCT01892345) analyzed the efficacy of eculizumab, a monoclonal antibody that blocks the complement protein C5 and prevents the activation of the complement cascade, in patients who were AQP4-IgG seropositive.88 Eculizumab was found to be effective in reducing ARR in 94% of the patients when compared with placebo, and 98% of the patients were relapse-free during a period of 12 months. Digala et al. reported a single patient with seronegative AQP4-IgG NMOSD treated with eculizumab, which was refractory for initial therapies. This patient was relapse-free for 12 months and showed an improvement in disability measured by the Expanded Disability Status Scale (EDSS).91
SAkuraSky89 (Efficacy and Safety Study of Satralizumab (SA237) as Add-on Therapy to Treat Participants With Neuromyelitis Optica (NMO) and NMO Spectrum Disorder, ClinicalTrials.gov identifier: NCT02028884) analysed the effect of satralizumab, an IL-6 receptor blocker, as an add-on therapy for AZA, MMF and oral corticosteroids in patients with NMOSD. The study sample included 70% of seropositive AQP4-IgG, and the remaining were patients who were seronegative. Satralizumab was associated with a relapse-risk reduction in 79% of patients who were seropositive when compared with placebo. Positive outcomes were detected for at least 21 months in the long-term follow-up study with patients who were seropositive.92 However, there was no significant difference in outcomes for patients with seronegative NMOSD when compared with the placebo group. In a second RCT (SAkuraStar; Efficacy and Safety Study of Satralizumab (SA237) as Monotherapy to Treat Participants With NMO and NMOSD, ClinicalTrials.gov identifier: NCT02073279 ), satralizumab was evaluated as a monotherapy for patients with NMOSD, both seropositive and seronegative AQP4-IgG, compared with placebo.93 A subgroup analysis suggests that satralizumab reduced the risk of relapse in seropositive AQP4-IgG. However, there is insufficient evidence to indicate a risk reduction for the seronegative subgroup, mainly due to a greater degree of disease heterogeneity, as well as the small sample size (n=24).93 The same tendency was found in a study published in 2021, which evaluated the efficacy of satralizumab in patients with seropositive and seronegative AQP4-IgG. In the seropositive subgroup, 77% of patients who received satralizumab were relapse-free in a period of 24 months when compared with placebo subgroup (41%). Nonetheless, in the seronegative subgroup, 63% of patients using satralizumab were relapse-free for the same period when compared with 78% of the placebo group.92
Monotherapy with inebilizumab, a monoclonal antibody depleting CD19+ B cells, was compared with placebo in the N-MOmentum study (A Clinical Research Study of Inebilizumab in Neuromyelitis Optica Spectrum Disorders, ClinicalTrials.gov identifier: NCT02200770).90 Inebilizumab was associated with a relapse-risk reduction of 73% during a period of 6 months. Despite the inclusion of patients with seropositive and seronegative AQP4-IgG, the clinical trial could not find benefits in the second subgroup, but it may be due to the small sample size (n=16). A descriptive study of these seronegative patients using inebilizumab showed an apparent decrease in ARR when compared with the placebo subgroup, but the results were not statistically significant.94 A long-term efficacy study supports the efficacy results reported in the initial study, in which 87.7% of patients who were AQP4-IgG positive continued inebilizumab and 83.4% of patients who switched from placebo to inebilizumab were relapse-free during the extension study.95
Ravulizumab is another monoclonal antibody recently approved for the treatment of patients with NMOSD. It is a humanized antibody that binds to the same complement component C5 epitope as eculizumab.96 The CHAMPION-NMOSD study (An Efficacy and Safety Study of Ravulizumab in Adult Participants With NMOSD, ClinicalTrials.gov identifier: NCT04201262) selected only patients with seropositive AQP4-IgG NMOSD to receive treatment with ravulizumab and compared them with the placebo control group from the PREVENT study. All patients with AQP4-IgG-positive NMOSD treated with the ravulizumab group were relapse-free compared with 20 patients in the PREVENT placebo group, in a median follow-up period of 73.5 weeks.97
Despite the lack of significant results for patients with seronegative AQP4-IgG NMOSD in these pivotal studies, some authors consider that, based on the known immunopathogenic mechanisms of NMOSD versus other autoimmune CNS diseases, treatments targeting specific mechanisms, such as complement inhibition, may be more restricted to AQP4-IgG-seropositive NMOSD.98 Previous studies that included patients who were AQP4-IgG seronegative are described in Table 1.86,89,90,93
Table 1: Monoclonal antibodies evaluated in patients with AQP4-IgG-seronegative NMOSD
| Study name | TANGO86 | N-MOmentum90 | SAkuraSky89 | SAkuraStar93 |
| Drug | TCZ versus AZA | Inebilizumab | Satralizumab | Satralizumab |
| Mechanism of action | TCZ is an anti-IL6 receptor; AZA prevents DNA replication | Anti-CD19 | Anti-IL6 receptor | Anti-IL6 receptor |
| Dose | TCZ: 8 mg/kg IV 4/4 weeks AZA: 2 to 3 mg/kg/day oral | 300 mg IV 2 weeks apart; then 6/6 months | 120 mg SC on weeks 0, 2 and 4; then 4/4 weeks | 120 mg SC on weeks 0, 2 and 4; then 4/4 weeks |
| AQP4-IgG status | TCZ: 85% AQP4-IgG+ AZA: 90% AQP4-IgG+ | 93% AQP4-IgG+ | 70% AQP4-IgG+ | 70% AQP4-IgG+ |
| Total relapse rate | TCZ: 8/59 (14%) AZA: 28/59 (47%) | Inebilizumab: 21/174 (12%) Placebo: 22/56 (39%) | Satralizumab: 8/41 (20%) Placebo: 18/42 (43%) | Satralizumab: 19/63 (30%) Placebo: 16/32 (50%) |
| Relapse rate in patients who were AQP4-IgG- | TCZ: 2/9 (22%) AZA: 3/6 (50%) | Inebilizumab: 3/17 (17%) Placebo: 0/4 | Satralizumab: 5/14 (36%) Placebo: 6/14 (43%) | Satralizumab: 10/22 (46%) Placebo: 3/9 (33%) |
| Total relapse-free at 96 weeks | Not applicable | Not applicable | Satralizumab: 78% Placebo: 59% | Satralizumab: 72% Placebo: 51% |
AQP4-IgG = aquaporin-4-immunoglobulin G;AQP4-IgG+ = aquaporin-4-immunoglobulin G positive;AQP4-IgG- = aquaporin-4-immunoglobulin G negative;AZA = azathioprine;IL = interleukin;IV = intravenous;NMOSD = neuromyelitis optica spectrum disorder;SC = subcutaneous;TCZ = tocilizumab.
With regard to future perspectives, an anti-CD20 monoclonal antibody, ublituximab, is being evaluated in combination with IVMP for the acute management of ON and myelitis attacks. A preliminary phase I study showed a reduction in disability status over a period of 90 days.99 Bortezomib, a 26S proteasome inhibitor approved for haematological neoplasms, was related to a relapse-free period of 12 months for four out of five patients with NMOSD and a decrease in AQP4-IgG levels.100 Aquaporumab, a recombinant human monoclonal antibody against AQP4, was effective in reducing NMOSD lesions in in vitro models.101 In addition, stem cell-based therapies are being investigated. An open-label cohort study, which included 11 patients with seropositive and one patient with seronegative AQP4-IgG, showed a relapse-free period of 5 years in 80% of patients, improvement in disability and seroconversion of patients from positive AQP4-IgG to negative.102 Most recently, a meta-analysis involving 31 patients with NMOSD demonstrated that 76% of the participants were attack-free during the evaluation period with stem cells.103
Prognosis
NMOSD is characterized by an accumulation of attack-related disability in visual, motor, sensory and autonomic dysfunction. The attacks are characterized by a new or worsening of neurological symptoms over days with frequent partial recovery despite treatments. Despite this characteristic, the early initiation of acute and preventive treatment has improved the long-term outcomes in patients with NMOSD. There is no clear progressive phenotype for NMOSD as seen in patients with MS.104
NMOSD prognosis is predicted by factors such as the age of symptom onset, number of attacks during the first 2 years, first attack severity, association with other autoimmune pathologies and serology status of AQP-IgG.105–108 Previous studies showed a lower rate of recovery of visual attacks in patients with seropositive AQP4-IgG when compared with patients who were seronegative.109,110 A prospective study of 29 patients presenting with isolated LETM found that 55% of the patients seropositive for AQP4-IgG relapsed within 1 year, while none of the patients who were seronegative relapsed.111 It is important to mention that there are differences in the technique of antibody detection (CBA versus enzyme-linked immunosorbent assay) and a mixture of patients with seropositive and seronegative AQP4-IgG, with the last group having some MOGAD cases.
Conclusions
In conclusion, seronegative NMOSD is a challenging diagnosis. It requires the exclusion of an extensive list of alternative diagnoses, and additional clinical and MRI features are required by the current NMOSD diagnostic criteria. Despite the limitations of current studies in patients with seronegative NMOSD, therapeutic response for new drugs appears to be less clear compared with AQP4-IgG-positive NMOSD, indicating that a possible distinct disease mechanism (not related to AQP4 or AQP4-IgG) may be associated with those patients. Further research is required to discover other biomarkers and new treatments for this orphan group of patients.